Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.2 Bogotá Apr./June 2013
Description of cellular rejection in liver transplant patients at the Hospital Pablo Tobón Uribe 2005-2010
Germán Osorio MD (1), Esteban Quevedo (2), John-Alejandro Castañeda (2), Sandra Milena Isaza (2), Juan-Camilo Pérez MD (3), Juan-Ignacio Marín MD (3), Octavio Muñoz MD (3), Oscar Santos MD (3), Sergio Hoyos MD (1, 3), Carlos Guzmán MD (3), Álvaro Mena MD (3), Juan-Carlos Restrepo MD (1, 3)
(1) Professor in the Gastro-hepatology Group at the Universidad de Antioquia in Medellin, Colombia.
(2) Medical Student at the Universidad Pontificia Bolivariana in Medellin, Colombia.
(3) Liver Transplant Group at the Hospital Pablo Tobon Uribe in Medellin, Colombia. Mail: jcrestrepo@hptu.org.co
Received: 05-10-12 Accepted: 16-04-13
Abstract
Introduction: Acute cellular rejection is a complication of orthotopic liver transplantation (OLT) which occurs in between 30% and 70% of transplant patients in the first year after the procedure.
Objective: The objective of this study was to describe the main variables associated with cellular rejection in liver transplant patients at the Hospital Pablo Tobon Uribe in Medellin from 2005 to 2010.
Methods: Medical records of 248 patients who had undergone OLTs with cadaveric donor grafts were evaluated retrospectively. Patients with histological, clinical and biochemical evidence of cellular rejection were identified in accordance with universally accepted criteria.
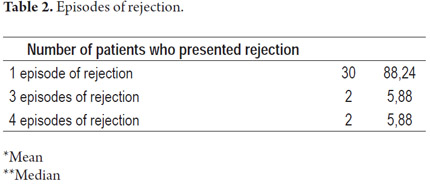
Results: 44 episodes of cellular rejection in 34 patients were confirmed from among 248 liver transplantations performed in from 2005 to 2010. The incidence of rejection was 13.7%. Thirty patients (88.2%) had one episode of rejection, two (5.8%) had three episodes and two others (5.8%) had four episodes.
Conclusions: We describe the main features of acute cellular rejection in this series and compare them with reports in the international literature. No other reports from Colombia were found. Most cases were mild to moderate acute cellular rejection which responded well to medical management without implications for graft or patient survival.
Keywords
Cellular rejection, orthotopic liver transplantation.
INTRODUCTION
Liver transplantation is recognized as the optimal therapy for terminal acute and chronic hepatic illnesses. An estimated 5,000 liver transplants (orthotopic hepatic transplantation) are performed annually in the United States and Western Europe (1).
During 2011, 1,085 organ transplants were performed in Colombia. Of these, 185 were liver transplants making the liver the second most frequently transplanted organ after the kidney (2). Nowadays, hepatic transplant results are excellent due to improvements in surgical techniques, care during and after surgery, immunosuppression schemes, prophylaxis and management of infections. One year survival rates are above 80% and five year survival rates are above 70 percent (3).
Complications occur despite these good results. The most important are vascular and biliary complications, infections, graft rejection and recurrence of illness. There are also complications associated with the treatments used in transplanted patients especially the use of immunosuppresors and broad spectrum antibiotics. The secondary and toxic effects of immunosuppresors include arterial hypertension, renal dysfunction, diabetes, ocular alterations, osteopathy, dyslipidemia, de novo neoplasia (First-line agents, including cyclosporine, increase the development of lymphoproliferative syndromes and lymphoma). All this must be taken into account when deciding upon immunosuppression for a transplant recipient (4). Each of these complications may interfere to one or another degree with the survival of the graft and/or the patient (3).
Cellular rejection of the hepatic graft occurs because of the intervention of the immune system which reacts to the genetic disparity between the donor and the recipient and generates a series of physiopathological conditions that cause an immune response which may advance to graft failure (5). Acute cellular rejection is the most common. It is indicated by clinical findings and biochemical changes but requires histological confirmation most of the time.
In the long run individual episodes of acute rejection have no influence upon survival of the hepatic graft or survival of the patient, but recurring events may result in permanent organ damage (5). In some cases hepatic re-transplant becomes the only option to save the patient.
This study attempts to describe post-transplant cellular rejection during the first 5 years of the hepatic transplant group in a hospital in the city of Medellín. It compares those results to results reported in the world literature.
MATERIALS AND METHODS
In the hepatic transplant program at Hospital Pablo Tobón Uribe and the Universidad de Antioquia, 269 liver transplants were performed on adults between February of 2004 and November of 2010. Of these, 15 were retransplants, all with cadaveric donors. The total number of patients at the Hospital Pablo Tobón Uribe in the city of Medellín who had hepatic orthotopic transplants from 2005 to 2010 was 248. This is a retrospective, descriptive, observational study. The sources of information are the hospital's database and the clinical histories of the patients.
Inclusion criteria
Patients transplanted in the Hospital Pablo Tobón Uribe in the city of Medellín between 2005-2010 who showed histological, clinical or biochemical evidence of cellular rejection following surgery were included. The histology report by a pathologist had to show portal or periportal hepatitis, venulitis and/or nonsuppurative cholangitis. The severity of rejection was classified according to BANF criteria as mild, moderate and severe in accordance with inflammatory compromise. Biochemical evidence included increased levels of alkaline phosphatase, Gamma-glutamyltransferase (GGT), bilirubin, and aminotransferase. Clinical manifestations included jaundice, abdominal pain, hepatosplenomegaly and fever although these are not specific to rejection. Patients were excluded if they failed to meet these criteria.
All clinical histories and the database of the hepatic transplant group of Hospital Pablo Tobón Uribe and Universidad de Antioquia were reviewed retrospectively. Factors reviewed included social-demographic variables, tests of hepatic function and cross matched scores. In addition time of occurrence of cellular rejection, biochemical resolution time determined by normalization of hepatic function tests, and mortality rates associated with cellular rejection were also determined for our report.
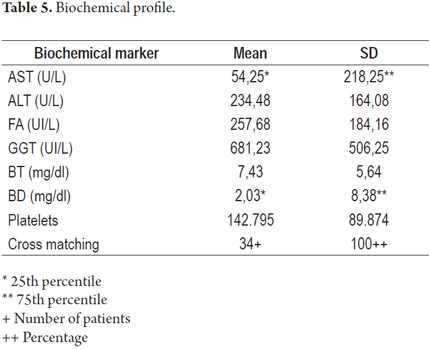
Results were expressed descriptively according to existing variables in the study population. The distribution of the variables was determined by the Kolmogorov-Smirnov test. Normal distributions are presented with mean and standard deviation, but abnormal distributions are presented in terms of 25th, 50th and 75th percentiles.
RESULTS
Between January 2005 and December 2010 (60 months), 248 liver transplants with cadaveric donors were performed in adults. The retrospective analysis found 44 episodes of cellular rejection in 34 patients for an incidence of 13.7%.
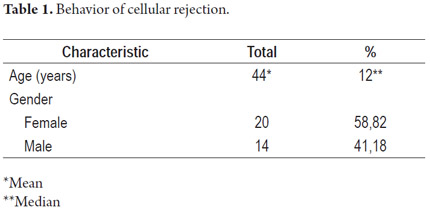
Out of the 34 patients who showed cellular rejection, 30 (88.2%) presented a single episode, while two (5.8%) presented three episodes, and two others (5.8%) presented four episodes for a total of 44 episodes among 34 affected patients (Tables 1 and 2).
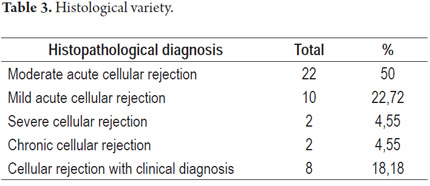
There were 22 cases (50%) of moderate acute cellular rejection, 10 cases (22.72%) of mild acute cellular rejection, 2 cases (4.55%) of severe acute cellular rejection, and two cases of (4.55%) chronic cellular rejection. Eight cases (18.18%) were not possible to classify according to histological type of the rejection by means of biopsy because of counter-indications in these patients. They were classified as cases of rejection because of clinical and biochemical findings (Table 3).
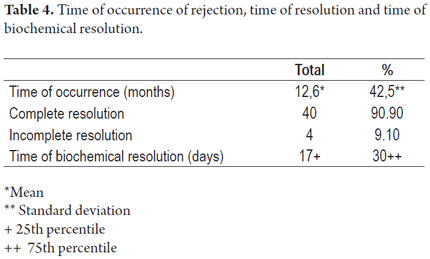
The average number of days following transplantation at which the rejection occurred was 378.18 (12.6 months) with a median of 42.5 days (1.4 months). 40 of the cases (90.9%) resolved completely, while 4 (9.1%) did not achieve resolution. One of these required a retransplant. The mortality rate associated with rejection in our study was 5.88% or 2 deaths out of 34 patients. These were both patients who did not achieve resolution. The average number of days required for biochemical resolution of cellular rejection was 30 (Table 4).
The average value of aspartate aminotransferase (AST) measured at the time of cellular rejection was 54.25 U/L while the average value of aspartate alanine transaminase (ALT) was 234 U/L (±164). The alkaline phosphatase (ALP) average was 257 U/L (±184) and the gamma-glutamyl transpeptidase average was 681 U/L (±506). Total bilirubin was 7.34 mg/dl (±5.64) and direct bilirubin was 2.03 mg/dl (The 75th percentile is 8.38.) The average platelet count was 142,795 (±89,874). Cross matching was negative in all patients with cellular rejection (Table 5).
DISCUSSION
Liver transplantation has become the choice treatment for patients with terminal hepatic illness (6). Since the first liver transplant was performed in 1963 by Thomas Starzi (7), knowledge about this procedure and its complications has increased. Cellular reaction continues to an important consideration associated with transplantation since between 30% and 70% of transplanted patients present cellular rejection within a year of the procedure. The highest incidence occurs in the first 7 to 10 days, but a great number of episodes also occur during the first and second year after transplantation (8).
Based upon the reversibility and histologic characteristics of the inflammatory infiltrate, rejection is divided into hyper-acute (mediated by antibodies), acute (cellular) and chronic (ductopenic). Hyper-acute rejection appears a few hours after transplantation and originates as a consequence of the humoral reaction of preformed antibodies (5, 9). Acute rejection generally occurs weeks or even months after transplantation and is mediated by T cells. It is a response to recognition of allogenic determinants of the transplanted liver such as those of the major histocompatibility complex (10). Chronic rejection occurs months after transplantation. Its primary histologic characteristic is the progressive destruction of biliary ducts (6).
Risk factors identified for cellular rejection include youthful age, black race (11), transplants required as the result of auto-immune illnesses (12). transplants required as the result of hepatic failure, cold ischemia time longer than 15 hours, donors older than 30 years (7). and recipients infected with hepatitis C virus (13). Studies have shown that original illnesses also influence the incidence of rejection. The rate of rejection is lower among patients with alcoholic hepatic illness than in patients with primary biliary cirrhosis (14). Patients from rural areas have higher incidences of rejection than other patients (15). Other risk factors that have been associated with cellular rejection after transplantation include transplanted tissue containing biochemical markers such as the modulator of mitochondrial RNA CXCL9 (16).
The 13.7% incidence of cellular rejection found in this study is lower than those reported in other studies (17). The low mortality rate of 5.88% associated with cellular rejection means that these patients have good prognoses in our institution.
The primary indication for transplantation among the patients who presented cellular rejection was cryptogenic cirrhosis. This was reported in 9 (26.47%) of the 34 patients while alcoholic cirrhosis was found in 9 patients and primary biliary cirrhosis was found in 6 patients (17.65%). These data contrast with Neuberger's report15 because our study included a higher proportion of rejection among patients with alcoholic illness than in patients with primary biliary cirrhosis. In addition we observed a slight trend towards more frequent rejections among women (58%) than men. The study proportion was one woman for every 1.31 men. Base pathologies of auto-immune illnesses and cryptogenic cirrhosis were more common among women.
The mean age at rejection time was 44 years which is compatible with the risk factors previously mentioned since there is a higher rate of rejection among young adults. The low death rate among patients transplanted in the unit shows a higher percentage of success than in other studies (18), but an analytical study would be required to explain this finding. It is unlikely for acute rejections to require retransplantation while 28% to 35% of the patients who present chronic cellular rejection do not respond to treatment with high dosage of steroids and do require retransplantation. In this center, only one patient required retransplantation because of failure of rejection to resolve resulting in a lower incidence than that globally reported (19). Nevertheless, this may be due to the higher proportion of acute rejections than chronic rejections given that the latter is more closely associated with the need for retransplantation.
In conclusion, this series describes the primary characteristics of acute cellular rejection and compares them to the international literature. No other Colombian reports were found. Most cases were mild or moderate acute cellular rejections which responded well to medical management without repercussions to the survival of the graft or the patient.
REFERENCES
1. Lucey MR. Liver Transplantation: An Overview. Liver Transplantation. Michael R. Lucey, James Neuberger and Abraham Shaked. Landes Bioscience 2003. p. 1-4. [ Links ]
2. Instituto nacional de salud. Informe anual de red de donación y trasplantes. 2011. [ Links ]
3. Thuluvath P, Guidinger M, Fung J, Johnson L, Rayhill S, Pelletier S. Liver transplantation in the United States, 1999-2008. Am J Transplant 2010; 10(4 Pt 2): 1003-19. [ Links ]
4. Van Thiel D, Makowka L, Starzl T. Liver transplantation: where it's been and where it's going. Gastroenterol Clin North Am 1988; 17(1): 1-18. [ Links ]
5. Bermejo J, Ontañon J. Rechazo en trasplante hepático: histopatología e inmunología. En Álvarez R. Inmunología del trasplante hepático. 1997. p. 262-270. [ Links ]
6. Wiesner R, Ludwig J, van Hoek B, Krom R. Current concepts in cell-mediated hepatic allograft rejection leading to ductopenia and liver failure. Hepatology 1991; 14(4 Pt 1): 721-9. [ Links ]
7. Starzl T, Marchioro T, Vonkaulla K, Hermann G, Brittain R, Waddell W. Homotransplantation of the liver in humans. Surg Gynecol Obstet 1963; 117: 659-76. [ Links ]
8. Fisher L, Henley K, Lucey M. Acute cellular rejection after liver transplantation: variability, morbidity, and mortality. Liver Transpl Surg 1995; 1(1): 10-5. [ Links ]
9. Bird G, Friend P, Donaldson P, O'Grady J, Portmann B, Calne R, et al. Hyperacute rejection in liver transplantation: a case report. Transplant Proc 1989; 21(4): 3742-4. [ Links ]
10. Lai Q, Pinheiro R, Levi Sandri G, Spoletini G, Melandro F, Guglielmo N, et al. Laparoscopy in Liver Transplantation: The Future has Arrived. HPB Surg 2012; 2012: 148387. [ Links ]
11. Maggard M, Goss J, Ramdev S, Swenson K, Busuttil R. Incidence of acute rejection in African-American liver transplant recipients. Transplant Proc 1998; 30(4): 1492-4. [ Links ]
12. Neuberger J, Adams D. What is the significance of acute liver allograft rejection? J Hepatol 1998; 29(1): 143-50. [ Links ]
13. Neuberger J. Incidence, timing, and risk factors for acute and chronic rejection. Liver Transpl Surg 1999; 5(4 Suppl. 1): S30-6. [ Links ]
14. Farges O, Saliba F, Farhamant H, Samuel D, Bismuth A, Reynes M, Bismuth H. Incidence of rejection and infection after liver transplantation as a function of the primary disease: possible influence of alcohol and polyclonal immunoglobulins. Hepatology 1996; 23(2): 240-8. [ Links ]
15. Park K, Bensen R, Lu B, Nanda P, Esquivel C, Cox K. Geographical rural status and health outcomes in pediatric liver transplantation: an analysis of 6 years of national United Network of Organ Sharing Data. J Pediatr 2013; 162(2): 313-8. [ Links ]
16. Asaoka T, Marubashi S, Kobayashi S, Hama N, Eguchi H, Takeda Y, Tanemura M,Wada H, Takemasa I, Takahashi H, Ruiz P, Doki Y, Mori M, Nagano H. Intragraft transcriptome level of CXCL9 as biomarker of acute cellular rejection after liver transplantation. J Surg Res 2012; 178(2): 1003-14. [ Links ]
17. Varela G, Hernández J, Nieto J, Alcántar J, Fuentes V, Castañeda P, et al. Pediatric liver transplant program at Hospital Infantil de México Federico Gómez. Rev Invest Clin 2011; 63(Suppl. 1): 57-61. [ Links ]
18. Li C, Wen T, Yan L, Li B, Yang J, Wang W, et al. Predictors of patient survival following living donor liver transplantation. Hepatobiliary Pancreat Dis Int 2011; 10(3): 248-53. [ Links ]
19. Feltracco P, Barbieri S, Galligioni H, Michieletto E, Carollo C, Ori C. Intensive care management of liver transplanted patients. World J Hepatol 2011; 3(3): 61-71. [ Links ]











 text in
text in