Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957versión On-line ISSN 2500-7440
Rev Col Gastroenterol v.27 n.2 Bogotá abr./jun. 2012
Intramural esophageal hematoma: Dissection of the perforation
Martin Gómez Zuleta, MD (1), Álvaro Rodríguez Gómez, MD (2), Amaranto Siado, MD (3)
(1) Assistant Professor in the Gastroenterology Unit of the Department of Internal Medicine at the Universidad Nacional de Colombia and Hospital El Tunal in Bogotá, Colombia.
(2) Gastroenterology Resident at the Universidad Nacional De Colombia in Bogotá, Colombia.
(3) Gastroenterologist at the Hospital El Tunal in Bogotá, Colombia
Received: 03-04-12 Accepted: 15-05-12
Abstract
Intramural esophageal hematomas are rare with few cases reported in the literature. Risk factors that affect the incidence of this condition include nausea and vomiting, but its most common clinical presentation is the triad of hematemesis, dysphagia and chest pain. Conservative treatment is best in most cases. We present our experience in 7 cases collected during the last 8 years in which you can see the entire spectrum of the disease from submucosal dissection to perforation of the esophagus.
Key words
Perforation, esophageal dissection, esophageal hematoma.
INTRODUCTION
Intramural esophageal hematomas occur infrequently and are characterized by hemorrhaging or bleeding contained between the mucosa and the muscular layers of the esophagus. This condition can lead to dissection and perforation of the submucosa and usually appears to be due to a sudden increase of intrathoracic pressure after situations such as trauma, vomiting, coughing and retching (1). Risk factors such as esophageal varices, esophageal ulcers and coagulopathy also favor this condition. Its most frequent clinical appearance is the triad of hematemesis, dysphagia and chest pain (2, 3). Intramural esophageal hematomas can be diagnosed radiologically, but need upper endoscopy for confirmation (4-6). This condition's development is often benign with treatment limited to clinical observation. Nonetheless, when there are complications like esophageal perforation, severe bleeding, or obstruction of the esophagus and the airways, endoscopic intervention or surgery become necessary (7).
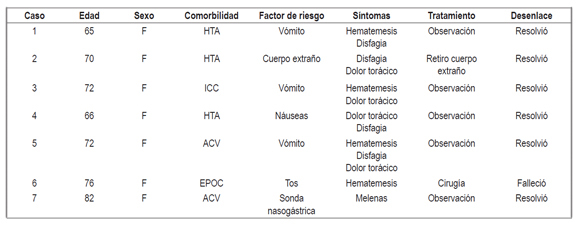
In this article we review our experience in 7 cases recorded from among the approximately 40,000 endoscopies done from 2002 to 2011. These cases cover several endoscopic diagnoses including hematoma, dissection and perforation of the mucosa (See Table 1).
Table 1. 7 cases recorded over a 9 year period.
CASE PRESENTATION
Case 1
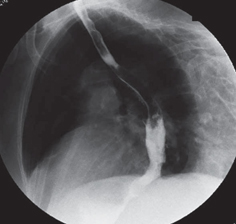
A 65-year-old female patient with a history of high blood pressure was admitted after two days of emetic episodes related to food contents followed by hematemesis with no hemodynamic stability. Upper endoscopy showed a hematoma in the proximal third of esophagus toward the right wall. The hematoma dried the mucosa and extended into the distal third of the esophagus (Figure 1). Patient was treatment by eliminating oral feeding and was observed. Endoscopic follow-up 48 hours later showed improvement of the hematoma and healing of the mucosa (Figure 2). The patient recovered successfully and was discharged after three days.
Figure 1. Hematoma and dissection of the right wall of the esophagus.
Figure 2. Healing of esophageal mucosa.
Case 2
A 70-year-old female patient with a history of heart failure was admitted following 2 days in which she felt dysphagia, chest pain and the presence of a foreign body at the hypopharynx. Upper endoscopy showed a chicken bone in the proximal esophagus and hematoma on the right esophageal wall. The foreign object was removed successfully through the mouth followed by observation of the patient who evolved without complications. She was discharged on the third day.
Case 3
A 72-year old female patient with a history of heart failure was admitted after eight days of chest pain and hematemesis. Upper endoscopy performed after admission showed dissection of the mucosa in the middle third of the esophagus toward the right wall extending into the distal third of the esophagus. To avoid any confusion and rule out the possibility of a tumor, biopsies were taken. They were negative for any malignancy. Patient was observed and progressed favorably.
Case 4
A 66-year-old female patient with a history of high blood pressure was admitted following 2 days of chest pain, dysphagia and melena. Upper endoscopy showed longitudinal tearing of the mucosa from the proximal third of the esophagus toward the right wall all the way to the distal third. Patient was observed, progressed satisfactorily, and was discharged on the third day.
Case 5
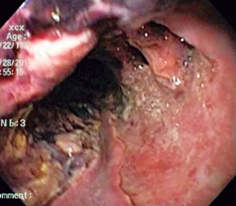
A 72-year-old female patient with an old stroke noted in her medical history was admitted following several emetic episodes the day before which had been followed by hematemesis and anemia. Upper endoscopy showed dissection of the sub mucosa in the proximal third of the esophagus toward the right wall (Figure 3). A large hematoma could also be observed extending from the middle third of the esophagus toward the left wall. It dried the wall all the way to the distal third (Figure 4). The patient was hospitalized and esophagography ruled out perforation (Figure 5). Endoscopic follow-up 48 hours later showed drainage of the hematoma in the light of the esophagus and submucosa dissection (Figure 6). The patient's symptoms resolved, she progressed successfully, and she was discharged on the fourth day.
Figure 3. Submucosa dissection of the esophagus.
Figure 4. Hematoma and esophageal submucosa dissection.
Figure 5. Esophagography ruling out perforation.
Figure 6. Partially resolved hematoma and submucosa dissection.
Case 6
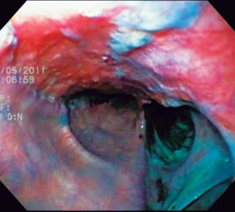
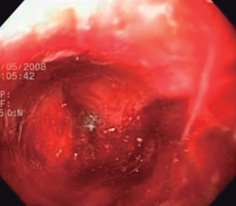
A 76-year-old female patient with a history of chronic obstructive pulmonary disease (COPD) was admitted following 3 days of coughing and dyspnea. She was taken to the ICU after suffering hypoxemic respiratory failure and a massive right pleural effusion. A thoracotomy was performed. 24 hours later the patient presented hematemesis. Upper endoscopy was performed and showed a large perforation with necrotic tissue in the middle third of the esophagus towards the right wall (Figure 7). Patient was surgically treated but died the next day.
Figure 7. Esophageal perforation.
Case 7
An 82-year-old female patient who had been hospitalized due to a stroke and who was being fed through a nasogastric tube presented melena and bloody drainage through the catheter. An upper endoscopy showed multiple blood clots from the distal third of the esophagus that prevented evaluation of the mucosa. The feeding tube was removed and the patient placed under observation. Endoscopic follow-up a week later showed mucosal dissection from the middle third of the esophagus toward the back wall extending all the way to the distal third of the esophagus but with complete resolution of hematoma. The patient progressed satisfactorily (Figure 8).
Figure 8. Dissection of entire submucosa of the stomach forming a bulge that prevented passage of endoscope.
DISCUSSION
Since the 1957 description of intramural esophageal hematoma by Williams, this condition has continued to be a diagnostic challenge ever since. Not only is it infrequent case, but it has been known only from series of cases like case 8 presented above.
The esophagus is an organ which is prone to lesions caused by external mechanisms such as foreign bodies, oral tracheal intubation, nasogastric catheters and endoscopic interventions including dilatations and hemostatic therapy. The esophagus is also affected by internal mechanisms including gagging, vomiting and coughing. Risk factors such as esophageal ulcers, esophageal varicose vein sclerosis, hemophilia and coagulopathy have been associated with intramural esophageal hematomas (9-11). In our work, intrinsic mechanisms were seen more frequently than were extrinsic ones while the most frequent comorbidities were high blood pressure and strokes (in contrast to the records in different sets of cases).
Medical manifestations such as chest pain, dysphagia and hematemesis were present in a third of the patients (12). In our set, dysphagia and chest pain prevailed in 57% of the patients. There was only one case in which the patient presented the clinical triad reported in the medical literature. Consequently, differential diagnoses were necessary to rule out other possible diagnoses including like aortic dissection, acute myocardial infarction, and pulmonary thromboembolism (13).
Diagnosis is usually done through upper endoscopy, but when there is the possibility of perforation, thoracic x-rays, esophagography, CT scans and MRIs are used instead (14, 15). All of our cases were diagnosed through endoscopy although when the endoscopy raised a suspicion of perforation esophagography was performed which ruled perforation out.
Despite the growing use of radiological studies for diagnosis of esophageal hematoma, we consider upper endoscopy to be more precise and detailed. In addition, it offers immediate therapeutic alternatives in case of complications like endoscopic decompression due to esophageal obstruction.
The evolution of esophageal hematoma is usually benign, and most patients recuperate spontaneously with conservative treatment. Consequently, routine endoscopic follow-ups are not recommended (16-18). The patients presented above all progressed in similar fashions except for the one case in which surgery was required to treat a perforation. The outcome of that case was fatal. In the other cases endoscopic follow-ups were performed without obtaining any changes in the course of the disease. This suggests that follow-up endoscopy is not necessary as long as clinical assessment indicates favorable progress.
We can conclude that intramural esophageal hematoma is not frequent, occurs predominantly among women, and can be suspected clinically but must be confirmed endoscopically. Treatment should be conservative in most cases, and its most frequent complications are submucosal dissection and perforation.
REFERENCES
1. Cullen SN, McIntyre AS. Dissecting intramural haematoma of the oesophagus. Eur J Gastroenterol Hepatol 2000; 12(10): 1151-62.
2. Mosimann F, Brönnimann B. Intramural haematoma of the oesophagus complicating sclerotherapy for varices. Gut 1994; 35(1): 130-1.
3. Hanson JM, Neilson D, Pettit SH. Intramural oesophageal dissection. Thorax 1991; 46(7): 524-7.
4. Lowman RK, Goldman R, Stern H. The roentgen aspects of intramural dissection of the esophagus. Radiology 1969; 93(6): 1329-31.
5. Demos TC, Okrendt DH, Studlo JD, Flisak ME. Spontaneous oesophageal haematoma diagnosed by computed tomography. J Comput Assist Tomogr 1986; 10(1): 133-5.
6. Atefi D, Horney JT, Eaton SB, Shulman M, Whaley W, Galambos JT. Spontaneous intramural haematoma of the esophagus. Gastrointest Endosc 1978; 24(4): 172-4.
7. Shim J, Jang JY, Hwangbo Y, Dong SH, Oh JH, Kim HJ, et al. Recurrent massive bleeding due to dissecting intramural hematoma of the esophagus: treatment with therapeutic angiography. World J Gastroenterol 2009; 15(41): 5232-5.
8. Williams B. Case report; oesophageal laceration following remote trauma. Br J Radiol 1957; 30(360): 666-8.
9. Bradley JL, Han SY. Intramural haematoma (incomplete perforation) of the esophagus associated with esophageal dilatation. Radiology 1979; 130(1): 59-62.
10. Tong M, Hung WK, Law S, Wong KH, Kwok KF, Wong J. Esophageal hematoma. Dis Esophagus 2006; 19(3): 200-2.
11. Low DE, Patterson DJ. Complete esophageal obstruction secondary to dissecting intramural hematoma after endoscopic variceal sclerotherapy. Am J Gastroenterol 1988; 83(4): 435-8.
12. Gluck M, Jiranek GC, Low DE, Kozarek RA. Spontaneous intramural rupture of the esophagus: clinical presentation and endoscopic findings. Gastrointest Endosc 2002; 56(1): 134-6.
13. Ho CL, Young TH, Yu CY, Chao YC. Intramural hematoma of the esophagus: ED diagnosis and treatment. Am J Emerg Med 1997; 15(3): 322-3.
14. Jung KW, Lee OJ. Extensive spontaneous submucosal dissection of the esophagus: Long-term sequential endoscopic observation and treatment. Gastrointest Endosc 2002; 55(2): 262-5.
15. Yuen EH, Yang WT, Lam WW, Kew J, Metreweli C. Spontaneous intramural haematoma of the oesophagus: CT and MRI appearances. Australas Radiol 1998; 42(2): 139-42.
16. Steadman C, Kerlin P, Crimmins F, Bell J, Robinson D, Dorrington L, et al. Spontaneous intramural rupture of the oesophagus. Gut 1990, 31(8): 845-9.
17. Singh A, Papper M. Extensive intramural esophageal dissection: an unusual endoscopic complication. Gastrointest Endosc. 2012; 75(1): 186-7.
18. Barone JE, Robilotti JG, Comer JV. Conservative treatment of spontaneous intramural perforation (or intramural haematoma) of the oesophagus. Am J Gastroenterol 1980; 74(2): 165-7.
1. Cullen SN, McIntyre AS. Dissecting intramural haematoma of the oesophagus. Eur J Gastroenterol Hepatol 2000; 12(10): 1151-62. [ Links ]
2. Mosimann F, Brönnimann B. Intramural haematoma of the oesophagus complicating sclerotherapy for varices. Gut 1994; 35(1): 130-1. [ Links ]
3. Hanson JM, Neilson D, Pettit SH. Intramural oesophageal dissection. Thorax 1991; 46(7): 524-7. [ Links ]
4. Lowman RK, Goldman R, Stern H. The roentgen aspects of intramural dissection of the esophagus. Radiology 1969; 93(6): 1329-31. [ Links ]
5. Demos TC, Okrendt DH, Studlo JD, Flisak ME. Spontaneous oesophageal haematoma diagnosed by computed tomography. J Comput Assist Tomogr 1986; 10(1): 133-5. [ Links ]
6. Atefi D, Horney JT, Eaton SB, Shulman M, Whaley W, Galambos JT. Spontaneous intramural haematoma of the esophagus. Gastrointest Endosc 1978; 24(4): 172-4. [ Links ]
7. Shim J, Jang JY, Hwangbo Y, Dong SH, Oh JH, Kim HJ, et al. Recurrent massive bleeding due to dissecting intramural hematoma of the esophagus: treatment with therapeutic angiography. World J Gastroenterol 2009; 15(41): 5232-5. [ Links ]
8. Williams B. Case report; oesophageal laceration following remote trauma. Br J Radiol 1957; 30(360): 666-8. [ Links ]
9. Bradley JL, Han SY. Intramural haematoma (incomplete perforation) of the esophagus associated with esophageal dilatation. Radiology 1979; 130(1):59-62. [ Links ]
10. Tong M, Hung WK, Law S, Wong KH, Kwok KF, Wong J. Esophageal hematoma. Dis Esophagus 2006; 19(3): 200-2. [ Links ]
11. Low DE, Patterson DJ. Complete esophageal obstruction secondary to dissecting intramural hematoma after endoscopic variceal sclerotherapy. Am J Gastroenterol 1988; 83(4): 435-8. [ Links ]
12. Gluck M, Jiranek GC, Low DE, Kozarek RA. Spontaneous intramural rupture of the esophagus: clinical presentation and endoscopic findings. Gastrointest Endosc 2002; 56(1): 134-6. [ Links ]
13. Ho CL, Young TH, Yu CY, Chao YC. Intramural hematoma of the esophagus: ED diagnosis and treatment. Am J Emerg Med 1997; 15(3): 322-3. [ Links ]
14. Jung KW, Lee OJ. Extensive spontaneous submucosal dissection of the esophagus: Long-term sequential endoscopic observation and treatment. Gastrointest Endosc 2002; 55(2): 262-5. [ Links ]
15. Yuen EH, Yang WT, Lam WW, Kew J, Metreweli C. Spontaneous intramural haematoma of the oesophagus: CT and MRI appearances. Australas Radiol 1998; 42(2): 139-42. [ Links ]
16. Steadman C, Kerlin P, Crimmins F, Bell J, Robinson D, Dorrington L, et al. Spontaneous intramural rupture of the oesophagus. Gut 1990, 31(8):845-9. [ Links ]
17. Singh A, Papper M. Extensive intramural esophageal dissection: an unusual endoscopic complication. Gastrointest Endosc. 2012; 75(1): 186-7. [ Links ]
18. Barone JE, Robilotti JG, Comer JV. Conservative treatment of spontaneous intramural perforation (or intramural haematoma) of the oesophagus. Am J Gastroenterol 1980; 74(2): 165-7. [ Links ]











 texto en
texto en