Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.2 Bogotá abr./jun. 2013
Microbiological conditions for culturing Helicobacter Pylori
Martín Alonso Bayona Rojas, Bact., Esp., M. Sc. (1)
(1) Professor in the Applied Biomedical and Genetics Research Group (GIBGA - Grupo de investigaciones Biomédicas y de Genética Aplicada) of the Faculty of Medicine Universidad de Ciencias Aplicadas y Ambientales in Bogotá, Colombia. Mail: mabayona@udca.edu.co
Received: 17-09-12 Accepted: 16-04-13
Abstract
Early diagnosis and culturing of Helicobacter pylori are of great importance for the study of the growth characteristics of these bacteria which can contribute to knowledge of classical and molecular epidemiology, genetic diversity and susceptibility to antibiotics. The ubiquity and importance of this pathogen throughout the world has forced us to consider and propose effective routine alternatives for isolating and identifying these bacteria in microbiology laboratories. This review was conducted to describe the literature concerning the conditions for cultivation of this organism in the laboratory.
Key words
Helicobacter pylori, microbiology, isolation, microbial culture.
BACKGROUND
It is estimated that H. pylori infects between 50% and 75% of the world's population. Of every 10 people infected with this microorganism, only one develops the disease: 9 never develop it. The infection is associated etiologically with the presence of gastric or duodenal peptic ulcers and with the development of mucosa-associated lymphoid tissue (MALT). H. pylori participate in the multi-causal etiological chain leading to gastric cancer (1). In fact, the World Health Organization (WHO) has classified H. pylori as a Group 1 biological and carcinogenic agent for the human population with the highest incidence of infection during childhood in developing countries. This is apparently related to unfavorable economic, hygiene and sanitary conditions (2, 3). Diverse levels of virulence are apparently primarily related different strains of the bacteria, but are also associated with other factors such as ethnic origin, undernourishment, overcrowding, geographic location and age (4).
This paper reviews microbiological issues related to culturing H. pylori and factors implicit in it. Our bibliographic searches explored online databases including Medline, Proquest, Embase, Jstore, Pubmed, Hinary, Springer, Nature, Science Online and the Oxford Journal. We also searched in particular journals including Plos, Nas and Imbiomed. Our search terms combined Helicobacter and maintenance, supplements for Helicobacter, laboratory maintenance, culture on solid medium and susceptibility to antibiotics.
One Colombian study done by the Universidad Del Valle and sponsored by the Instituto Colombiano para el Desarrollo de la Ciencia y la Tecnología reported a 69.1% prevalence of H. pylori infections in regional hospitals in 16 Colombian Departments. This finding was determined from biopsies from upper digestive endoscopies. In previous decades research into causes of acid peptic disease and gastric adenocarcinoma focused principally on dietary factors, but the discovery that H. pylori is a frequent gastric pathogen has changed etiological ideas about these and others gastroduodenal diseases (5).
Since the study of H. pylori in our country began at the end of the last decade, there are few reports of laboratory experiences with the microbiological capacities necessary for its isolation and culture (6).
MICROBIOLOGICAL CHARACTERISTICS
The members of the Helicobacter genus were described in 1989. They colonize the stomach and intestines of human and some animal species. Helicobacter is a Gram-negative microaerophilic curved bacillus that possesses an outer membrane and 4 to 8 polar flagella protected by a lipid structure. They produce urease, catalase and cytochrome oxidase. Urease increases bacterial virulence of H. pylori since it transforms urea into NH3 and H20 which alkalinizes the surrounding acid. Other factors are lipase, adhesins, catalase, platelet activator factor, cytotoxin-associated gene A (Cag A), pic B (which induces cytokines) and the vacuolating cytotoxin A (VacA) (3, 7).
Samples for culturing are obtained from gastric mucosa. Extra-gastric samples are obtained from dental plaque, the rectum, the bladder and the esophagus. The time required for formation of colonies ranges from 4 to 7 days in conditions of 5% to 10% O2, 5% to 10 % CO2, and 80% to 90% N2 with 95% humidity and 35o to 37 o C temperature. Usually this microorganism is cultured in blood serum and antibiotics (7).
CONDITIONS FOR TAKING SAMPLES
The protocol recommended for taking sample from biopsies of patients with chronic gastritis is that proposed by the Sidney system. It is important to remember that H. pylori are predominantly found in the pyloric antrum of the stomach except for individuals treated with IBP and H2 receptor antagonists who have greater densities in the corpus. Five biopsies must be taken: one sample each from the greater and lesser curvatures of the antrum from points two to three centimeters from the pylorus, one sample each from the greater and lesser curvatures of the corpus from points eight centimeters from the cardia, and one from the angular incisure (8). By employing this protocol it is possible to detect the bacteria in almost every infected individual (9). Taking samples for biopsies is an almost painless procedure for patients, but this procedure must be done by an expert gastroenterologist who follows ethical and medical protocols. This procedure is not recommended for patients with bleeding ulcers because it can cause hemorrhaging. All studies should be approved by an ethics committee and have clearly written signed informed consent forms.
Other types of samples are also used. They include as gastric acid obtained from a string test and samples isolated from vomit which provide different results. H. pylori have also been cultured from extra-gastric samples from dental plaque, the esophagus, the rectum and the urinary bladder.
Other important issue is whether a patient has previously been treated with antibiotics. In such a case a patient must wait at least 4 weeks for testing in order to get successful results from a culture. Although forceps used to take biopsies must be disinfected to prevent contamination between patients, excessive disinfection could affect the viability of bacteria.
Biopsy samples must be ground or pulverized and mixed together with a small amount of saline solution. Then a loop is used to spread the sample over the surface of the medium. The sample material is streaked with the loop in a series of parallel lines onto different segments of the plate (8, 9).
Samples must be processed quickly because the microorganism is sensitive to the environment. Samples taken from the antrum and corpus should be introduced into sterile test tubes with 0.5 ml of saline solution. They can remain there for a maximum of 6 hours. In case of delays, the use of transport media such as Stuart medium is recommended. These samples should be stored at 4o to 8 °C for no longer than 24 hours before processing. Next, the sample should be homogenized and duplicates should be cultured in different kind of media. Culture media that can be used include Brucella broth and agar, BHI, Muller Hinton, Columbia agar and trypticase soy agar. These are generally supplemented with Fetal Bovine Serum, lysed erythrocytes, yeast extract, peptone and cyanobacteria. 7% to 10% horse, lamb or rabbit blood is generally added. Among the antibiotics that are added are vancomycin, sulfamethoxazole, trimethoprim, cefsulodin and polymyxin B antibiotics. Samples can be preserved in trypticase soy broth or BHI plus 20% glycerol. They can be stored in a freezer at -80o C or in liquid nitrogen (10, 11, 12).
CULTURING
The utility and importance of H. pylori culturing resides in the knowledge gained about the bacteria's growth characteristics, genetic diversity, epidemiology and about the possibility of determining its resistance to antibiotics used in treatment (7, 13).
Tersterman et al. (2001) described the use of a defined substrate, Hams F-12, employed for mammal cell cultures. Modifications were made to isolate H. pylori. These consisted in supplementing the substrate with B-cyclodextrin, cholesterol and fetal bovine serum without blood (which would have made it more costly). Blood agar plates were used to culture biopsies and reference strains of H. pylori. Culture growth was successful in 100% of these cases (14).
In 2010 Joo et al. established a thin layer liquid culture for recovering H. pylori. They first added Brucella broth to 90 mm diameter Petri dishes, and then added equine serum, yeast extract and dimethyl-beta-cyclodextrin. After about 3.3 hours growth was observed. It continued to grow exponentially for 28 hours (15).
In 2000 Stevenson et al. proposed an alternative culture in which the base components were Columbia agar and a mix of antibiotics including vancomycin, amphotericin b, trimethoprim and cefsulodin which inhibit the growth of other kinds of bacteria. In addition the medium was supplemented with horse blood, meat extract, agar, and corn starch (16).
When samples from the pyloric antrum and gastric fundus were cultured in Columbia agar plus 7% defibrinated lamb's blood and DENT supplement (vancomycin, trimethoprim, amphotericin b, and cefsulodin), 100% specificity was obtained turning this into the gold standard method (17).
Successful Helicobacter culturing requires use of fresh lamb or horse blood in the agars employed. Commercially prepared culture media can work, but their freshness is difficult to verify. Frequently they are old or dry, and they may not have the appropriate selection of antibiotics. When agars are prepared, they must not be used immediately. They must be stored inside of sealed plastic bags at 4o C for no more than 3 weeks (7). Our research confirms that the optimal conditions are found with the use of Brucella agar plus 8% horse blood at 4o C for a maximum time of 20 days.
In 2008 a study by Yepes et al. determined the resistance of H. pylori in patients of the gastroenterology department of the Hospital Universitario San Ignacio (HUSI). Samples obtained were initially transported inside of sterile screw cap tubes and frozen at -700 C for a maximum period of 3 weeks. Then, the sample was thawed and cultivated in Brucella agar supplemented with 5% lamb's blood. Samples were incubated for 5 days in humid microaerophilic media at 370C (18).
The results of our comparison of two transport media, Mueller Hinton broth supplemented with cyanobacteria extract (MH-CE) and Mueller Hinton broth supplemented with fetal calf serum (MH-FCS), showed that after 48 hours at room temperature more bacteria was recovered using MH-CE than was recovered with MH-FCS (p≤0.005). The MH-CE medium is simple and cheap, and it can be used to preserve the viability of H. pylori from biopsies (19).
In 2010 Trespalacios et al. isolated and identified H. pylori from gastric biopsies which were macerated in a 1% activated charcoal solution to obtain homogeneous solutions. Samples were then cultured in a modified Wilkins Chalgren medium supplemented with Isovitalex and antibiotics and incubated under anaerobiotic conditions at 37 0C for 4 to15 days. This method resulted in 80% H. pylori recovery (20).
In 2005 Quiroga et al. cultured samples from biopsies obtained from patients with gastroduodenal diseases which were macerated in aseptic conditions and then cultured in Lab M H. pylori medium supplemented with 8% horse serum, 1% Isovitalex and selective supplement for Campylobacter (Merck). The authors reported good results for H. pylori recovery (21).
Growing H. pylori in vitro requires media such as Brucella broth or agar supplemented with vitamins and horse serum or cyclodextrins. Liquid media generally produce slow growth, but optimum growth of H. pylori can be obtained by replacing the serum or cyclodextrins with a commercially available cholesterol solution which makes this medium an alternative for H. pylori recovery from clinical samples (22).
In 2001 Majalca et al. evaluated a base media of gelose and chocolate (GC) to which was added 2% freeze dried hemoglobin, Campylobacter agar, Casman agar, Columbia agar, brain-heart infusion agar, Brucella agar, Mueller Hinton agar or trypticase soy agar. Each mixture was supplemented with 7% to 10% of horse or lamb blood plus antibiotics (with or without nicotinamide-adenine) to a final concentration of 15 ug/mL. A microaerophilic environment was generated using system sachets and 3 Alka-Seltzer tablets in 10 mL of water. All of these components were placed inside of a flask sealed with plastic paraffin film with or without the use of a candle. The strains were stored at -70 0C using Brucella broth plus 10% horse serum, 25% glycerin and horse blood as well as Brucella broth plus 10% fetal bovine serum and 30% glycerol. It is important to highlight that the microaerophilic environment was obtained with 3 Alka-Seltzer tablets. The best medium in terms of H. pylori recovery was Casman agar with 7% horse blood for 5 to 7 days, and the best medium for preservation was the Brucella broth with 2% fetal bovine serum (23).
The sensitivity of a culture medium changes in relation with variables such as collection, transport, and storage of the sample, the culture medium itself, and incubation conditions. In 2007Navarro et al. evaluated an ecometric method for three culture media: trypticase soy agar, BHI agar and Brucella agar. All three media were supplemented with 5% lamb's blood. Low levels of H. pylori recovery with all of the three media were correlated with an absolute growth index (AGI) below 2.5. This result indicates that none of the media tested have good capacity for H.pylori recovery which is explained by the low blood concentration and absence of nutrients such as Isovitalex (24).
Growing H. pylori without serum remains difficult since nutritional requirements are only partially understood. Amino acids, metals, sodium chloride for iron, zinc and magnesium are critical for growth, but copper is not necessary. These data indicate that H. pylori and other Helicobacter species are not as demanding as was thought. The data also suggest that the chemical media described here could generate the growth from a variety of Helicobacter species which would allow researchers to develop a more detailed characterization of their physiologies and interactions with host cells (25).
In 2010 Mcnulty et al. evaluated three selected media: PYL from bioMérieux in France; Helicobacter agar from Beckton Dickinson in the United States, and Brugman Helicobacter Agar. They found no significant differences in the number of colonies grown or in recovery rates. They observed the presence of typical colonies which were identified through Gram staining and catalase, oxidase, urease and other biochemical tests (27).
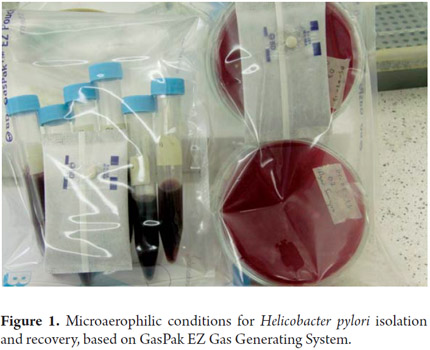
My experience as a member of GIBGA (Grupo de Investigaciones Biomédicas y de Genética Aplicada Applied Biomedical and Genetics Research Group) with H. pylori recovery from gastric biopsies has led me to establish and recommend a transport medium with selective enrichment. That medium contains Campylobacter broth plus 2% Isovitalex, 8% whole horse or lamb blood, 0.1% trimethoprimsulfamethoxazole, 0.1% vancomycin, 0.1% penicillin and 0.1% amphotericin. This medium is incubated at 370 C for 3 to 5 days. Colonies are observed after 18 hours of incubation in anaerobiotic conditions. Anaerobiotic conditions are generated using the BD GasPak EZ Gas Generating Container System (Ref 260683) which is a sachet system (Figure 1). After incubation samples are isolated in media such as Brucella agar and chocolate agar supplemented with the ingredients previously mentioned in the transport and enrichment medium. The methods for recovery from broth and solid media recommended by the author have been evaluated with a reference strain of H. pylori NCTC 11638 (strain donated by Dr. Alba Alicia Trespalacios from Universidad Javeriana).
To confirm the purity of every strain obtained, each is tested with gram staining and oxidase, catalase, and urease tests as well as genotyping of the 16s ribosomal gene. We observe a biofilm in a liquid culture medium which has as important characteristic that promotes genetic interchanges. This phenomenon boosts generation of strains that are more virulent and resistant to extreme environments (28, 29).
ANTIBIOGRAMS
The method approved by the Clinical and Laboratory Standards Institute (CLSI) for evaluation of the sensitivity of H.pylori to antibiotics is an agar dilution antibiotic method (28). On the other hand, the British Society for Antimicrobial Chemotherapy (BSAC) recommends the E-test which has a good correlation with the referenced method (10).
To test sensitivity, we use Muller Hinton agar supplemented with 5% lamb's blood. The inoculum is prepared in a 0.85% saline solution and compared to a MacFarland standard No. 2 test tube (1x107 a 1x108 UFC/mL). To obtain the inoculum, the strain should be taken from a subculture made from blood agar incubated for 72 hours. As second alternative is to taket the sample from an H. pylori culture in Brucella broth adjusted to the MacFarland standard (1x108 UFC/mL). This inoculum is spread in Mueller Hinton agar supplemented with 10% horse serum and 2% Isovitalex (20).
Because the method of diluting in agar is not routinely applicable, and because the E- test is expensive and has discrepancies with metronidazole, in 2002 McNulty reviewed studies with the disk-diffusion method and recommended the following disk concentrations and cut off points:
1. For metronidazole use a 5 µg disk. Bacteria are considered resistant if the halo is less than 16mm in diameter, intermediate if the halo is between 16 and 21 mm in diameter, and sensitive if the halo is greater than 21 mm in diameter. In cases of intermediate sensitivity it is recommended to also use a minimum inhibitory concentration test.
2. For clarithromycin is recommended the use of 2 ug disk. Bacteria are considered resistant if there is no inhibition halo. A clarithromycin disk with 15ug concentration can also be used, in which case bacteria are considered resistant if the halo is less than 18mm in diameter (26).
In 2012 Ramos confirmed that culturing is the most specific test. The best samples for culturing are gastric biopsies which should be placed in a Stuart medium and cultivated for a short time. Charcoal should be added to the culture media at a concentration of 10% because it protects the microorganisms from free radicals of oxygen and fatty acids (31).
CONCLUSIONS
Preliminary identification of H. pylori from gastric biopsies is based on the characteristics of colonies and detection of enzymes such as catalase, cytochrome-oxidase and urease. Urease is a basic element for bacterial survival in the acid gastric environment.
When we analyzed media reported in the literature, we observe diverse possibilities according to the accessibility of different commercial products and different ingredients stored in microbiology laboratories. The basic components for preparation of these media are broth or nutrient agar supplemented with 8% fresh lamb or horse blood, 2% Isovitalex, 10% charcoal, 10% equine serum and antimicrobials such as vancomycin, trimethoprim, cefsulodin and amphotericin. Anaerobiotic conditions are obligatory because H. pylori are fastidious microorganisms. Colonies appear within 2 to 7 days under conditions of 5% to 10% 02, 5% to 10 % C02, 80% to 90% N2, 95% humidity and 35o C to 37o C temperature.
Acknowledgments
The author sincerely wishes to thank Andrés Julián Gutiérrez Escobar, GIBCA team leader.
REFERENCES
1. Sierra F. Helicobacter pylori. Estado actual. Revista colombiana de cirugía 2002; 17(3): 128-130. Disponible en http://www.encolombia.com/medicina/cirugia/ciru17302editorial.htm [ Links ]
2. Gutiérrez O. Seroprevalencia y factores de riesgo asociados con la infección por Helicobacter pylori en niños. revista de gastroenterología 2001; 16(1): 19-22 Disponible en http://www.encolombia.com/medicina/gastroenterologia/gastro16101trab-seroprevalencia.htm [ Links ]
3. Naranjo D, Suárez M, Bayona M, Gallego M, Urbina M, Rojas D. Aspectos históricos, epidemiológicos y patológicos de las helicobacteriosis en humanos y en caninos. Medicina (Bogotá) 2012; 34: 146-161. [ Links ]
4. World Gastroenterology Organisation Global Guideline. Helicobacter pylori in Developing Countries. Journal of Digestive Diseases 2011; 12; 319-326. [ Links ]
5. Bravo Luis E, Cortés Armando. Helicobacter pylori: patología y prevalencia en biopsias gástricas en Colombia. Revista Colombia Médica 2003; 34(3). Disponible en http://www.bioline.org.br/request?Rc03019. [ Links ]
6. Cittelly Diana Marcela, Henao Sandra Consuelo, Orozco Oscar, Martínez Julian David, Detección de Helicobacter pylori en Colombia: diferentes metodologías aplicadas a su estudio en una población de alto riesgo de cáncer gástrico. Revista colombiana de gastroenterología 1999; 14(3): 164-169. Disponible en http://www.encolombia.com/gastro14399-deteccion.htm [ Links ]
7. Blanchard T, Nedrud J. Laboratory maintenance of Helicobacter species. Current Protocols in Microbiology 2012; supplement 24. [ Links ]
8. Dixon M, Genta R, Yardley J, et al. Classification and grading of gastritis. The updated Sydney system. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol 1996; 20: 1161-81. [ Links ]
9. El-Zimaity H, Graham D. Evaluation of gastric mucosal biopsy site and number for identification of Helicobacter pylori or intestinal metaplasia: role of the Sydney system. Hum Pathol 1999; 30: 72-7. [ Links ]
10. Ndip R, Mackay W, Farthing M, Weaver L. Culturing Helicobacter pylori from clinical specimens: review of microbiologic methods. J Pediatr Gastroenterol Nutr 2003; 36: 616-622. [ Links ]
11. Hernández F, Rivera P. Historia natural de la infección por Helicobacter pylori, su tratamiento antimicrobiano y el empleo de plantas medicinales. Rev Costarric Cienc méd 2003; 24(3-4): 149-165. [ Links ]
12. Alarcón T, Baquero M, Domingo D, López-Brea M, Royo G. Procedimientos en microbiología microbiológico de la infección por Helicobacter pylori. Primera edición, Sociedad Española de Enfermedades infecciosas y Microbiología Clínica, Madrid, España; 2004. [ Links ]
13. Eeskandarian R, Ghorbani R, Shiyasi M, Momeni B, Hajifathalian K, Madani M. Prognostic role of H. pylori infection in acute coronary syndrome a prospective cohort study. Cardiovasc J Afr 2012; 23(3): 131-135. [ Links ]
14. Tersterman T, McGee D, Mobley H. Helicobacter pylori growth and urease detection in the chemically defined medium Hams F- 12 nutrient mixture. J Clin Microbiol 2001; 39(11): 3842-3850. [ Links ]
15. Joo J, Park K, Song J, Kim D, Lee K, Kwon Y, Kim J, Kim K, Youn H, Kang H, Baik S, Lee W, Cho M, Rhee K. Thin-layer liquid culture technique for the growth of Helicobacter pylori. Helicobacter 2010; 15(4): 295-302. [ Links ]
16. Stevenson T, Lucia L, Acuff G. Development of a selective medium for isolation of Helicobacter pylori from cattle and beef samples. Appl Environ Microbiol 2003; 66: 723-727. [ Links ]
17. Bilbao P, Claros M, Damiani E, Ascarrunz C, Cárdenas A, Lobo M, Altman E, Gabastou J, Verez B, Trigoso C. Infección por Helicobacter pylori: asociación a patologías gástricas y métodos de diagnóstico. Biofarbo 2007; 15(1): 51-54. [ Links ]
18. Yepes C, Rodríguez B, Ruiz A, Ariza B. Resistencia antibiótica del Helicobacter pylori en el hospital Universitario San Ignacio de Bogotá. Acta Med Colomb 2008; 33(1): 11-14. [ Links ]
19. Vega A, Silva H, Cortiñas T. Evaluation of a Serum-free transport medium supplemented with cyanobacterial extract, for the optimal survival of Helicobacter pylori from biopsy samples and strains. European Journal of clinical microbiology y infectious diseases 2012; 31(2): 135-139. [ Links ]
20. Trespalacios A, Otero W, Mercado M. Resistencia de Helicobacter pylori a metronidazol. Claritromicina y amoxicilina en pacientes colombianos. Rev Col Gastroenterol 2010; 25(1): 31-38. [ Links ]
21. Quiroga A, Citelly D, Bravo M. Frecuencia de los genotipos babA2, oipA y cagE de H. pylori en pacientes colombianos con enfermedades gastroduodenales. Biomédica 2005; 25: 325-334. [ Links ]
22. Jiménez L, Rohrer S, Jain U, Ertl C, Sewald X, Haas R. Effects of cholesterol on Helicobacter pylori growth and virulence properties in vitro. Helicobacter 2012; 17(2): 133-9. [ Links ]
23. Majalca C, Rivera J, Ochoa S, Giono S. Transporte, aislamiento, identificación y conservación de cepas de Helicobacter pylori. Bioquimia 2001; 26(4): 85-89. [ Links ]
24. Navarro J, Perea A, Pineda J, Díez O, Mercado M, Trespalacios A. Evaluación de la productividad de tres medios de cultivo para la recuperación de H. pylori. Universita Scientiarum, Revista de la Facultad de Ciencias 2007; 12: 79-86. [ Links ]
25. Tersterman T, Conn P, Mobley H, McGee D. Nutritional requirements and antibiotic resistance patterns of Helicobacter species in chemically defined media. J Clin Microbiol 2006; 44(5): 1650-8. [ Links ]
26. Mcnulty C, Owen R, Tompkins D, Hawtin P, McColl K, Price A, Smith G, Teare L. Helicobacter pylori susceptibility testing by disc diffusion. Journal Antimicrobial Chemotherapy 2002; 49(4): 601-609. [ Links ]
27. Miendje V, Van der Borre C, Fontaine V. Comparative evaluation of 3 selective media for primary isolation of Helicobacter pylori from gastric biopsies under routine condition. Diagnostic Microbiology & Infectious Disease 2010; 68: 474-476. [ Links ]
28. Grande R, Di Campli E, Di Bartolomeo S, Verginelli F, Di Giulio M, Baffoni M, Bessa L, Cellini L. Helicobacter pylori biofilm: a protective environment for bacterial recombination. J Appl Microbiol 2012; 113(3): 669-76. [ Links ]
29. Carron M, Tran V, Sugawa C, Coticchia J. Identification of Helicobacter pylori biofilms in human gastric mucosa. J Gastrointest Surg 2006; 10(5): 712-7. [ Links ]
30. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing and approved standard M7-A5. Informational supplement M100-S10.22. Clinical and Laboratory Standards Institute Wayne, Pa. 2000. [ Links ]
31. Ramos Javier. Infectología clínica. Segunda edición. Editorial El Manual Moderno S.A de C.V. 2012. [ Links ]











 texto em
texto em