Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.27 no.4 Bogotá oct./dic. 2012
Case report
(1) Gastro-hepatology Group of the Faculty of Medicine at the Hospital Pablo Tobón Uribe, Universidad de Antioquia in Medellín, Colombia
(2) Hospital Pablo Tobón Uribe, Universidad de Antioquia in Medellín, Colombia
(3) Resident in Internal Medicine at the Universidad Pontificia Bolivariana
Received: 03-05-12 Acceted: 23-10-12
Abstract
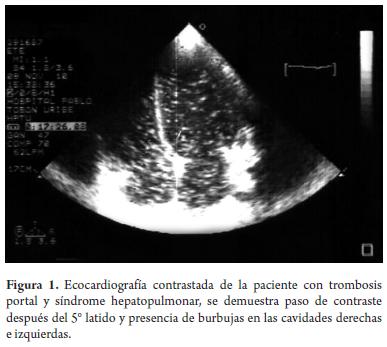
We report the case of a female patient diagnosed with hepatopulmonary syndrome (HPS) which occurred in the context of chronic thrombosis of the portal and mesenteric veins resulting from primary thrombophilia (protein C and protein S deficiencies). This case of HPS was diagnosed when echocardiography with agitated saline contrast showed the patient was positive for extra cardiac shunt. Scintigraphy using albumin macro-aggregates showed evidence of uptake in the brain and persistent hypoxemia with elevated alveolar-arterial gradient for the age of the patient.
Key words
Hepatopulmonary syndrome, portal vein thrombosis, nodular regenerative hyperplasia.
INTRODUCTION
More than 50% of patients with hepatic diseases have respiratory symptoms and of these patients 30% may present pulmonary diseases as the cause of these symptoms (1).
Complications of chronic hepatic diseases cause changes in lung mechanics which can be manifested as hypoxemia, although patients with hepatopulmonary syndrome (HPS) may manifest in other ways from secondary hypoxemia to alterations in the pulmonary blood vessels. HPS is characterized by the appearance of persistent hypoxemia in a patient with hepatic disease and vascular lung dilation (2). The vascular component includes difuse or local dilation of the pulmonary capillaries, and less commonly includes pulmonary arteriovenous shunts.
The term hepatopulmonary syndrome (HPS) was first introduced into the literature by Kennedy and Kudson in 1977, and many definitions have been proposed since then. Currently most of the evidence comes from isolated reports and case studies which use widely varying diagnostic criteria. Reported prevalence ranges from 15% to 32% among patients sufering from liver cirrhosis depending on the criteria used. This variability is explained by the lack of consensus about hypoxemia values and the use tests to confirm HPS (3). HPS can also occur in acute liver diseases such as viral hepatitis and hepatic failure (4). To date, there have been few cases and series that report the presence of HPS together with cirrhotic portal hypertension. The characteristics of these patients have not yet been fully studied (5).
The following is the case of a woman with portal hypertension of non cirrhotic origin who developed hepatopulmonary syndrome which was subsequently treated at the Liver Unit of Hospital Pablo Tobon Uribe.
CASE DESCRIPTION
The patient was a 21 year old student who resided in a rural area who had no relevant personal medical precedents. She was transferred from a second level complexity hospital after being diagnosed with cirrhosis and nonspecific pulmonary compromise due to persistent asymptomatic hypoxemia. Upon admission she had had no supplemental oxygen. Her oxygen saturating was 80%, she presented oral and distal cyanosis and Hippocratic fngers. Physical examination showed was no evidence of chronic hepatopathy. Her hepatic profle was AST: 41 U/L, ALT: 29 U/L, ALP: 114 U/L, GGT: 161 U/L, TP Ins 8.12, INR: 1.2, albumin 3.1 g/dL and her complete blood count showed 87,000 cells/mm3 of thrombocytopenia.
At that time there was no clinical, paraclinical or imaging evidence of cirrhosis. after hospitalization, a triphasic abdominal CAT scan showed chronic portal thrombosis with mesenteric extension and severe collateral circulation. The thrombophilia study found a deficit of C and S coagulation proteins. The hypoxemia study showed arterial gases had a PO2 of 57 mmHg and an A-a gradient of 30 mmHg (15 mmHg is expected for that age). An angio-thorax CAT-Scan resulted in rejection of pulmonary embolism. Normal cardiac structures were found in echocardiography, but after applying agitated saline solution it showed the passage of bubbles to lef cavities after fifth heartbeat compatible with extracardiac shunt (Figure 1). Magnetic Resonance Angiography (MR) of the heart revealed a structurally normal heart, and gammagraphy with albumin macroaggregates showed abnormal reception of the tracer at the brain level. Right heart catheterization was performed demonstrating pulmonary artery pressure of 40/10 mmHg, with a mean of 25 mmHg. The diagnosis of hepatopulmonary syndrome with presinusoidal portal hypertension without hepatic cirrhosis was then made. The patient is currently receiving anticoagulation treatment and oxygen at home. She is asymptomatic, has good functions and a strong family, social and work life.
DISCUSSION
HPS is characterized by permanent hypoxemia in patients with underlying secondary hepatic disease in the presence of vessel lung dilation (6).
Hypoxemia is associated with a broad alveolar-arterial gradient (Aa) of oxygen. This is defined as one above 15 mmHg, as over 25 mmHg in people older than 65 years, or defined as increasing with age by: Aa Gradient (0.26 x age - 0.43) + 10. Hypoxemia severity is classified according to PO2: it is low when PO2 is 80 mmHg, moderate at 60-80 mmHg, severe at 50-60 mmHg, and quite severe with PO2 less than 50 mmHg (7).
In early stages, a patient with hepatopulmonary syndrome remains asymptomatic. There are no pathognomonic symptoms or signs of this syndrome, though there were symptomatic findings suggestive of it. The patient may report dyspnea, especially when changing position from lying to siting or standing (platypnea) and physical examination may show orthodeoxia (decreasing PaO2 or O2 saturation resulting from change of positions). Cyanosis, digital hippocratism and telangiectasias (as a manifestation of systemic vessel dilation) can also appear. Hypoxemia occurs as a result of several mechanisms: first, as an alteration of ventilation-perfusion, second, as the presence of truly anatomic shunts, and third as the decline in the difusion-perfusion (8).
Physiopathologically, HPS reffects an abnormal dilation of the pulmonary bed which has been atributed among other factors to the overproduction of nitric oxide. This molecule is one of the most potent pulmonary vessel dilators and appears to be responsible not only for the hyperdynamic and splanchnic vessel dilation, but also for the HPS (9).
At the microvascular level, endothelial synthesis of nitric oxide and increased expression of the inducible form of this enzyme in macrophages result in increased production of nitric oxide. This is augmented as the endothelin-1 production at the hepatic level and overexpression of endothelin receptors in the pulmonary vascular bed also stimulate production of nitric oxide (10).
There is then a significant hemodynamic change. The pulmonary capillaries expand to reach diameters of up to 100 microns, thereby generating short circuits from lef to right and the alterations described in oxygenation.
These hemodynamic changes, pulmonary vessel dilation and extracardiac short circuiting, are the foundations for the confirmed diagnosed methods of HPS.
The echocardiography contrasted with agitated saline solution is a procedure applied via a peripheral vein. The agitated saline solution forms bubbles larger than 10 microns. Under normal conditions the bubbles go to right cavities, stop at the capillary level of the lungs, and are not observable ecocardiographically in the lef chambers. In the HPS context, where capillaries measure much more than 15 microns, bubbles pass through the capillaries and enter the lef cardiac chambers between the third and sixth beat after application of the solution completely shadowing the lef cardiac cavities. If the passage of bubbles occurs before the third pulse this indicates that intra cardiac communication and its causes are outside the scope of this review. Another diagnostic method based on the same hemodynamic principles is gammagraphy with albumin macroa-ggregates, where albumin macromolecules 20 microns in diameter are injected. Any acquisition (primarily cerebral or renal) of the contrast media is considered to be positive for left-right shunt (without differentiating whether it is intracardiac or extracardiac) (11, 12).
Any form of acute or chronic hepatic disease can coexist with hypoxemia due to dilation of the pulmonary vessels. Consequently, portal hypertension is not essential for manifestation of this syndrome. Although cases of hepatic failure and acute hepatitis have been reported, they are the exceptions because what they have in common is the description of the syndrome in cirrhotic patients with portal hypertension. These cases have no association with the etiology of cirrhosis, and the relationship with the severity of hepatic dysfunction or portal hypertension is not yet clear.
Despite advances in knowledge about HPS, there are few publications about patients with portal hypertension, who do not have cirrhosis, but who do have this syndrome. There are a number of hepatic entities for which there have been reported cases of HPS other than cirrhosis. They include idiopathic portal hypertension, portal thrombosis, congenital hepatic fibrosis, Budd - Chiari syndrome, hepatic metastases, neonatal hepatitis and nodular regenerative hyperplasia. Still, there are no clearly known mechanisms by which HPS develops in these pathologies (13). Currently, it is calculated that 4% to 8% of the hepatopulmonary cases occur in patients with non-cirrhotic portal hypertension. The literature about the coexistence of HPS in patients with non-cirrhotic portal hypertension is limited to case reports and controlled studies with small sample sizes. In 2000, Binay and his collaborators (14) demonstrated the presence of HPS in non-cirrhotic patients. They defined the HPS diagnostic criteria for the study as positive CE, PaO2 less than 70 mmHg and A-a gradient greater than 20 mmHg. They evaluated 25 patients with non-cirrhotic portal hypertension with contrast echocardiography with agitated saline solution. Two patients met the criteria for HPS, and both had normal hepatic and pulmonary functioning. During the same year, the author described the characteristics of two other patients with HPS and Budd - Chiari syndrome. Both underwent derivation through cavoplasty, one successfully, the other unsuccessfully. The patient who could be diverted was given oxygen for eight weeks and recovered from dyspnea (15).
One of the largest studies of HPS was conducted between 1996 and 1998 and published in 2003 (13). In that study the incidence of HPS among 45 patients with hepatic cirrhosis patients and 31 patients with non-cirrhotic portal hypertension was compared. It was found that fve (10.8%) of patients with cirrhosis and three (9.7%) patients without cirrhosis met the diagnostic criteria for HPS. The conclusions were that cirrhosis is not a prerequisite for the development of this syndrome and that patients with idiopathic portal hypertension and portal vein thrombosis may also develop HPS, as described in our case above.
So far there is no efective medical therapy for HPS. Liver transplantation, with 5 year survival rates of about 75%, is the only therapeutic option (16). In these cases, mortality and resolution of hypoxemia are related to the severity of the hypoxemia prior to transplant. Therapies that have been tried in an anecdotal way, but which have no support from the literature, include antibiotics, beta blockers, glucocorticoids, nitric oxide inhibitors, somatostatin, and cyclophosphamide, but none have been successful.
Isolated cases of the use of interventional therapies such as intrahepatic transjugular portosystemic shunts (TIPS, cavoplasty and embolization of arteriovenous shunts to improve the portal pressure gradient have also been reported in. For this reason, patients with contraindications for liver transplantation only receive symptomatic management with ambulatory oxygen therapy.
There are no descriptions of treatment of HPS in patients with non-cirrhotic portal hypertension. In 2011, Maganty and Ghanta reported the case of a 26 year old patient with portal hypertension secondary to nodular regenerative hyperplasia who had dyspnea and platypnea and who required home oxygen. The patient had a MELD of 10, and her only indication for transplant was lung compromise. After undergoing orthotopic liver transplantation her post operative examination showed persistent hypoxia. During the following three weeks she gradual improved and oxygen was totally removed (17).
The patient described above is now being managed with anticoagulation indicated for the thrombophilia described and with ambulatory oxygen. At the moment no interventional therapy is planned, and she has contraindications for liver transplantation due to the extension of portal vein thrombosis and the technical limitations of this complication.
REFERENCES
1. Kochar R, Nevah Rubin MI, Fallon MB. Pulmonary complications of cirrhosis. Curr Gastroenterol Rep 2011; 13(1): 34-9. [ Links ]
2. Wolfe JD, Tashkin DP, Holly FE, et al. Hypoxemia of cirrhosis. Detection of abnormal small pulmonary vascular channels by a quantitative radionuclide method. Am J Med 1977; 63(5): 746-74. [ Links ]
3. Castaing Y, Manier G. Hemodynamic disturbances and VA/Q matching in hypoxemic cirrhotic patients. Chest 1989; 96(5): 1064-9. [ Links ]
4. Regev A, Yeshurun M, Rodríguez M, Sagie A, Nef GW, Molina EG, Schif ER: Transient hepatopulmonary syndrome in a patient with acute hepatitis A. J Viral Hep 2001; 8: 83-86. [ Links ]
5. Babbs C, Warnes TW, Haboubi NY. Noncirrhotic portal hypertension with hypoxemia. Gut 1988; 29: 129-131. [ Links ]
6. Mandell MS. Clinical controversies surrounding the diagnosis and treatment of hepatopulmonary syndrome. Minerva Anestesiol 2007; 73(6): 347-55. [ Links ]
7. Ho V. Current concepts in the management of hepatopulmonary syndrome. Vasc Health Risk Manag 2008; 4(5): 1035-41. [ Links ]
8. Rodríguez-Roisin R, Roca J, Agustí AGN, Mastai R, Wagner PD, Bosch J. Gas exchange and pulmonary vascular reactivity in patients with liver cirrhosis. Am Rev Respir Dis 1987; 135: 1085-1092. [ Links ]
9. Rolla G. Is nitric oxide the ultimate mediator in hepatopulmonary syndrome? J Hepatol 2003; 38: 668-670. [ Links ]
10. Fallon MB, Abrams GA, Luo B, Hou Z, Dai J, Ku DD. The role of endothelial nitric oxide synthase in the pathogenesis of a rat model of hepatopulmonary syndrome. Gastroenterology 1997; 113: 606-14. [ Links ]
11. Palma DT, Fallon MB. The hepato pulmonary syndrome. J Hepatol 2006; 45(4): 617-25. [ Links ]
12. Rodríguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome a liver-induced lung vascular disorder. N Engl J Med 2008; 358(22): 2378-87. [ Links ]
13. Kaymakoglu S, Kahraman T, Kudat H, Demir K, Cakaloglu Y, Adalet I, Dincer D, Besisik F, Boztas G, Sözen AB, Mungan Z, Okten A. Hepatopulmonary syndrome in noncirrhotic portal hypertensive patients. Dig Dis Sci 2003; 48(3): 556-60. [ Links ]
14. De BK, Sen S, Sanyal R. Hepatopulmonary syndrome in noncirrhotic portal hypertension. Ann Intern Med 2000; 132(11): 924. [ Links ]
15. De BK, Sen S, Biswas PK, Sanyal R, Majumdar D, Biswas J. Hepatopulmonary syndrome in inferior vena cava obstruction responding to cavoplasty. Gastroenterology 2000; 118(1): 192-6. [ Links ]
16. Swanson KL, Wiesner RH, Krowka MJ. Natural history of hepatopulmonary syndrome: impact of liver transplantation. Hepatology 2005; 41: 1122-9. [ Links ]
17. Maganty K, Ghanta R, Bejarano P, Weppler D, Tekin A, Moon J, Nishida S, Tzakis A, Martin P. Liver transplantation for hepatopulmonary syndrome due to noncirrhotic portal hypertension. Transplant Proc 2011; 43(7): 2814-6. [ Links ]











 texto en
texto en 

