Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.27 no.4 Bogotá oct./dic. 2012
Case report
(1) Internist and Professor of Gastroenterology in the Faculty of Medicine at the Universidad Nacional de Colombia, Gastroenterologist at Hospital El Tunal in Bogotá, Colombia.
(2) Internist and Gastroenterologist at the Universidad Nacional de Colombia and the Clínica de la Policía in Bogotá, Colombia.
(3) Professor and Coordinator of Gastroenterology in the Faculty of Medicine at the Universidad Nacional de Colombia, Gastroenterologist at the Clínica Fundadores in Bogotá, Colombia.
Received: 06-08-12 Accepted: 23-10-12
Abstract
In 1890 Ludwig Courvoisier and Louis-Felix Terrier described a common bile duct obstruction leading to secondary dilation of the gallbladder to the point that it could be felt. We present a case report which illustrates this important sign together with a historical account of the authors who first described it. We show how new diagnostic methods can help diagnose this etiology.
Key words
Courvoisier-Terrier's sign, history, diagnosis.
120 years ago Ludwig Courvoisier and Louis Terrier described one of the classic signs in medicine, a sign that has endured the passage of time and modern imaging techniques (1), despite demonstration of multiple exceptions.
We refer to the Courvoisier-Terrier's sign, a painless palpable finding from physical examination of the gallbladder. Despite the passage of years this sign has contextualized the scenario of malignant obstructions of the common gallbladder which are pathophysiologically explained by progressively increasing hydrostatic pressure that leads to distention of the gallbladder's flexible walls (2).
In this article we review a clinical case that exemplifes Courvoisier-Terrier's sign and allows us to review the pathophysiological facts that lead to this find.
CLINICAL CASE
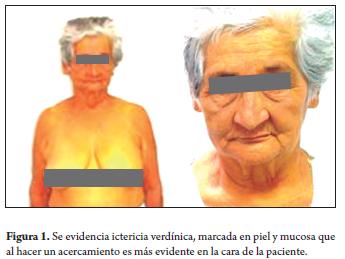
A 72 year old woman was admited to Hospital el Tunal in Bogotá, Colombia following a month evolution of severe pain in the right hypochondrium radiating to the back and associated with choluria, acholia and progressive greenish jaundice the symptoms which resulted her initial hospitalization at small local hospital. The patient mentioned no relevant background. Upon physical examination the patient showed stable vital signs with greenish jaundice that compromised both the skin and mucosa in a generalized form (Figure 1). The abdomen was sof and without signs of peritoneal irritation, but a consistently painless mass was felt over the right hypochondrium that corresponded to the bladder (positive for Courvoisier-Terrier's sign). There were no signs of peritoneal irritation.
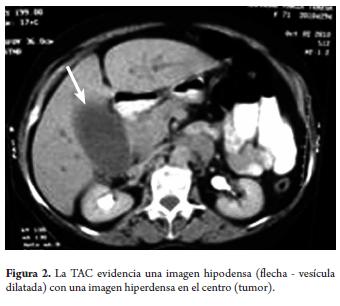
Due to the patient's clinical characteristics, tests were done for a possible obstructive biliary pathology of malignant etiology. Hyperbilirubinemia resulting from direct bilirubin and elevated alkaline phosphatase was found (Table 1). An abdominal CAT showed gallbladder distension associated with dilatation of the intrahepatic and extrahepatic bile duct and with an increase in the size of the pancreatic head (Figure 2). As a result of these findings an ERCP was performed, but pancreatography failed to find any lesions. Management with ampicillin sulbactam was begun in order to prevent cholangitis.
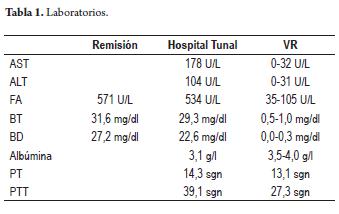
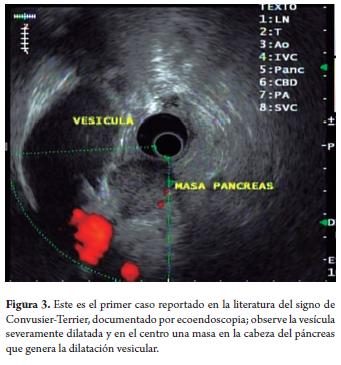
Patient was transferred to Hospital el Tunal in Bogotá where her hepatic profle was assessed. Once again hyperbilirubinemia due to direct bilirubin, elevated transaminases, hypoalbuminemia, slightly prolonged cloting times (Table 1) and CBC without anemia was found. In face of these findings pancreatic cancer was suspected. Echoendoscopy showed an image suggestive of pancreatic cancer with a severely dilated bladder (Figure 3). THe decision was made to perform another ERCP to treat the obstruction since the patient was rapidly deteriorating as the result of cholangitis. Unfortunately, the ERCP failed again, and the patient died the next day due to severe sepsis before there was any chance of transparietal liver drainage and palliative care.
DISCUSSION
Ludwig Georg Courvoisier (1843-1918) was born in Basel, Switzerland. After graduation from the local university's medicine school, he travelled to Vienna where he was tutored by Czerny and Billroth. He then went to London where he was tutored by Wells and Ferguson and where he did his studies in gastrointestinal surgery, the work to which he dedicated his academic life. Back in Basel he focused his interests on biliary tract surgery. 12 years later he was named professor at the University of Basel and became one of the great figures of his time. Among his notable interventions was the first successful choledocholithotomy and the development of multiple cholecystectomy surgical techniques. He was also an expert in entomology and botany (2).
Louis Felix Terrier (1837-1908) was born in Paris, France. He began his studies as a veterinarian but later changed his focus and registered in the school of medicine of the French capital. He became a distinguished surgeon and faculty professor. Like Courvoisier, he described the dilatation of the gallbladder in the context of obstructive greenish jaundice and fecal discoloration (2).
Courvoisier Terrier's syndrome was described 120 years ago by these two authors when they evaluated 187 cases.
They divided the patients into two groups: 87 patients with obstructions caused by stones and 100 patients with obstructions due to other causes. They found that in the group with bile duct obstructions due to stones bladder atrophy was more common than distension (70 cases: 80%) while in the other group bladder dilatation was more common find (92 cases: 92%). They concluded that common bile duct obstruction secondary to stone rarely results in bladder dilatation while in contrast a malignant obstruction of the duct commonly causes bladder dilatation (3). Recent studies report that 83% of palpable bladders result in distal tumors while 15% are secondary to obstruction from stones in the distal region of the common bile duct. Physical examination can only identify 53% of distended bladders while computed tomography can identify 87% which helps prioritize surgery (1) as in this case.
The pathophysiological explanation of these findings is based on the fact that stones irritate the cystic duct as well as the bladder leading to chronic inflammation which in turn produces alterations in the wall. These chronic changes can produce fibrosis in the duct as well as in the bladder thus preventing biliary congestion from distending bladder walls. In contrast, obstruction from other causes, especially from the compression caused by a tumor, progressively elevates the retrograde hydrostatic pressure which causes the flexible wall of the bladder to distend. The amount of distension depends on the degree of obstruction (4). The greenish jaundice found in a physical examination is a consequence of oxidation of the circulating bilirubin into biliverdin, a reaction that is most frequently observed in disorders accompanied by long duration of hyperbilirubinemia (5).
The designation as of "law" for this sign has been the subject of great debate over time since several exceptions to the norm have been found. These include the presence of chronic and autoimmune pancreatitis, bile duct obstruction due to parasites, cholangiopathy associated with AIDS, congenital choledochal cysts, and congestion of the common hepatic duct proximal to the cystic duct insertion as in the case of adenomegalies of the portal vein and hilar cholangiocarcinoma. This is why the absence of this sign does not exclude or confirm a pathological malignancy (3), thus we prefer to denominate it as, "Courvoisier Terrier's sign" rather than Courvoisier's law. It is worth highlighting that the case presented here illustrates the validity and importance of a careful physical examination of the patient even when good images exist, no mater how complex the images may be.
CONCLUSIONS
Whether or not an obstruction is chronic is the key to explaining the clinical and paraclinical findings of this syndrome. Sub-acute or chronically elevated intraductal pressures are more susceptible to developing into malignant obstructions due to the gradual and progressive nature of the disease. Nevertheless, because there are many exceptions, it is not possible to consider Courvoisier Terrier's sign a law. Rather, it should be understood as something that needs to be evaluated within each patient's clinical context. It is important to highlight that when the original authors described this observation, there were none of the imaging aids which we currently have such as ultrasound, CT scans, MRIs or ERCPs. We therefore consider it important to remind clinicians that the signs and symptoms have not lost their utility or validity and thus their use in daily clinical practice should be reestablished.
REFERENCES
1. Fitzgerald J White. M. Courvoisier's Gallbladder: law or sign. World J Surg 2009; 33: 886-891. [ Links ]
2. Fresquet Febrer JL, Aguirre Marco C. La cirugía en la historia. La revolución quirúrgica y la cirugía científica. Valencia, manuscrito; 1995. [ Links ]
3. Haubrich W. Courvoisier of Courvoisier's sign. Gastroenterology 2004; 127(4): 1037-1040. [ Links ]
4. García J, Jimeno C. Distensión de la vesícula biliar por obstrucción tumoral coledociana. Rev Esp Enferm Dig 2007; 99 (8): 469-470. [ Links ]
5. Viteri AL. Courvoisier's law and evaluation of the jaundiced patient. Tex Med 1999; 76: 60-61. [ Links ]











 texto en
texto en 

