Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.27 no.3 Bogotá July/Sept. 2012
Endoscopic management of biliary complications following orthotopic liver transplantation
Rodrigo Castaño Llano, MD.(1), Mario H. Ruiz Vélez, MD. (2), Juan Carlos Restrepo Gutiérrez, MD. (1), Sergio I. Hoyos Duque MD. (1), Carlos E. Guzmán Luna MD.(3), Álvaro Mena Hurtado, MD.(3), Octavio Muñoz Maya, MD. (4), Juan Ignacio Marín, MD.(4), Vanessa García, MD.(5), Gonzalo Correa Arango, MD.(6)
(1) Gastro-hepatology Group at the Universidad de Antioquia and Hospital Pablo Tobón Uribe in Medellín, Colombia.
(2) General Surgery and Endoscopy at the Hospital Pablo Tobón Uribe in Medellín, Colombia.
(3) Liver Transplant Surgery at the Hospital Pablo Tobón Uribe in Medellín, Colombia.
(4) Internal Medicine and Hepatology at the Hospital Pablo Tobón Uribe in Medellín, Colombia.
(5) Radiology Specialist Corporal Imaging and Professor at the Universidad de Antioquia and the Hospital Pablo Tobón Uribe in Medellín, Colombia.
(6) Gastro-hepatology Group at the Universidad de Antioquia and Chief of the Hepatic Transplant Group at the Hospital Pablo Tobón Uribe in Medellín, Colombia.
Received: 18-01-12 Accepted: 17-08-12
Abstract
Background. Complications of bile duct reconstruction following liver transplantation are common and are an important cause of morbidity and mortality. Currently, endoscopic retrograde cholangiopancreatography (ERCP) is an attractive alternative for management of biliary complications. It has high diagnostic and therapeutic utility, is less invasive than other techniques and has low morbidity. The aims of this study are to evaluate the results of endoscopic management of patients with biliary complications following liver transplantation, and to then determine risk factors and their impacts on patient survival.
Materials. We reviewed the medical records of patients with biliary complications following liver transplantation who were admitted to the Hospital Pablo Tobón Uribe between January 2002 and December 2010. Cases were reviewed whether or not patients had undergone transplantation at this center.
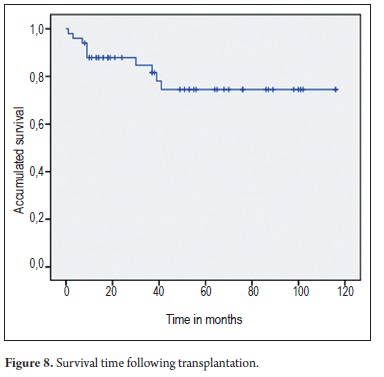
Results. 148 ERCPs were performed on 50 patients (30 men and 20 women). Average patient age was 47 years (5 to 71 years old). Average follow up time was 44 months. 42 biliary strictures in (33 anastomotic and 9 non anastomotic), 4 fistulas, 3 filling defects (stones or bile casts) and 1 papillary stenosis (Oddi dysfunction) were found. Strictures were managed with plastic (30 patients) prostheses or, since 2008, with metal prostheses (12 patients). 94% of cases of non-ischemic stenosis improved with biliary stents. There were no significant differences in outcomes between plastic and metal prostheses, but there was a significant reduction in the number of ERCPs needed in the metal stent group (84 versus 28). Fistulas were closed with plastic stents in three of the four patients. Three patients had stones that were successfully removed. One patient with papillary stenosis improved after sphincterotomy. Complications occurred in 8 patients: four cases of bleeding (all controlled endoscopically), three cases of mild pancreatitis, and one patient with sepsis that recovered with antibiotic treatment. Multivariate analysis showed a significant association of anastomotic strictures with patient age (p = 0.002). The overall survival analysis showed that the probability of survival for 40 months after liver transplantation is 0.745. There were no differences among transplant patients without biliary complications.
Conclusions. Endoscopic cholangiography is safe and effective for the diagnosis and management of biliary complications following hepatic transplantation. The only factor which showed a direct relationship with the possibility of biliary complications was age. The survival of the group with biliary complications did not differ from transplant patients without biliary complications.
Key words
Liver transplantation, biliary stent, biliary stricture, biliary fistula, biliary drainage.
INTRODUCTION
Orthotopic liver transplant (OLT) is the only therapeutic alternative available for improving the survival and quality of life for patients with advanced chronic liver disease and for those with acute liver failure and poor prognoses. Ever since the first description of OLT by Tomas Starzl (1) in 1963 there have been significant advances in areas such as organ selection, explant, preservation solutions, implantation techniques and immunosuppression. Complications derived from the reconstruction of the bile duct are described in between 5% and 25% of the series and are considered, even today, the Achilles heel of OLT (2). Initially, mortality secondary to biliary complications was 30% (3). Today it does not go over 10% to 15% (4). However, morbidity - predominantly infectious complications - is still relevant. Its incidence varies between 10% and 30% (5, 6). These high rates of post OLT biliary complications point to the inherently greater sensitivity of the biliary epithelium to ischemia compared with the sensitivities of hepatocytes and the vascular endothelium (7).
Stenosis and biliary fistulas are the most frequent complications, but biliary lithiasis and dysfunctions of the sphincter of Oddi are also common. These may appear at any stage of transplantation, and clinical diagnosis is frequently confused with other infectious or immunological complications proper to the transplant itself (2, 8).
Biliary complications have become increasingly common with improved survival of transplant patients. These biliary complications not only affect survival of the organ, but have great impacts on the transplant patients quality of life through repeated hospitalizations, interventions and emotional trauma to which patients and their families may be subject to. In addition, they have an impact on the cost (9).
Despite improvements in surgical techniques and perioperative care for transplant patients, biliary complications are a therapeutic challenge for transplantation teams. In the past, surgical intervention was considered the first option for management of patients with biliary complications after an OLT (10), but recent papers point to endoscopic treatment for endoscopic retrograde cholangiography (ERCP) as an attractive alternative for treating these patients. It is less invasive, has a greater diagnostic and therapeutic utility and has low mortality rates when used in medical centers with this specialty (11-13).
The objective of this study was to evaluate the results of endoscopic management in a series of patients who presented biliary complications after OLTs at referral centers in Medellin, Colombia. It is intended to evaluate potential risk factors and treatment results as well as to determine impact on patient and graft survival.
MATERIALS AND METHODS
Information regarding endoscopic management of biliary complications was obtained from the clinical records and a prospective database of all patients who entered the Hepatic Transplant Program of the Pablo Tobon Uribe Hospital between January 2002 and December 2010 whether or not the transplantation was performed at this center. As described in a recent publication, post OLT biliary complication rate was 9.84%. For this evaluation, 42 patients from the referral center and 8 patients from another hospital in the city, all with biliary complications, were managed by endoscopy by the authors.
General techniques
All the transplants were deceased-donor liver transplantation (DDLT). Custodial (HTK: Histidine-Tryptophan-Ketoglutarate) preservation solution was employed in all cases. The piggy back technique was used to join the suprahepatic vena cava of the donor liver to the recipient retrohepatic vena cava by anastomosis followed by anastomosis of the portal vein and graft reperfusion. This is followed by arterial anastomosis and finally biliary anastomosis. In principle a choledochoenterostomy is performed in every case. Polydioxanone (PDS) 6/0 sutures are used for continuous posterior stitching and separate anterior stitching. The T tube is never left in the bile duct. Three cavity drains are left, one is located on the right upper liver, another one on the right lower liver and another on the left lower liver.
A triple immunosuppression scheme is used without induction. It combines the use of steroids, azathioprine, and calcineurin inhibitors (most often cyclosporine). Steroids are usually discontinued after three months after transplantation. Mycophenolate mofetil is only employed in cases of renal dysfunction when dosages of calcineurin inhibitors are decreased or suspended completely in patients with severe rejection. Tacrolimus is indicated for pediatric patients, adults with recurrent rejection or histological indicators of poor prognoses.
Patient characteristics
Demographic characteristics of the donors and recipients and reason for liver transplant were determined. In addition, risk factors for biliary complications in OLTs were registered. They included donors age, hot and cold ischemia times, intrahepatic and perihepatic complications. Patients who presented any vascular complications were analyzed separately. No transplants were performed on patients with ABO incompatibility.
Indications for endoscopic retrograde cholangiopancreatography (ERCP)
A total of 148 endoscopic retrograde cholangiopancreatographies (ERCPs) were performed on 50 endoscopically managed patients. Indications for performance of an ERCP were cholestasis in the absence of cellular rejection as determined by clinical history (abdominal pain, fever), radiological findings (bilomas, fistulas, dilated ducts) or laboratory data showing a cholestatic pattern. Biliary fistula was suspected when excessive amounts of fluid flowed out of the Jackson-Pratt drain and when imaging indicated a biloma. These were also indications for ERCP. Patients with cholestasis without a clear cause but who were not in chronic or acute rejection also received ERCPs. Hepatic biopsies were performed to exclude rejection and recurrent cholestatic hepatitis C virus. ERCPs were postponed in cases of a biliary dilatation or the presence of gallstones due to the high risk of development of biliary fistulas. In cases in which ERCP was indicated, it was performed first. If cholestasis did not resolve, a hepatic biopsy was performed.
Technical aspects of ERCP
ERCP findings included biliary stenoses, fistulas and filling defects and papillary stenoses (dysfunction of the sphincter of Oddi). We recorded whether or not balloon dilation was used, whether plastic and/ or metallic stents were used, and whether there was a stenosis relapse during follow up.
Cannulation of the bile duct was done selectively. Contrast medium was injected with minimum pressure to avoid cholangio-venous reflux and potential sepsis. For patients without stenosis, fistulas or large gall stones, we tried to place stents without sphincterotomies. All patients received prophylactic antibiotics (sulbactam-ampicillin or ciprofloxacin) before ERCPs. The majority of these procedures (>80%) were performed under sedation. Complications such as pancreatitis, bleeding or sepsis were registered.
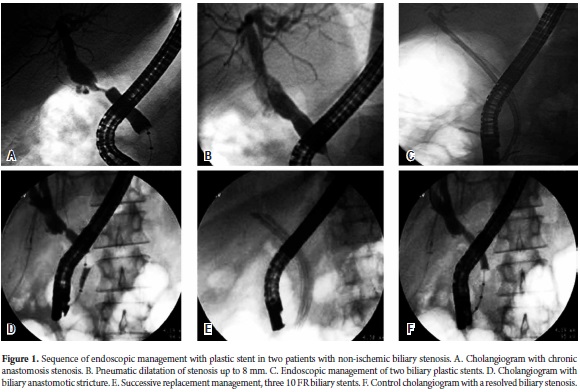
Non-ischemic stenoses were managed with pneumatic balloon dilation before placing plastic stents. Successive replacements throughout a year took place until at least three 10 FR stents had been placed. Since 2008 balloon dilation has not been used. Instead stenoses have been most frequently handled with partially covered self-expanding metallic stents (there were no completely covered stents available).
Ischemic stenosis was considered when there were multiple stenoses or a stenosis was at least 5mm of the anastomosis.
ERCP complications
ERCP complications were defined according to the criteria established by Cotton (14, 15). Pancreatitis, cholangitis, hemorrhaging and perforation were registered when they occurred. Adverse events were classified as mild when hospitalization was no longer than 3 days, moderate from 4 to 7 days and severe when hospitalization extended for more than a week. Fatal outcomes were evaluated when death was attributable to the procedure.
Evaluation of Treatment
Treatment responses were measured by ERCP which showed complete or almost complete resolution or almost complete of the stenosis. There is always a residual belt which does not require subsequent surgical or percutaneous intervention. The normalization of hepatic enzymes is not the final objective of therapy because many patients may have marginally increased enzymes for various reasons. The success of treatment for fistulas was defined as complete closure of the fistula without any symptoms or need for surgery. The closure of the fistula was confirmed during the ERCP when the stent was being removed. For patients with filling defects or papillary stenosis success was defined as the complete resolution of stones and improvement of symptoms.
Statistical analysis
Absolute and relative distributions as well as summary indicators (central tendency measurements, position and dispersion) were used for statistical analysis. The Chi squared independence test or Fishers Exact test was used to explore possible associations in the descriptive analysis. For survival analysis the Kaplan-Meier method was applied using the Breslow test (generalized Wilcoxon test) for comparing curves. Cox regression was used for the multivariate analysis; a p value of less than 0.05 was considered statistically significant. SPSS version 17 was used for data processing and analysis.
Ethical aspects
This investigation was classified according to the Helsinki international declaration, the Belmont report and Colombian Resolution 8430 of 1993 as an investigation with no biological, physiological, psychological or social risks. It also took into account resolution 1995 of 1999 which establishes the norms regarding medical record use.
RESULTS
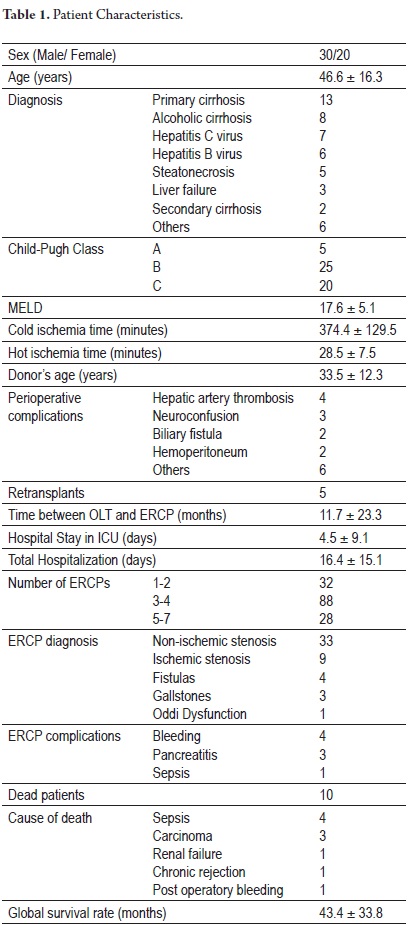
148 ERCPs were performed on 50 patients for diagnosis and management of biliary complications. The average age of these patients (20 men and 20 women) was 47 years (range 5 to 71 years of age). ERCPs did not resolve non-ischemic stenoses in 2 of 33 patients. The average time between the first transplant and the first ERCP was 11.6 months, while the minimum follow up time was 7 months and the average monitoring of the series was 44 months. Demographic characteristics and other study variables are shown in Table 1.
BILIARY STENOSIS
Out of 50 patients, 42 had biliary anastomotic stricture, out of which 33 were non/ischemic. Initially, the patients were dilated with a 6 to 8 mm pneumatic balloon (according to the severity of the stenosis) followed by the placement of a 10 FR plastic stent (Figure 1).
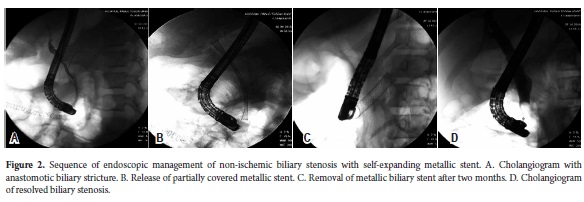
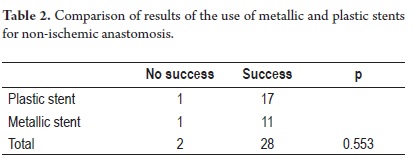
Results from balloon dilatation followed by stenting were similar to those from stent placement without pneumatic dilatation. Most recently, metallic stents have been used for 12 patients. They require less time for treating stenoses and were successful in eleven of the twelve patients (Figure 2 and Table 2).
Nevertheless, the 84 ERCPs were necessary for 21 patients with plastic stents while only 28 ERCPs were required for the 12 patients with metallic stents (p=0.002).
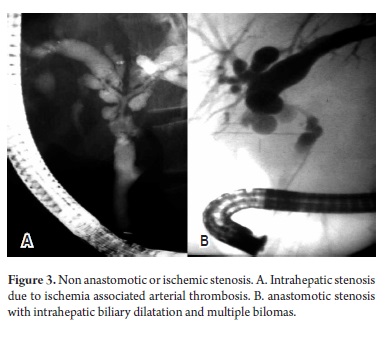
Nine patients presented ischemic stenoses. On average an ERCP was performed within the first six months following transplantation, except for one patient with a late arterial thrombosis. Four out of nine patients passed away less than a year after transplantation (1 to 9 months - Figure 3).
BILIARY FISTULAS
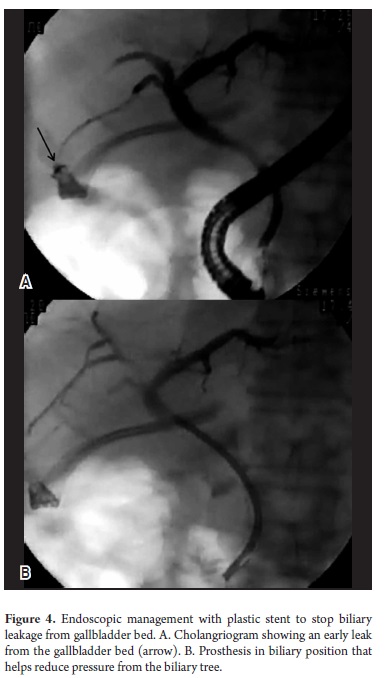
Four patients developed biliary fistulas: three anastomotic fistulas and one fistula located in the gallbladder bed. All developed early and were managed with 10 FR plastic stents. Three were resolved, but in one case stenting failed to stop anastomotic leakage produced by the fistula. Anastomotic ischemia was suspected and surgery was performed. On average patients required 2 ERCPs each. The second ERCP was performed 6 to 8 weeks after stent placement to remove the 10 FR stent and to verify closure (Figure 4).
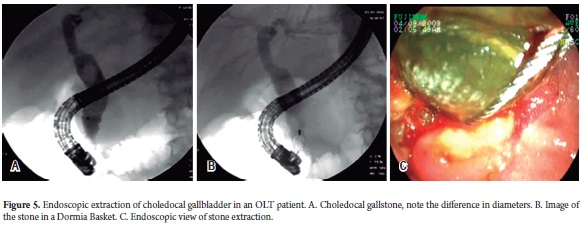
FILLING DEFECTS
Gallstones were removed from the bile ducts of three patients. One of them was associated with an anastomotic stenosis which was managed with a plastic stent. A patient presented a cast of gallstones, all which were successfully managed through sphincterotomy and gallstone extraction. The average number of ERCPs for this group was 1.6 (Figure 5).
SPHINCTER OF ODDI DYSFUNCTION
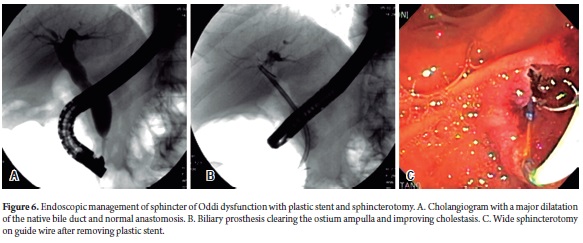
Even though sphincter of Oddi dysfunction is most frequently described in women, we found this problem in a male patient 54 months after OLT. The patient presented abdominal pain and a cholestatic pattern in laboratory tests. An ERCP found no evidence of anastomotic stenosis, but did find a large dilatation in the native bile duct (Figure 6).
ERCP COMPLICATIONS
There were eight complications for an incidence of 16%. Four patients experienced bleeding following sphincterotomies. They were treated endoscopically with sclerotherapy with adrenaline and argon plasma. Transfusions of two or three units of red blood cells were required for two of these patients. Mild pancreatitis, evidenced by increased blood amylase, was present in three patients. Patients were observed in a wait and see mode until complete recovery. There was one case of sepsis following a cholangiography. The Patient suffered hemodynamic repercussion due to shock which was managed with antibiotics in the ICU with a perfect recovery.
VASCULAR COMPLICATIONS
There were 4 perioperative thromboses of the hepatic artery, a late thrombosis of the hepatic artery (78 month post-OLT) and a thrombosis of the portal vein. Two of the perioperatory thromboses of the hepatic artery evolved into ischemia. One of them underwent a second operation, but both patients died. The patient with late thrombosis of the hepatic artery also had an ischemic stenosis which was resolved by dilatation and changing the plastic stent. The patient with portal vein thrombosis had an anastomotic stenosis which was resolved through the replacement of the plastic stent.
BILIARY COMPLICATION RISK FACTORS
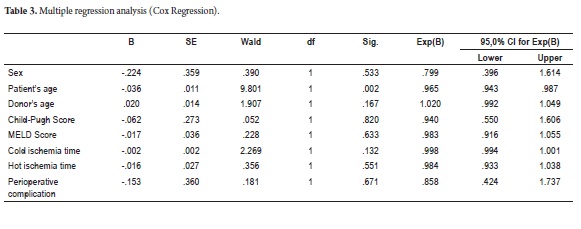
To determine variables implicated in anastomotic and non-anastomotic biliary complications a multivariate analysis was performed (Cox regression). That analysis evaluated the patients sexes and ages, donors ages, Child-Pugh scores, MELD scores, cold ischemia time, hot ischemia time and the presence of perioperative complications. The analysis found a significant association between anastomotic stenoses and patients ages (p=0.002) (Table 3).
SURVIVAL RATE
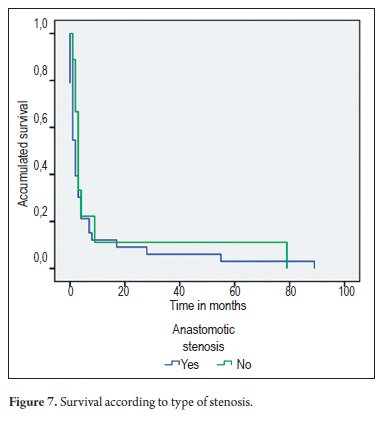
No significant differences were found between survival times among patients with anastomotic stenosis and those with non-anastomotic (ischemic) stenosis (p=0.163) (Figure 7).
An analysis of overall survival rates demonstrated that the probability of survival at 40 months after liver transplantation was 0.745. This rate was the same for patients who did not present biliary complications (Figure 8).
DISCUSSION
This study is the third in a series that has evaluated biliary complications following OLT. In the first study was an overall evaluation of a group of 254 OLT patients with OLT. It found an acceptable rate of biliary complications on the order of 9.8%. This is comparable to other large medical centers. A second study, now in press, compared ERCP, the gold standard for evaluation of biliary complications, with ultrasound and magnetic resonance cholangiopancreatography (MRCP). It found poor positive predictive sensitivity for ultrasound (55.6% to 93.7%), but better positive predictive sensitivity for MRCP (80% to 92.3%).
The management of bile duct complications in OLT patients has taken a turn toward avoidance of repeated surgical interventions and avoidance of the percutaneous approach in favor of less invasive interventions such as ERCP. ERCP results in minimal morbidity and, as shown in our series, is without mortality. (16)
In conformity with other series (5, 9, 17)the most frequently managed complication was anastomotic or non-ischemic stenosis which accounted for 66% of the complications in this study. These stenoses had a 94% response rate with endoscopic management. Only two out of 31 patients showed no improvement. Stenoses appearing in the first year following OLT can be managed for 6 months through stent changes. Those that appear more than a year after transplantation require stent changes every 1 to 2 years (18). These patients were treated in two different ways. Before 2008 balloon dilatation was combined with successive changes of plastic stents. More recently, it has been found that dilatation alone without stenting is sufficient for managing stenoses which are not complex (ischemic) (19).
From 2008 balloon dilatation has been abandoned in favor of direct placement of a partially covered self-expanding metallic stent because dilatation led to migration of the covered stent (todays totally covered stents were not available). Dilation also increased costs and duration of procedures and added to morbidity by increasing the need to perform sphincterotomies in order to release balloons. Of the 12 patients managed with metallic stents, eleven overcame stenoses and stents were removed 6 to 8 weeks after being placed. One patient from another city had her stent removed after 11 months without problems.
Stenoses which are ischemic, non-anastomotic or proximal to an anastomosis are harder to manage endoscopically. These difficulties are related to arterial liabilities such as hepatic arterial thrombosis, cold ischemia time, longer organ preservation of over 10 hours and ABO incompatibility. Ischemic stenoses generally compromise the hepatic hilum and have multiple presentations which compromise the intrahepatic ducts (Figure 3). The gallstone molds form frequently in these patients and they must be managed with balloon dilatation and successive stent replacements. On average, they require a greater number of ERCPs and have lower response rates than do patients with non-ischemic stenoses. Nevertheless, it has been proven that the endoscopic treatment of these patients does not affect future reconstructive surgery (20). It is recommended that endoscopic management be exhausted before percutaneous surgery is attempted for these patients. Recently, reliable success of intrahepatic biliary dilatation with ERCP has been described (21). Exceptions are patients with compromised hepatic confluence extending to the right and left liver. For these patients percutaneous intervention may be more advantageous. Long term monitoring of these patients must be short because the possibility of stenotic relapse is high even several years after successful intervention (22).
ERCP generally locates biliary fistulas even in cases where a suspected fistula cannot be located after repeated use of contrast imaging. In an immunosuppressed patient, it is recommended that the stent be left in. the probability of fistula improvement is 95%. In our series there were no fistulas associated with T tube removal. The four that were related were early fistulas. In the case of a T tube fistula, it is recommended that the stent be placed parallel to the T tube. It should be either removed immediately or after a day or two. Both approaches are safe. Most patients require only two ERCPs, one to place the stent and one to remove it. These differ from post cholecystectomy fistulas, which are resolved early. In the case of OLT these fistulas may have take longer to close due to immunosuppression. For this reason it is recommended that removal wait two to three months. This wait is justified by the frequent development of late fistulas after removal of the T tube. Other series have looked at the use of nasal-biliary drains (23), but the discomfort they involve, the high rate of self-removal and longer hospital stays have led even those authors to recommend immediate surgery (10). Currently, the recommended approach is endoscopic, reserving surgery for when the endoscopic approach has failed. Results with management of biliary stenosis with metallic stents have generally been favorable, with some groups favoring them (24-32), and other groups criticizing them (33).
As we have mentioned in our series, in 50% of these cases the presence of biliary stones is associated with stenosis. We recommend dilating the stenosis before removing the gallstone. Differential diagnosis includes checking for the presence of clots and biliary molds. Biliary molds are related to diffuse ischemic hilum stenoses (34). Even though endoscopic intervention may be attempted, the long term prognosis is poor because of the frequent infections and hepatic abscesses so this condition is commonly approached percutaneously. In general, bile duct compromise from several stenoses and hepatic artery thrombosis must be approached by a quick retransplant.
Sphincter of Oddi dysfunction following OLT has been described in from 3% to 7% of cases and is a late complication (2, 22). The diagnosis is based on dilation of the native bile duct associated with increased hepatic enzymes, with improvement after the sphincterotomy. In these patients sphincter manometry is not justified.
Our series had fewer biliary complications than other series discussed here. One of the reasons is that T tubes were not used when the surgeon reconstructed bile ducts. A randomized study has shown that T tubes were associated with five times more frequent complications (35). Choledocal-choledocal reconstruction allows an endoscopic approach to the bile duct and is recommended even for OLTs with a live donor which has a greater incidence of biliary complications (36, 37).
A reasonable rate of complications after ERCP of 16% was found in this study. Bleeding following sphincterotomy predominated (8%), occurring in four patients two of whom required transfusions. Acute pancreatitis (6%) was not as frequent as in other series where they have been described as occurring more frequently than in neoplastic ERCPs (38). Although sepsis did develop following one ERCP this does not necessarily imply that the procedure induced morbidity. Since the sepsis was resolved by a stay in the ICU with antibiotics intervention the procedure can be described as safe and effective (13).
Vascular and biliary complications which occurred included four biliary thromboses, two anastomotic stenoses and one non-anastomotic stenosis. One patient required a retransplant and passed away due to massive post-op bleeding. An association between arterial vascular complications and biliary stenosis is recognized (39).
The multivariate analysis (Cox regression) showed a significant relation between the presentation time of stenosis and age. Different series have described other associations such as the use of a T tube and the level of pre-op bilirubin (40, 41). Another study describes cold ischemia time and the presence of cirrhosis prior to OLT (42), while another discusses male sex and insert rejection (43).
More recently the administration of Sorafenib (tyrosine-kinase inhibitor) to prevent progression of hepatocellular carcinoma in OLT waiting list patients has been described as increasing the possibility of biliary complications and acute rejection (44). On the other hand, Sirolimus (mTOR inhibitor), due to its negative effects on collagen and colangiocite regeneration, has also been implicated as an inducer of biliary complications in these patients (45). The habit of smoking was not evaluated, which has also been implicated in vascular and biliary complications in OLT patients (46, 47).
Based on the study previously mentioned, biliary complications did not have an impact on grafts or patients, a case that has already been mentioned in other publications (48). In our series, only diffuse stenoses with hilum compromise negatively impacted the survival of the graft and the patient, as has been widely reported (49). Success in the management of these patients is based on an interdisciplinary focus with the concurrence of hepatologists, endoscopists, transplant surgeons and interventional radiologists.
Many questions arise when reviewing the data presented here and in other series regarding management of biliary complications through endoscopy. There is no unified protocol for endoscopic management of these patients that determines the number of cholangiographies, their time sequence, whether to use metallic or plastic stents, the period between plastic stent changes, or when protocols should be changed or even when they have failed. These questions will only be solved with randomized studies with a great number of patients.
CONCLUSIONS
Endoscopic cholangiography is a safe and effective intervention for the diagnosis and management of biliary complications secondary to OLT. It obviates the necessity of more invasive interventions such as percutaneous intervention or surgery which have higher rates of morbidity and mortality. These approaches must be reserved for cases where endoscopic management has failed. Only age showed a direct relation to the possibility of biliary complications. The survival rate of the group of patients with biliary complications does not differ from the survival rate of transplanted patients who did not have biliary complications.
Conflict of interests
The authors declare that they have no conflicts of interests.
REFERENCES
1. Starzl TE, Marchioro TL, Vonkaulla KN, Hermann G, Brittain RS, Waddell WR. Homotransplantation of the Liver in Humans. Surgery, gynecology & obstetrics 1963; 117: 659-76.
2. Balderramo D, Navasa M, Cardenas A. Current management of biliary complications after liver transplantation: emphasis on endoscopic therapy. Gastroenterol Hepatol 2011; 34: 107-15.
3. Starzl TE, Putnam CW, Hansbrough JF, Porter KA, Reid HA. Biliary complications after liver transplantation: with special reference to the biliary cast syndrome and techniques of secondary duct repair. Surgery 1977; 81: 212-21.
4. Muñoz OG, Insuasty MR, Marín JI, et al. Complicaciones de la vía biliar después de trasplante ortotópico de hígado: Experiencia en el Hospital Pablo Tobón Uribe - Medellín. Rev Col Gastroenterol 2011; 26: 9-14.
5. Yagci G, Cetiner S, Ersoz N, et al. The effect of gained experience on postoperative complications and mortality in cadaveric liver transplantation: a single-center experience. Transplant Proc 2011; 43: 912-6.
6. Vera A, Contreras F, Guevara F. Incidence and risk factors for infections after liver transplant: single-center experience at the University Hospital Fundacion Santa Fe de Bogotá, Colombia. Transplant infectious disease : an official journal of the Transplantation Society 2011.
7. Noack K, Bronk SF, Kato A, Gores GJ. The greater vulnerability of bile duct cells to reoxygenation injury than to anoxia. Implications for the pathogenesis of biliary strictures after liver transplantation. Transplantation 1993; 56: 495-500.
8. Krok KL, Cardenas A, Thuluvath PJ. Endoscopic management of biliary complications after liver transplantation. Clin Liver Dis 2010; 14: 359-71.
9. Ryu CH, Lee SK. Biliary strictures after liver transplantation. Gut Liver 2011; 5: 133-42.
10. Kuo PC, Lewis WD, Stokes K, Pleskow D, Simpson MA, Jenkins RL. A comparison of operation, endoscopic retrograde cholangiopancreatography, and percutaneous transhepatic cholangiography in biliary complications after hepatic transplantation. J Am Coll Surg 1994; 179: 177-81.
11. Londono MC, Balderramo D, Cardenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol 2008; 14: 493-7.
12. Williams ED, Draganov PV. Endoscopic management of biliary strictures after liver transplantation. World J Gastroenterol 2009; 15: 3725-33.
13. Sanna C, Giordanino C, Giono I, et al. Safety and efficacy of endoscopic retrograde cholangiopancreatography in patients with post-liver transplant biliary complications: results of a cohort study with long-term follow-up. Gut Liver 2011; 5: 328-34.
14. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991; 37: 383-93.
15. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 2010; 71: 446-54.
16. Morelli J, Mulcahy HE, Willner IR, Cunningham JT, Draganov P. Long-term outcomes for patients with post-liver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc 2003; 58: 374-9.
17. Krol R, Karkoszka H, Ziaja J, et al. Biliary complications after orthotopic liver transplantation: a 5-year experience. Transplant Proc 2011; 43: 3035-8.
18. Thuluvath PJ, Atassi T, Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int 2003; 23: 156-62.
19. Kulaksiz H, Weiss KH, Gotthardt D, et al. Is stenting necessary after balloon dilation of post-transplantation biliary strictures? Results of a prospective comparative study. Endoscopy 2008; 40: 746-51.
20. Davidson BR, Rai R, Nandy A, Doctor N, Burroughs A, Rolles K. Results of choledochojejunostomy in the treatment of biliary complications after liver transplantation in the era of nonsurgical therapies. Liver Transpl 2000; 6: 201-6.
21. Li QY, Qin YS, Ling Q, Yang FC, Zheng SS. No Therapeutic ERCP in Anastomotic Stricture without Intrahepatic Biliary Dilation after Liver Transplantation. Hepatogastroenterology 2011; 58: 1127-31.
22. Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy 2005; 37: 857-63.
23. Ostroff JW. Post-transplant biliary problems. Gastrointest Endosc Clin N Am 2001; 11: 163-83.
24. Traina M, Tarantino I, Barresi L, et al. Efficacy and safety of fully covered self-expandable metallic stents in biliary complications after liver transplantation: a preliminary study. Liver transplantation : official publication of the American Association for the Study of Liver 2009; 15: 1493-8.
25. Hu B, Gao DJ, Yu FH, Wang TT, Pan YM, Yang XM. Endoscopic stenting for post-transplant biliary stricture: usefulness of a novel removable covered metal stent. J Hepatobiliary Pancreat Sci 2011; 18: 640-5.
26. Chaput U, Scatton O, Bichard P, et al. Temporary placement of partially covered self-expandable metal stents for anastomotic biliary strictures after liver transplantation: a prospective, multicenter study. Gastrointest Endosc 2010; 72: 1167-74.
27. Garcia-Pajares F, Sanchez-Antolin G, Pelayo SL, et al. Covered metal stents for the treatment of biliary complications after orthotopic liver transplantation. Transplant Proc 2010; 42: 2966-9.
28. Garcia-Cano J, Taberna-Arana L, Jimeno-Ayllon C, et al. Use of fully covered self-expanding metal stents for the management of benign biliary conditions. Rev Esp Enferm Dig 2010; 102: 526-32.
29. Marin-Gomez LM, Sobrino-Rodriguez S, Alamo-Martinez JM, et al. Use of fully covered self-expandable stent in biliary complications after liver transplantation: a case series. Transplant Proc 2010; 42: 2975-7.
30. Tee HP, James MW, Kaffes AJ. Placement of removable metal biliary stent in post-orthotopic liver transplantation anastomotic stricture. World J Gastroenterol 2010; 16: 3597-600.
31. Doros A, Nemeth A, Deak AP, et al. Successful treatment with a covered stent and 6-year follow-up of biliary complication after liver transplantation. Cardiovasc Intervent Radiol 2010; 33: 425-9.
32. Mahajan A, Ho H, Sauer B, et al. Temporary placement of fully covered self-expandable metal stents in benign biliary strictures: midterm evaluation (with video). Gastrointest Endosc 2009; 70: 303-9.
33. Phillips MS, Bonatti H, Sauer BG, et al. Elevated stricture rate following the use of fully covered self-expandable metal biliary stents for biliary leaks following liver transplantation. Endoscopy 2011; 43: 512-7.
34. Ostroff JW. Management of biliary complications in the liver transplant patient. Gastroenterol Hepatol (N Y) 2010; 6: 264-72.
35. Scatton O, Meunier B, Cherqui D, et al. Randomized trial of choledochocholedochostomy with or without a T tube in orthotopic liver transplantation. Ann Surg 2001; 233: 432-7.
36. Wang SF, Huang ZY, Chen XP. Biliary complications after living donor liver transplantation. Liver Transpl 2011; 17: 1127-36.
37. Duailibi DF, Ribeiro MA, Jr. Biliary complications following deceased and living donor liver transplantation: a review. Transplant Proc 2010; 42: 517-20.
38. Kobayashi N, Kubota K, Shimamura T, et al. Complications of the treatment of endoscopic biliary strictures developing after liver transplantation. J Hepatobiliary Pancreat Sci 2011; 18: 202-10.
39. Dacha S, Barad A, Martin J, Levitsky J. Association of hepatic artery stenosis and biliary strictures in liver transplant recipients. Liver Transpl 2011; 17: 849-54.
40. Foley DP, Fernandez LA, Leverson G, et al. Biliary complications after liver transplantation from donation after cardiac death donors: an analysis of risk factors and long-term outcomes from a single center. Ann Surg 2011; 253: 817-25.
41. Qian YB, Liu CL, Lo CM, Fan ST. Risk factors for biliary complications after liver transplantation. Arch Surg 2004; 139: 1101-5.
42. Yuan D, Wei YG, Lin HM, et al. Risk factors of biliary complications following liver transplantation: retrospective analysis of a single centre. Postgrad Med J 2009; 85: 119-23.
43. Chang TI, Ho MC, Wu YM, Lee PH, Hu RH. Biliary complications after liver transplantation: an 18-year single-center experience. J Formos Med Assoc 2011;110:183-9.
44. Truesdale AE, Caldwell SH, Shah NL, et al. Sorafenib therapy for hepatocellular carcinoma prior to liver transplant is associated with increased complications after transplant. Transpl Int 2011; 24: 991-8.
45. Tabibian JH, Yeh HC, Singh VK, Cengiz-Seval G, Cameron AM, Gurakar A. Sirolimus may be associated with early recurrence of biliary obstruction in liver transplant patients undergoing endoscopic stenting of biliary strictures. Ann Hepatol 2011; 10: 270-6.
46. Mathur AK, Ranney DN, Patel SP, et al. The effect of smoking on biliary complications following liver transplantation. Transpl Int 2011; 24: 58-66.
47. Pungpapong S, Manzarbeitia C, Ortiz J, et al. Cigarette smoking is associated with an increased incidence of vascular complications after liver transplantation. Liver Transpl 2002; 8: 582-7.
48. Gunawansa N, McCall JL, Holden A, Plank L, Munn SR. Biliary complications following orthotopic liver transplantation: a 10-year audit. HPB (Oxford) 2011; 13: 391-9.
49. Wang MF, Jin ZK, Chen DZ, Li XL, Zhao X, Fan H. Risk factors of severe ischemic biliary complications after liver transplantation. Hepatobiliary Pancreat Dis Int 2011; 10: 374-9.
1. Starzl TE, Marchioro TL, Vonkaulla KN, Hermann G, Brittain RS, Waddell WR. Homotransplantation of the Liver in Humans. Surgery, gynecology & obstetrics 1963; 117: 659-76. [ Links ]
2. Balderramo D, Navasa M, Cardenas A. Current management of biliary complications after liver transplantation: emphasis on endoscopic therapy. Gastroenterol Hepatol 2011; 34: 107-15. [ Links ]
3. Starzl TE, Putnam CW, Hansbrough JF, Porter KA, Reid HA. Biliary complications after liver transplantation: with special reference to the biliary cast syndrome and techniques of secondary duct repair. Surgery 1977; 81: 212-21. [ Links ]
4. Muñoz OG, Insuasty MR, Marín JI, et al. Complicaciones de la vía biliar después de trasplante ortotópico de hígado: Experiencia en el Hospital Pablo Tobón Uribe - Medellín. Rev Col Gastroenterol 2011; 26: 9-14. [ Links ]
5. Yagci G, Cetiner S, Ersoz N, et al. The effect of gained experience on postoperative complications and mortality in cadaveric liver transplantation: a single-center experience. Transplant Proc 2011; 43: 912-6. [ Links ]
6. Vera A, Contreras F, Guevara F. Incidence and risk factors for infections after liver transplant: single-center experience at the University Hospital Fundacion Santa Fe de Bogotá, Colombia. Transplant infectious disease : an official journal of the Transplantation Society 2011. [ Links ]
7. Noack K, Bronk SF, Kato A, Gores GJ. The greater vulnerability of bile duct cells to reoxygenation injury than to anoxia. Implications for the pathogenesis of biliary strictures after liver transplantation. Transplantation 1993; 56: 495-500. [ Links ]
8. Krok KL, Cardenas A, Thuluvath PJ. Endoscopic management of biliary complications after liver transplantation. Clin Liver Dis 2010; 14: 359-71. [ Links ]
9. Ryu CH, Lee SK. Biliary strictures after liver transplantation. Gut Liver 2011; 5: 133-42. [ Links ]
10. Kuo PC, Lewis WD, Stokes K, Pleskow D, Simpson MA, Jenkins RL. A comparison of operation, endoscopic retrograde cholangiopancreatography, and percutaneous transhepatic cholangiography in biliary complications after hepatic transplantation. J Am Coll Surg 1994; 179: 177-81. [ Links ]
11. Londono MC, Balderramo D, Cardenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol 2008; 14: 493-7. [ Links ]
12. Williams ED, Draganov PV. Endoscopic management of biliary strictures after liver transplantation. World J Gastroenterol 2009; 15: 3725-33. [ Links ]
13. Sanna C, Giordanino C, Giono I, et al. Safety and efficacy of endoscopic retrograde cholangiopancreatography in patients with post-liver transplant biliary complications: results of a cohort study with long-term follow-up. Gut Liver 2011; 5: 328-34. [ Links ]
14. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991; 37: 383-93. [ Links ]
15. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 2010; 71: 446-54. [ Links ]
16. Morelli J, Mulcahy HE, Willner IR, Cunningham JT, Draganov P. Long-term outcomes for patients with post-liver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc 2003; 58: 374-9. [ Links ]
17. Krol R, Karkoszka H, Ziaja J, et al. Biliary complications after orthotopic liver transplantation: a 5-year experience. Transplant Proc 2011; 43: 3035-8. [ Links ]
18. Thuluvath PJ, Atassi T, Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int 2003; 23: 156-62. [ Links ]
19. Kulaksiz H, Weiss KH, Gotthardt D, et al. Is stenting necessary after balloon dilation of post-transplantation biliary strictures? Results of a prospective comparative study. Endoscopy 2008; 40: 746-51. [ Links ]
20. Davidson BR, Rai R, Nandy A, Doctor N, Burroughs A, Rolles K. Results of choledochojejunostomy in the treatment of biliary complications after liver transplantation in the era of nonsurgical therapies. Liver Transpl 2000; 6: 201-6. [ Links ]
21. Li QY, Qin YS, Ling Q, Yang FC, Zheng SS. No Therapeutic ERCP in Anastomotic Stricture without Intrahepatic Biliary Dilation after Liver Transplantation. Hepatogastroenterology 2011; 58: 1127-31. [ Links ]
22. Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy 2005; 37: 857-63. [ Links ]
23. Ostroff JW. Post-transplant biliary problems. Gastrointest Endosc Clin N Am 2001; 11: 163-83. [ Links ]
24. Traina M, Tarantino I, Barresi L, et al. Efficacy and safety of fully covered self-expandable metallic stents in biliary complications after liver transplantation: a preliminary study. Liver transplantation : official publication of the American Association for the Study of Liver 2009; 15: 1493-8. [ Links ]
25. Hu B, Gao DJ, Yu FH, Wang TT, Pan YM, Yang XM. Endoscopic stenting for post-transplant biliary stricture: usefulness of a novel removable covered metal stent. J Hepatobiliary Pancreat Sci 2011; 18: 640-5. [ Links ]
26. Chaput U, Scatton O, Bichard P, et al. Temporary placement of partially covered self-expandable metal stents for anastomotic biliary strictures after liver transplantation: a prospective, multicenter study. Gastrointest Endosc 2010; 72: 1167-74. [ Links ]
27. Garcia-Pajares F, Sanchez-Antolin G, Pelayo SL, et al. Covered metal stents for the treatment of biliary complications after orthotopic liver transplantation. Transplant Proc 2010; 42: 2966-9. [ Links ]
28. Garcia-Cano J, Taberna-Arana L, Jimeno-Ayllon C, et al. Use of fully covered self-expanding metal stents for the management of benign biliary conditions. Rev Esp Enferm Dig 2010; 102: 526-32. [ Links ]
29. Marin-Gomez LM, Sobrino-Rodriguez S, Alamo-Martinez JM, et al. Use of fully covered self-expandable stent in biliary complications after liver transplantation: a case series. Transplant Proc 2010; 42: 2975-7. [ Links ]
30. Tee HP, James MW, Kaffes AJ. Placement of removable metal biliary stent in post-orthotopic liver transplantation anastomotic stricture. World J Gastroenterol 2010; 16: 3597-600. [ Links ]
31. Doros A, Nemeth A, Deak AP, et al. Successful treatment with a covered stent and 6-year follow-up of biliary complication after liver transplantation. Cardiovasc Intervent Radiol 2010; 33: 425-9. [ Links ]
32. Mahajan A, Ho H, Sauer B, et al. Temporary placement of fully covered self-expandable metal stents in benign biliary strictures: midterm evaluation (with video). Gastrointest Endosc 2009; 70: 303-9. [ Links ]
33. Phillips MS, Bonatti H, Sauer BG, et al. Elevated stricture rate following the use of fully covered self-expandable metal biliary stents for biliary leaks following liver transplantation. Endoscopy 2011; 43: 512-7. [ Links ]
34. Ostroff JW. Management of biliary complications in the liver transplant patient. Gastroenterol Hepatol (N Y) 2010; 6: 264-72. [ Links ]
35. Scatton O, Meunier B, Cherqui D, et al. Randomized trial of choledochocholedochostomy with or without a T tube in orthotopic liver transplantation. Ann Surg 2001; 233: 432-7. [ Links ]
36. Wang SF, Huang ZY, Chen XP. Biliary complications after living donor liver transplantation. Liver Transpl 2011; 17: 1127-36. [ Links ]
37. Duailibi DF, Ribeiro MA, Jr. Biliary complications following deceased and living donor liver transplantation: a review. Transplant Proc 2010; 42: 517-20. [ Links ]
38. Kobayashi N, Kubota K, Shimamura T, et al. Complications of the treatment of endoscopic biliary strictures developing after liver transplantation. J Hepatobiliary Pancreat Sci 2011; 18: 202-10. [ Links ]
39. Dacha S, Barad A, Martin J, Levitsky J. Association of hepatic artery stenosis and biliary strictures in liver transplant recipients. >Liver Transpl 2011; 17: 849-54. [ Links ]
40. Foley DP, Fernandez LA, Leverson G, et al. Biliary complications after liver transplantation from donation after cardiac death donors: an analysis of risk factors and long-term outcomes from a single center. Ann Surg 2011; 253: 817-25. [ Links ]
41. Qian YB, Liu CL, Lo CM, Fan ST. Risk factors for biliary complications after liver transplantation. Arch Surg 2004; 139: 1101-5. [ Links ]
42. Yuan D, Wei YG, Lin HM, et al. Risk factors of biliary complications following liver transplantation: retrospective analysis of a single centre. Postgrad Med J 2009; 85: 119-23. [ Links ]
43. Chang TI, Ho MC, Wu YM, Lee PH, Hu RH. Biliary complications after liver transplantation: an 18-year single-center experience. J Formos Med Assoc 2011;110:183-9. [ Links ]
44. Truesdale AE, Caldwell SH, Shah NL, et al. Sorafenib therapy for hepatocellular carcinoma prior to liver transplant is associated with increased complications after transplant. Transpl Int 2011; 24: 991-8. [ Links ]
45. Tabibian JH, Yeh HC, Singh VK, Cengiz-Seval G, Cameron AM, Gurakar A. Sirolimus may be associated with early recurrence of biliary obstruction in liver transplant patients undergoing endoscopic stenting of biliary strictures. Ann Hepatol 2011; 10: 270-6. [ Links ]
46. Mathur AK, Ranney DN, Patel SP, et al. The effect of smoking on biliary complications following liver transplantation. Transpl Int 2011; 24: 58-66. [ Links ]
47. Pungpapong S, Manzarbeitia C, Ortiz J, et al. Cigarette smoking is associated with an increased incidence of vascular complications after liver transplantation. Liver Transpl 2002; 8: 582-7. [ Links ]
48. Gunawansa N, McCall JL, Holden A, Plank L, Munn SR. Biliary complications following orthotopic liver transplantation: a 10-year audit. HPB (Oxford) 2011; 13: 391-9. [ Links ]
49. Wang MF, Jin ZK, Chen DZ, Li XL, Zhao X, Fan H. Risk factors of severe ischemic biliary complications after liver transplantation. Hepatobiliary Pancreat Dis Int 2011; 10: 374-9. [ Links ]











 text in
text in