Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.1 Bogotá Jan./Mar. 2013
Biliary complications in transplant patients: A comparison of two ERCP diagnostic methods
Vanesa García, MD. (1), Federico Acosta, MD. (2), Julián Cano MD,3 Claudia Montoya, MD. (3), Gonzalo Correa Arango, MD. (4), Juan Carlos Restrepo G., MD. (5), Rodrigo Castaño Llano, MD. (6)
(1) Radiologist specializing in Corporal Imaging at the Hospital Pablo Tobón Uribe, Professor at the Universidad de Antioquia
(2) Corporal Imaging Radiologist at the Universidad de Antioquia. Medellín, Colombia
(3) Emergency and Trauma Radiologist at the Universidad de Antioquia. Medellín, Colombia
(4) Internist and Hepatologist in the Gastro-hepatology Group at the Universidad de Antioquia, Chief of the Liver Transplant Group at the Hospital Pablo Tobón Uribe. Medellín, Colombia
(5) Internist and Hepatologist in the Gastro-hepatology Group at the Universidad de Antioquia and the Hospital Pablo Tobón Uribe. Medellín, Colombia
(6) Gastrointestinal Surgeon and Endoscopist in the Gastro-hepatology Group at the Universidad de Antioquia and the Hospital Pablo Tobón Uribe. E-mail: rcastanoll@une.net.co
Received: 08-08-12 Accepted: 17-01-13
Abstract
Background: Biliary complications after liver transplantation are a serious cause of morbidity and mortality. Direct invasive cholangiography techniques, endoscopic retrograde cholangiography (ERCP) and percutaneous transhepatic cholangiography (PTC) all have procedure-related complications. Ultrasonography and magnetic resonance cholangiopancreatography (MRCP) are non-invasive, safe, and accurate. Objective: The aim of this study was to evaluate the use of US and MRCP for detecting biliary complications following liver transplanta- tion and compare these findings with those from the gold standard, ERCP. Methods: Between march 2006 and January 2009, twenty-seven consecutive liver transplant recipients at the Hospital Pablo Tobón Uribe in Medellín-Colombia who presented clinical and biochemical evidence of biliary complications were evaluated with US, MRCP and ERCP. Results: The presence of a biliary anastomotic complications was confirmed in 26 patients (92.6%), anastomotic biliary strictures in 24 (88.9%), ischemic or diffuse intrahepatic biliary strictures in two (7.4%), and choledocholithiasis in one (3.7%). All patients underwent ERCP, 25 underwent US (92, 5%) and 13 underwent MRCP (48, 1%). There was a statistically significant correlation for MRCP and ERCP findings, but not for US findings. The sensitivity of MRCP was 80% and its specificity was 50%. The sensitivity of US was 55.6% with 50% specificity. Positive and negative predictive values for MRCP were 92.3% and 25%, but for US were 93.7% and 7.8% respectively. Conclusions: MRCP is an accurate imaging tool for assessment of biliary complications after liver transplantation. We recommend that MRCP be the diagnostic imaging modality of choice in this setting, reserving direct cholangiography for therapeutic procedures.
Keywords
Orthotopic liver transplantation, ERCP, magnetic resonance, ultrasound, biliary stent.
INTRODUCTION
The first orthotopic liver transplantation (OLT) in Colombia and in Latin America was performed in Medellin on August 14 1979 (1). Since then the number of proce- dures performed in Colombia has been increasing. In 2007 979 organ transplants were performed in Colombia. Of these 193 were liver transplants representing 19.7% of all transplanted organs. Liver transplants occupied 2nd place after kidney transplants. The greatest number of these liver transplants, eighty-six, were performed in Medellin. Of these, forty-five, or 23.3% of the national total, were per- formed in the Hospital Pablo Tobón Uribe (2).
The first liver transplantation ever performed at the Hospital Pablo Tobón Uribe was done on February 12, 2004. As of August 2010, 276 OLTs had been performed on adults with a five year survival rate of 81.6% (3).
The main indications for liver transplantation in this insti- tution are non-biliary cirrhosis (68.6%), chronic cholesta- sis (15.7%), acute liver failure (5.9%) and retransplantation (5.4%). Perioperative complications occurred in 38.1% of patients. Complications included intraoperative bleed-ing (7.6%), hemoperitoneum (4.3%), neural confusion (2.7%) and acute renal failure (2.7%). The most frequent early complications, defined as those that occur in the first month, were renal failure (10%) and acute rejection (9%). The most frequent late complications, defined as those occurring more than one month after transplantation, were rejection (1.1%) and biliary complications (0.5%) (3).
Liver transplantation is the treatment of choice for patients with end-stage liver disease. Biliary complications after OLT are among the most important complications. They occur in between 5% and 25% of liver transplant recipients espe- cially during the first three months after surgery (4-6). Early detection of these complications is important for ensuring success of the procedure. However, because the clinical and laboratory indications are nonspecific, it becomes necessary to perform various diagnostic imaging tests for proper char- acterization and treatment (7). The prevalence of these com- plications makes it important to recognize which clinical or laboratory findings indicate complications of the biliary tract complications and to be able to characterize them with exist- ing techniques including ultrasound, Magnetic Resonance Imaging (MRI) and Endoscopic Retrograde Cholangio Pancreatography (ERCP).
The use of ultrasound as the first diagnostic test for biliary complications is universally described in the large liver trans- plantation referral centers (4). Ultrasound is followed by ERCP, although ERCP can cause morbidity and mortality and these procedures sometimes fail (8). MRIs have become easily accessible and quick alternatives which cause no mor- bidity and which have sensitivity and specificity comparable to those of ERCP. Until now, ERCP has been considered the gold standard for these patients (9,10).
Considering all of this, we believed it would be important to analyze the correlation of ultrasound, MRIs and ERCP for diagnosis of biliary complications in patients who had undergone liver transplantation at the Hospital Pablo Tobón Uribe.
MATERIALS AND METHODS
The following is a retrospective descriptive study evalu- ating findings of biliary complications through imaging in a series of 26 patients who had undergone orthotopic liver transplantation. The sample includes all patients who underwent liver transplantation from March 2006 to January 2009 for whom suspicions of biliary complications arose following various imaging tests.
The medical records in the hospital database of patients who had undergone transplantation were retrospectively reviewed. Records included demographic variables, dates and details of transplantations, dates and clinical manifesta- tions of biliary complications, imaging studies performed following biliary complications, the results of those studies, and treatments of complications.
Description of diagnostic methods
Ultrasound. Echography was performed with an Acuson Antares 5.0 Release and Spotlights ACUSON X150 Ultrasound System. The equipment includes a multi- frequency (between 3.5 and 7.5 MHz) sector transducer which can be used through the trans-abdominal approach. Livers and biliary tracts were evaluated for already described signs to determine if there were any complications related to transplantation. This study was performed by a radiolo- gist who is trained in body imaging.
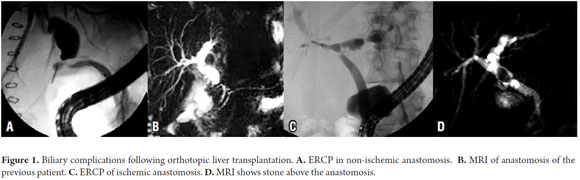
Endoscopic Retrograde Cholangio Pancreatography. ERCP was performed with Siemens AXIOM Luminos TF equipment for universal fluoroscopy. The biliary tract was evaluated under sedation and endoscopically treated when necessary (Figure 1A).
Magnetic Resonance Imaging (MRI). MRIs were per- formed with the Siemens Magnetom Avanto High-End 1.5 Tesla System. Simple contrasting and magnetic chol- angioresonance sequences were used to locate any signs of biliary tract alterations. These studies were interpreted by a radiologist from the body imaging area (Figure 1B).
Classification of Biliary Complications
- Non-ischemic or anastomotic stenosis: short single lesions, located at the site of anastomosis (Figures 1A and 1B).
Figure 1. Biliary complications following orthotopic liver transplantation. A. ERCP in non-ischemic anastomosis. B. MRI of anastomosis of the previous patient. C. ERCP of ischemic anastomosis. D. MRI shows stone above the anastomosis.
- Nonanastomotic or ischemic stenosis: multiple lesions or diffuse hilar intrahepatic dominance (Figure 1C).
- Bile leak: bile drainage outside of the biliary duct, either at the site of the anastomosis or elsewhere.
- Other complications: lithiasis (Figure 1D), bilomas and Sphincter of Oddi dysfunction.
Complications that occurred during the first 30 days after OLT were classified as early while those which occurred after the first 30 days were classified as late.
Statistical Analysis
Statistical analysis was performed with SPSS 17® and Epidat pro- grams. The population was initially described using descriptive statistical tools taking into account the type of variable. Absolute and percentage frequency distributions were used for qualitative variables, and summary measures of dispersion and central tendency were used for quantitative variables.
Concordance analysis using the Kappa statistic was applied to assess the accuracy between the tests. Results of each test were read within a maximum of in order to avoid differences in test results due to changes in the pathophysi- ological characteristics of patients. Kappa coefficient analy- sis was based on concordance proportions unattributable to chance. The closer a result was to one, the better the result was judged to be.
Finally we compared ultrasound and MRI to ERCP by calculating sensitivity, specificity, positive and negative pre- dictive values, and likelihood ratios, a validity index and the Youden index.
Ethical Issues
This study meets the ethical requirements set out in Republic of Colombia Law 23 of 1981 and those established in Health Ministry Resolution No. 008430 of 1993 which set out the scientific, technical and administrative standards for health administration involving human participation.
RESULTS
From February 2004 to August 2010 276 liver transplan- tations were performed on adults with cadaveric donors at the Hospital Pablo Tobón Uribe in Medellin. In this retros- pective analysis 27 patients with biliary complications were documented for an incidence of 9.78%.
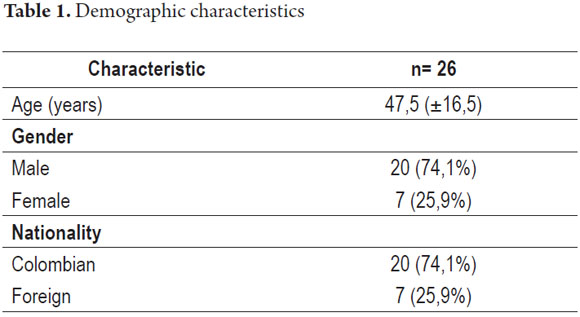
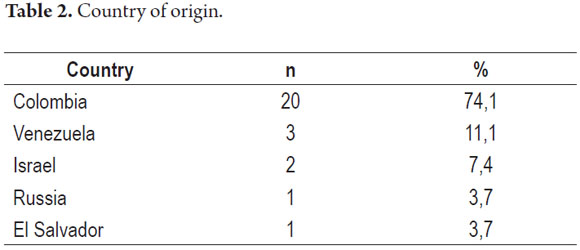
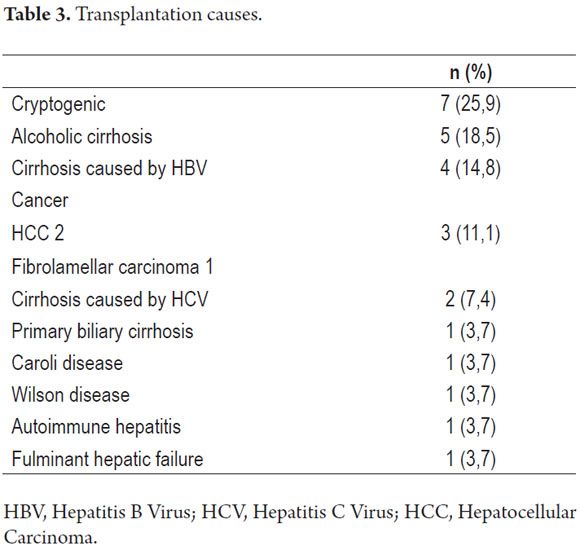
Of the patients included in the study 20 were men (74.1%) and 7 were women (25.9%). Their average age was 47.6 years (range 13-71 years). The Hospital Pablo Tobón Uribe is a national and international reference center for this type of procedures. Twenty patients (74.1%) were Colombians and seven patients were foreigners (Tables 1 and 2). The reasons for liver transplantation are shown in Table 3.
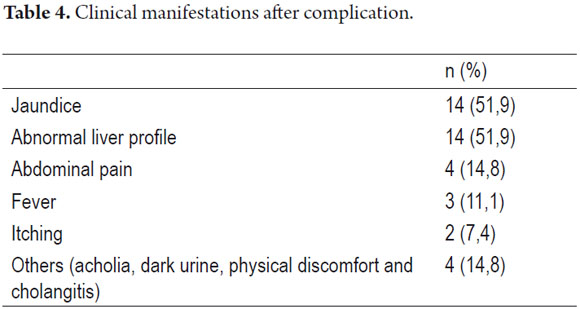
The most important clinical symptoms that led to chec- king patients for biliary complications following OLT were jaundice and abnormal liver profiles. Both were found in 14 patients (51.9% each). Other causes are specified in Table 4.
The time elapsed from transplantation until diagnosis of a complication varied from 1 to 1,786 days with a mean of 230.3 days (7.7 months). Twelve cases (44%) occu- rred within the first month after transplantation; six cases (22.2%) occurred between the first and third month after transplantation and 9 cases (33.3%) occurred after the third month of transplantation.
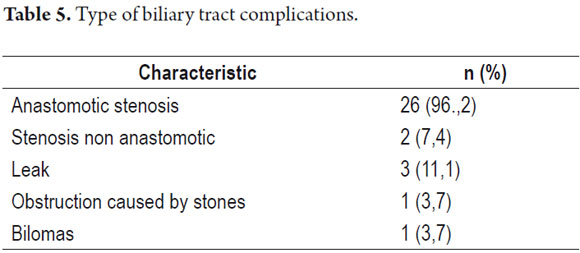
At the moment ERCPs were performed, there were 26 cases (96.2%) of anastomotic stenoses of which 2 (7.4%) were of ischemic origin. None of the documented steno- ses were non-anastomotic. There were 3 cases (11.1%) of bile leakage which were all associated with biliary stenoses. There was one case of ischemic stenosis with associated bilomas. There was one case (3.7%) of obstruction at the anastomosis site caused by biliary stones without stenosis (Table 5).
Twenty-six cases (96.2%) cases were treated with ERCP with biliary stents two of which used balloon dilation prior to stent placement. One patient (3.7%) was treated with only balloon dilatation. None of the patients required per- cutaneous procedures.
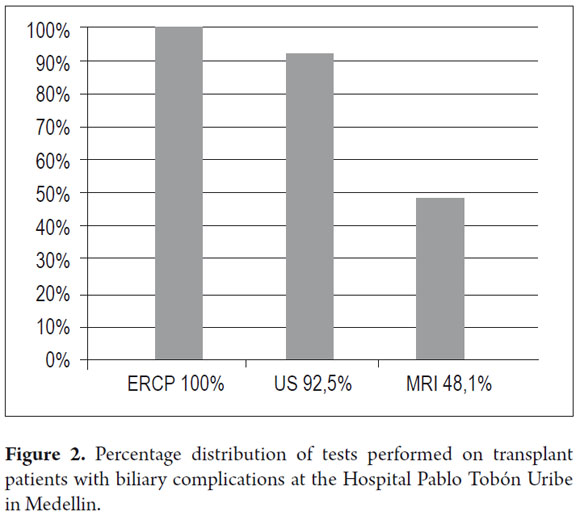
ERCP was the gold standard for diagnosing complica- tions: it was used for all patients. Ultrasound was used for 25 patients (92.5%) and cholangioresonance was used for 13 patients (48.1%) (Figure 2).
Of the 13 MRIs performed, four (30.8%) showed anasto- motic stenosis as their sole findings; three (23.1%) showed dilatation of the intrahepatic bile ducts as their sole fin- ding; four (30.8%) showed both findings and two (15.4%) showed no pathological findings in the bile duct. In total, MRIs showed pathological findings in the bile ducts of eleven patients (86.4%).
In the concordance analysis we found a Kappa of 0.699 indicating good concordance between MRIs and ERCPs since this value is between 0.6 and 0.8.
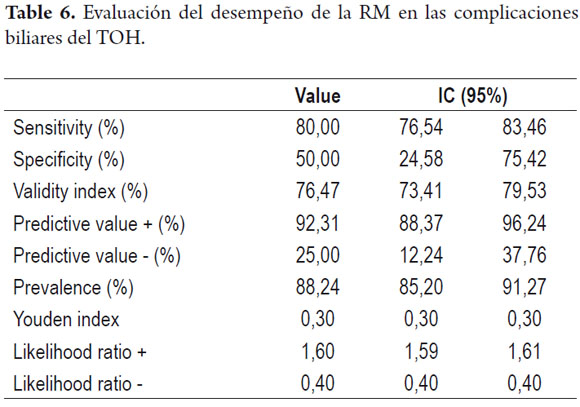
MRIs showed a sensitivity of 80% (76.54-83.46), a spe- cificity of 50% (24.58-75.42), a positive predictive value of 92.31% (88.37-96.24), a negative predictive value of 25% (from 12.24 to 37.76), a validity index of 76.47% (73.41- 79.53), a positive likelihood ratio of 1.60 (1.59-1,61) and a negative likelihood ratio of 0.40 (0.40 - 0.40) (Table 6).
MRI sensitivity was 80%. However, for every 100 patients with complications, MRIs indentify approximately 50 as being without complications.
MRIs' positive predictive value was 92.3%, while the negative predictive value was 25. This means that for every 100 patients who test negative for complications with MRIs, approximately 25 are really negative.
The difference between the true positive and false posi- tive rates (Youden index) was 0.3 (0.30 - 0.30). This value is closer to the expected value. It should be close to 1.0 to be considered a perfect test for comparison with ultrasound. The proportion of individuals correctly cassified (validity index) was 76.5 (73.41 - 79.53).
The positive likelihood ratio (LR) for ultrasound was 1.60 (1.59 - 1.61) which means that it is 1.60 times more likely that magnetic resonance will be positive in sick patients than in patients who are not sick. The negative LR was 0.40 (0.40 -0.40) which means that the probability of a negative result is 2.5 times higher in patients who are not sick than in sick patients (1/0.40 = 2.5).
Eight patients (66.6%) were found to have anastomotic anastomosis with MRIs.
Two patients (15.4%) for whom MRIs and ultrasound showed no pathological findings in the bile ducts were found to have anastomotic stenoses when they underwent ERCPs.
Of the 13 patients who underwent MRIs 12 (92.3%) also underwent ultrasound. Ultrasound found no compli- cations in nine of these patients (69.2%), showed dilation of the intrahepatic bile duct in three patients (23.1%), showed arterial stenosis in one case (7.7%) and showed splenomegaly and mild ascites in another case (7.7%). The concordance analysis found a Kappa of 0.1295 (p-value = 0.3711) which indicates is a moderate match between ultrasound and MRIs since this value is between 0 and 0.2. The three patients for whom bile leakages were found with ERCPs were also evaluated with ultrasound which showed that two of them had mild ascites and one had bilomas. None of these patients underwent MRIs.
The patient who was diagnosed with stones at the site of the anastomosis did not undergo an MRI. This patient underwent ultrasound which reported intrahepatic and extrahepatic dilation of the bile duct.
Of the 25 patients who underwent ultrasound 14 (56%) reported dilated intrahepatic bile ducts. Four of these also had dilated extrahepatic bile ducts. It was not possible to determine the site of the biliary stenosis by this method. ERCPs showed the anastomotic stenoses in all cases. Eleven (44%) patients did not show abnormalities of the bile duct in their ultrasound studies, but three (12%) of these 11 patients showed mild ascites. Concordance (correlation) between ultrasound and ERCPs was low: its value was bet- ween 0.21 and 0.40 with a Kappa value of 0.2535 (p-value = 0.8788).
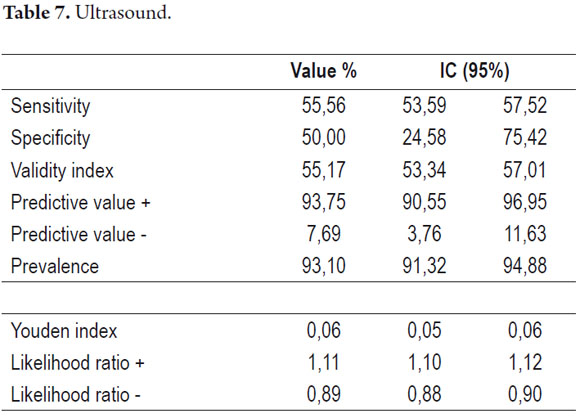
Ultrasound had a sensitivity of 55.56% (53.59-57.52), a specificity of 50% (24.58 - 75.42), a positive predictive value of 93.75% (90.55 -96.95), a negative predictive value of 7.69% (3.76-11.63) a validity index of 55.17%, a positive likelihood ratio of 1.11 (1.10-1.12) and a negative likeli- hood ratio of 0.89 (0.88 to 0.90) (Table 7).
Ultrasound's sensitivity was 55.6%. For every 100 patients who do not show biliary duct complications with ultrasound, about 50 really do not have complications.
The positive predictive value of ultrasound was 93.8% while the negative predictive value was only 7.7 (3.76-11.63). In other words this is the probability that patients who show no complications really have no com- plications, or that out of 100 patients who show no com- plications with ultrasound, approximately 7 really have no complications.
The difference between the true false positive rates (Youden index) was 0.06 (0.05 -0.06), a value that is far from the expected value that should be close to 1 to be con- sidered as a perfect test. The proportion of correctly classi- fied individuals (validity index) was 55.2% (53.34-57.01).
The positive likelihood ratio (LR) for ultrasound was 1.11 (1.10-1.12) which means that it is 1.11 times more likely that ultrasound will be positive for sick patients than for patients who are not sick. The negative LR was 0.9 (0.88 - 0.90) which indicates that the probability of a nega- tive result is 1.12 times higher for patients who are not sick patients than for sick patients (1/0.89 = 1.12).
Ultrasound found three additional cases of ascites (12%), one patient with splenomegaly (4%) and one patient with arterial stenosis (4%).
In a comparative analysis of the Kappa values with the chi-square test a significant statistical difference (p = 0.000) was found between MRIs and ultrasound. The ove- rall kappa value obtained was 0.6994 (CI 0.6994 - 0.6994).
DISCUSSION
Despite advances in surgical techniques, graft preservation, immunosuppression, and intensive care, biliary duct complications following OLTs continue to occur frequently (11) and represent a significant risk of morbidity. They can cost the loss of a graft and the life of the patient (4).
The incidence of 9.8% demonstrated in the study popu- lation analyzed is within the range of 5% to 25% described in the literature worldwide (3). Variations in incidences are associated with local factors in surgical technique and ischemia times involved in results.
Diagnosis of biliary stenosis following OLT should be done early to avoid unfavorable outcomes. The overlap between laboratory findings and clinical manifestations of various complications such as graft rejection or anastomo- tic stenosis requires diagnostic imaging to help differentiate among complications. The need for rapid diagnosis should be balanced against the risks of invasive methods. To achieve this, US and MRIs were used before ERCPs even though the value of these methods in relation to ERCP has not yet been established.
A good quality metaanalysis has evaluated 67 studies. It found a sensitivity of 97% and a specificity of 98% for MRI diagnoses of biliary stenoses (12). Nevertheless, this metaanalysis did not specifically evaluate biliary stenosis following OLT which leaves uncertainty about the utility of this method for evaluating these patients.
Although one study suggests comparable sensitivities and specificities for US and MRIs in evaluation of choledocho- lithiasis for anastomotic or intrahepatic biliary stenosis (13), MRIs are superior to US. MRIs also have the advantage of properly locating stenoses which allows for planning of treatment. This is especially useful for patients with separate biliary stenoses which occur most frequently following trans- plantation from living donors to either children or adults (9).
A recent metaanalysis which compared the use of ERCPs and MRIs for diagnosis of biliary obstructions following OLTs (14) showed some promising results for MRI. These findings were ratified in another recent evaluation by Pecchi (10) and Katz (15). Nevertheless, the type of biliary reconstruction following OLT influences the accuracy of the evaluation. Choledochus-choledochus reconstruction was used for all of our patients rather than bilioenteric anastomosis, and MRI findings are less accurate at the bilioenteric derivations (16).
Although initial studies favored the use of ERCPs over MRIs for typifying biliary stenoses (17), the development of equipment with higher resolutions and MRI management by better trained personnel who have specific techniques for these diseases have transformed MRIs the currently prefe- rred noninvasive method for evaluating the bile duct (18).
An evaluation of the correlation between the locations of stenoses seen with ERCP and those identified in MRIs in this present series shows that MRIs identified the exact locations of stenoses in 61.5% of the cases. The correlation between MRI findings and those of the gold standard ERCP for pathological findings in the biliary duct in general shows a concordance of 85.7% and a kappa value of 0.6994.
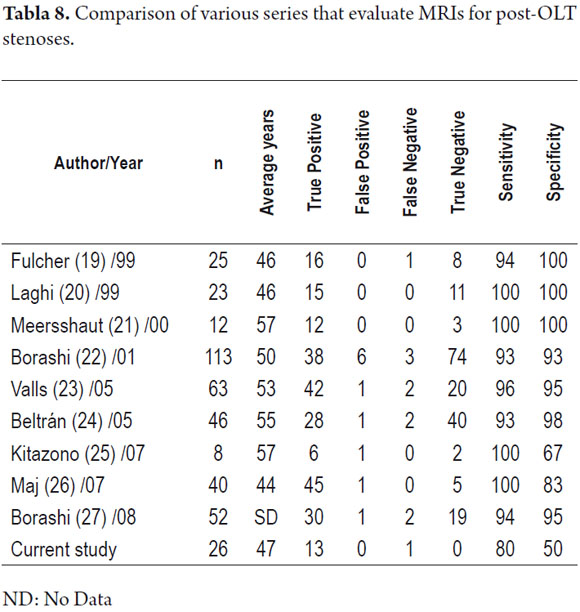
The correlation of pathological findings in the biliary duct between ultrasound and ERCPs had low kappa values while the correlation of ultrasound findings with those of MRIs had moderate kappa values. It can be inferred that an ultrasound report showing no complication does not rule out the possibility of a complication in the biliary duct in these patients. This does not create any added value for diagnosis of biliary duct complications in patients following liver transplantation because the overall kappa is not greater than the individual kappa on these tests. Even though ultrasound shows no value for diagnosis of biliary duct complications in patients following liver transplanta- tions, it is a suitable method for visualizing other findings, especially vascular disorders that threaten the viability of the graft. These findings are similar to those reported in various series in the medical literature (Table 8).
In this study we evaluated the diagnostic capacity of ultrasound and MRIs with respect to the gold standard ERCP. MRIs were found to have greater capacity diagno- sing biliary complications following OLTs than US. This diagnostic accuracy together with the fact that MRIs and ultrasound are noninvasive procedures justifies the syste- matic use of US and MRIs when there is clinical and/or laboratory suspicion of biliary stenosis following an OLT. In addition, MRIs allow safe location of stenoses and plan- ning of treatment.
CONCLUSIONS
- Clinical criteria can neither dismiss nor confirm bile duct complications in patients following liver trans- plantation with certainty. As described, some patients may be asymptomatic or present bizarre symptoms. The cholestatic profile could be used for initial scree- ning of these patients.
- Ultrasound represents the first step in diagnosis, but a negative ultrasound does not rule out bile duct com- promise. When there is diagnostic suspicion an MRI may be the diagnostic method to use given the high PPV of this test.
- Ultrasound did not show appropriate values of repro- ducibility and validity with the data used in this study which suggests that this test should be evaluated in studies with larger samples which might better support ultrasound's utility for detecting complications of the bile duct.
- Because ERCP is an invasive method with widely known complications, the use of MRIs is emerging as an important tool for diagnosis of biliary complica- tions in patients following OLTs. This is also suppor- ted by the fact that MRI showed better reproducibility (Kappa) and better validity (sensitivity and specificity) than ultrasound in this study.
- ERCP remains the gold standard for biliary duct compli- cations because it allows both diagnosis and treatment. However, MRIs provide more extensive information which allows diagnosis of other diseases. Consequently it should be considered a complementary test.
- Ample use of MRIs will lead to greater experience. As described above only 48% of the patients studied underwent diagnostic MRIs.
- The small number of patients in this study requires that prospective studies be performed. This study should be considered a base for those studies.
1. Restrepo J, Velásquez A, Aristizábal H, et al. Experiencia con trasplante hepático en humanos. Cirugía 1986; 1: 67-72. [ Links ]
2. Instituto Nacional de Salud. Estadísticas trasplantes. http://www.insgovco/indexphp?idcategoria=6746 Acceso noviembre 2011. [ Links ]
3. Muñoz OG, Insuasty MR, Marín JI, et al. Complicaciones de la vía biliar después de trasplante ortotópico de hígado: Experiencia en el Hospital Pablo Tobón Uribe - Medellín. Rev Col Gastroenterol 2011; 26: 9-14. [ Links ]
4. Ryu CH, Lee SK. Biliary strictures after liver transplantation. Gut and liver 2011; 5: 133-42. [ Links ]
5. Krol R, Karkoszka H, Ziaja J, et al. Biliary complications after orthotopic liver transplantation: a 5-year experience. Transplant Proc 2011; 43: 3035-8. [ Links ]
6. Chang TI, Ho MC, Wu YM, Lee PH, Hu RH. Biliary complications after liver transplantation: an 18-year single-center experience. J Formos Med Assoc 2011; 110: 183-9. [ Links ]
7. Gunawansa N, McCall JL, Holden A, Plank L, Munn SR. Biliary complications following orthotopic liver transplantation: a 10-year audit. HPB (Oxford) 2011; 13: 391-9. [ Links ]
8. Kobayashi N, Kubota K, Shimamura T, et al. Complications of the treatment of endoscopic biliary strictures developing after liver transplantation. Journal of hepato-biliary-pancreatic sciences 2011; 18: 202-10. [ Links ]
9. Beswick DM, Miraglia R, Caruso S, et al. The role of ultrasound and magnetic resonance cholangiopancreatography for the diagnosis of biliary structure after liver transplantation. European journal of radiology 2011. [ Links ]
10. Pecchi A, De Santis M, Gibertini MC, et al. Role of magnetic resonance imaging in the detection of anastomotic biliary strictures after liver transplantation. Transplant Proc 2011; 43: 1132-5. [ Links ]
11. Scarborough JE, Desai DM. Treatment options for biliary complications after orthotopic liver transplantation. Current treatment options in gastroenterology 2007; 10: 81-9. [ Links ]
12. Romagnuolo J, Bardou M, Rahme E, Joseph L, Reinhold C, Barkun AN. Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Annals of internal medicine 2003; 139: 547-57. [ Links ]
13. Cohen C, Elion RA, Frank I, et al. Once-daily antiretroviral therapies for HIV infection: Consensus Statement of an Advisory Committee of the International Association of Physicians in AIDS Care. J Int Assoc Physicians AIDS Care (Chic) 2002; 1: 141-5. [ Links ]
14. Jorgensen JE, Waljee AK, Volk ML, et al. Is MRCP equivalent to ERCP for diagnosing biliary obstruction in orthotopic liver transplant recipients? A meta-analysis. Gastrointest Endosc 2011; 73: 955-62. [ Links ]
15. Katz LH, Benjaminov O, Belinki A, et al. Magnetic resonance cholangiopancreatography for the accurate diagnosis of biliary complications after liver transplantation: comparison with endoscopic retrograde cholangiography and percutaneous transhepatic cholangiography - long-term follow-up. Clin Transplant 2010; 24: E163-9. [ Links ]
16. Kinner S, Dechene A, Paul A, et al. Detection of biliary stenoses in patients after liver transplantation: is there a different diagnostic accuracy of MRCP depending on the type of biliary anastomosis? Eur J Radiol 2011; 80: e20-8. [ Links ]
17. Zoepf T, Maldonado-Lopez EJ, Hilgard P, et al. Diagnosis of biliary strictures after liver transplantation: which is the best tool? World journal of gastroenterology : WJG 2005; 11: 2945-8. [ Links ]
18. Shanmugam V, Beattie GC, Yule SR, Reid W, Loudon MA. Is magnetic resonance cholangiopancreatography the new gold standard in biliary imaging? The British journal of radiology 2005; 78: 888-93. [ Links ]
19. Fulcher AS, Turner MA. Orthotopic liver transplantation: evaluation with MR cholangiography. Radiology 1999; 211: 715-22. [ Links ]
20. Laghi A, Pavone P, Catalano C, et al. MR cholangiography of late biliary complications after liver transplantation. AJR American journal of roentgenology 1999; 172: 1541-6. [ Links ]
21. Meersschaut V, Mortele KJ, Troisi R, et al. Value of MR cholangiography in the evaluation of postoperative biliary complications following orthotopic liver transplantation. European radiology 2000; 10: 1576-81. [ Links ]
22. Boraschi P, Braccini G, Gigoni R, et al. Detection of biliary complications after orthotopic liver transplantation with MR cholangiography. Magnetic resonance imaging 2001; 19: 1097-105. [ Links ]
23. Valls C, Alba E, Cruz M, et al. Biliary complications after liver transplantation: diagnosis with MR cholangiopancreatography. AJR American journal of roentgenology 2005; 184: 812-20. [ Links ]
24. Beltran MM, Marugan RB, Oton E, Blesa C, Nuno J. Accuracy of magnetic resonance cholangiography in the evaluation of late biliary complications after orthotopic liver transplantation. Transplant Proc 2005; 37: 3924-5. [ Links ]
25. Kitazono MT, Qayyum A, Yeh BM, Chard PS, Ostroff JW, Coakley FV. Magnetic resonance cholangiography of biliary strictures after liver transplantation: a prospective double-blind study. Journal of magnetic resonance imaging. JMRI 2007; 25: 1168-73. [ Links ]
26. Maj E, Cieszanowski A, Golebiowski M, et al. The role of MR cholangiography in the detection of biliary complications after orthotopic liver transplantation. Polish J Radiol 2007; 72: 25-31. [ Links ]
27. Boraschi P, Donati F, Gigoni R, et al. Complications after liver transplantation: evaluation with magnetic resonance imaging, magnetic resonance cholangiography, and 3-dimensional contrast-enhanced magnetic resonance angiography in a single session. Canadian Association of Radiologists journal = Journal l'Association canadienne des radiologistes 2008; 59: 259-63. [ Links ]











 text in
text in