Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.2 Bogotá Apr./June 2013
Complete cure of Barrett's Esophagus with low and high grade dysplasia through a combination of Focal Duette® Endoscopic Mucosal Resection and Radiofrequency Ablation: Case report and literature review
Mario Rey Ferro, MD (1), Raúl Eduardo Pinilla M, MD. (2)
(1) Specialist in Gastrointestinal Surgery and Endoscopy at the National Cancer Institute, Clínica de Marly, and the Clínica de la Mujer Bogota in Bogota, Colombia. Mail: reyferro1@gmail.com.
(2) General Practitioner from Universidad El Bosque, General Surgeon from Hospital Universitario de la Samaritana y Pontificia Universidad Javeriana, Endoscopist and Gastroenterologist from Hospital San José and the Fundación Universitaria de Ciencias de la Salud in Bogotá, Colombia. Minimally Invasive Gastrointestinal Surgery from Jose Joaquin Aguirre Hospital at the Universidad de Chile. Institut Clinic de Malaties Digestives i Metaboliques del Hospital Clinic i Provincial de Barcelona, Catalonia, Spain. Mail: radipisa@hotmail.com.
Received: 03-08-12 Accepted: 16-04-13
Abstract
The management of Barrett's esophagus (BE) and dysplastic and neoplastic changes associated with it has changed with the recent advent of techniques such as endoscopic mucosal resection and radiofrequency ablation. These two techniques have been added to the repertoire for managing this complication of gastroesophageal reflux disease because of their high levels of safety combined with the rarity of complications resulting from them. We report a case of Barrett's esophagus and associated dysplasia which was managed first with a sequence of mucosal resection of large lesions followed by radiofrequency ablation. Complete eradication of dysplasia and intestinal metaplasia was achieved.
Keywords
Barrett's esophagus, radiofrequency ablation, endoscopic mucosal resection, treatment.
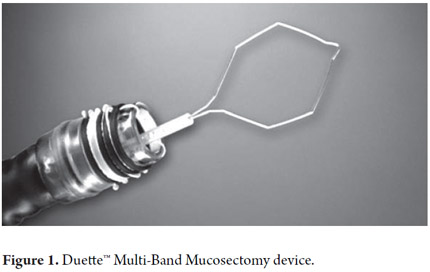
INTRODUCTIONSince its initial description more than 60 years ago by the Australian surgeon Norman Rupert Barrett, Barrett's esophagus has become one of the most fearful consequences of gastroesophageal reflux. This replacement of the columnar epithelium in the esophagus is confirmed when a biopsy finds the presence of intestinal metaplasia which has the risk of developing into adenocarcinoma. This condition remains a challenge for physicians and surgeons (1). Increased incidence esophageal adenocarcinoma of up to 400% has been reported. This finding has prompted development of multiple strategies to reduce the progression of this disease (2, 3). The risk of developing adenocarcinoma from Barrett's epithelium is 0.5% per year, (4) but this to 1.6% per year for low grade dysplasia (5) up to 6% per year for high grade dysplasia (6). There is no doubt that this condition needs specific follow-up which is offered to patients according to initial endoscopic findings in order to monitor and characterize the appearance dysplasia and to determine the type of treatment (7). Traditionally, surgery has been considered the treatment of choice for high grade dysplasia, but the not insignificant morbidity and mortality rates have motivated investigation into new nonsurgical treatments that might be able to decrease the number of complications without endangering long time results for patients. The Duette Multiband Mucosectomy Kit (Cook Ireland Ltd, Limerick, Ireland) is easily applicable to esophageal dysplasia (Figure 1) and has minimal complications which have made this procedure increasingly popular (8). Radiofrequency ablation (RFA) is a technique which ablates the lesion by heating the tissues. It has the advantage of penetrating only through the mucosa because it is automatically controlled by an impedance based feedback loop (9).
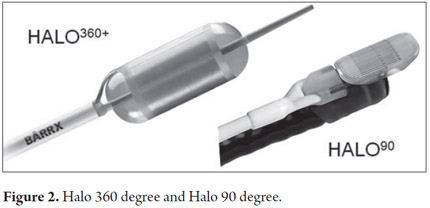
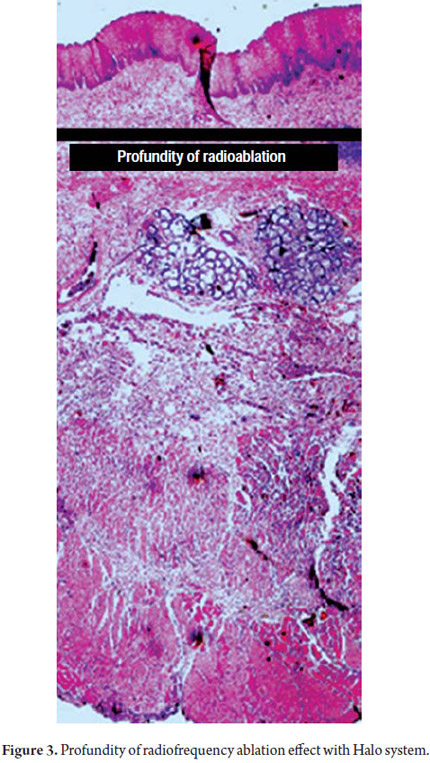
The HALO system (BÂRRX Medical, Inc., Sunnyvale, CA) is composed of 2 different ablation systems. The HALO 360 performs circumferential radiofrequency ablation and the HALO 90 performs focal ablation which can be used for primary treatment of short segments of EB or for secondary of focal residual lesions. The HALO 360 ablation catheter has a generator and a 3 cm bipolar electrode located in the external surface of a balloon which has 5 possible diameters (22 mm, 25 mm, 28 mm, 31 mm and 34 mm). The ablation catheter is inflated with a pedal while the radiofrequency is released by the electrode. For circumferential ablation, two applications of radiofrequency of 10-12 J/cm2 and 40W/cm2 are adequate for ablation of the thickness of the mucosa. The HALO 90 consists of an electrode with a 20 x 13mm surface attached over the end of the endoscope. The recommended potencies with this catheter are 2 applications of 12-15 J/cm2 and 40W/cm2. For the 2 types of catheters, the generator releases the radiofrequency at a predetermined density which reaches a uniform penetration in the tissue of 1000 microns that does not depend on the operator. With this method it is possible to destroy all epithelial layers, the lamina propia and part of the muscularis mucosae without damaging the submucosa (Figure 2) (9, 10).
We present the first case in our country of complete eradication of Barrett's esophagus and high and low dysplasia with the treatments described above.
CASE REPORT
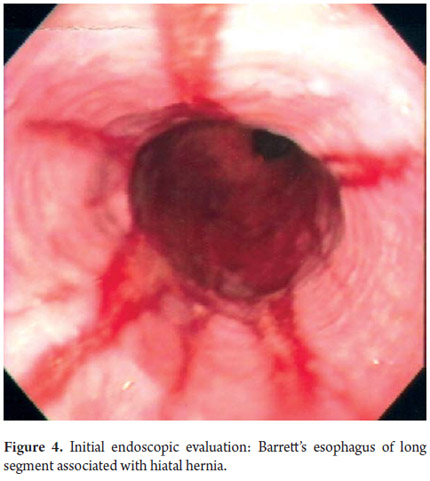
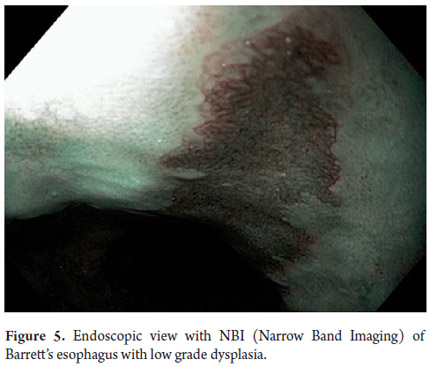
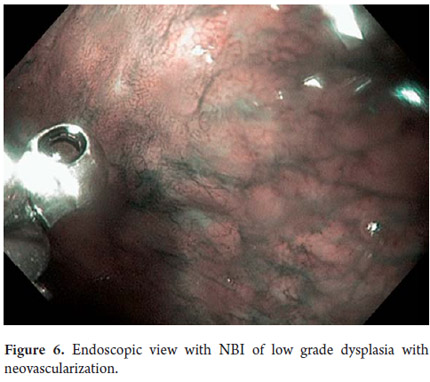
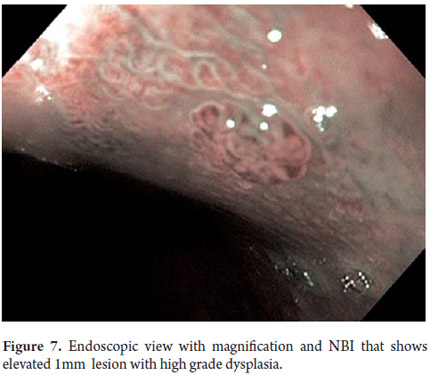
The patient is a 58 year old man who had been an occasional smoker until 19 years ago. Patient is a social drinker who was diagnosed with grade B esophagitis and 7 cm (30 to 37 cm) Barrett's esophagus in 2000. He had a 3 cm hiatal hernia associated with symptoms of pyrosis and intermittent hoarseness and coughing (Figure 3). Patient was treated with continuous administration of proton pump inhibitors to control symptoms and esophagitis. An endoscopic examination in 2002 identified Barrett's esophagus without elevated or sunken lesions. Biopsies showed low grade dysplasia which persisted until March 2007. An examination in August 2007 showed grade CA dysplasia in situ. Patient was referred to one of the authors (M.R.F) who checked the histological slides with 3 pathologists to confirm the diagnosis of high grade dysplasia. In November 2007 endoscopy with magnification and NBI (Narrow Band Imaging) was performed with patient under deep sedation to take direct biopsies. Each centimeter of the metaplastic epithelium was evaluated in a helical form. Three areas of dysplasia were identified. One was a small modulated area of 1mm. Images were taken pictures of each suspicious area and of the biopsy sites. Biopsies were placed in separate flasks which were marked for identification with locations in centimeters and the time that the samples were taken.
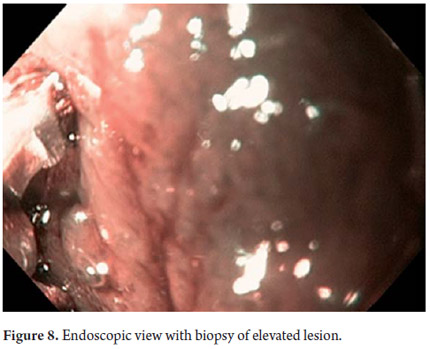
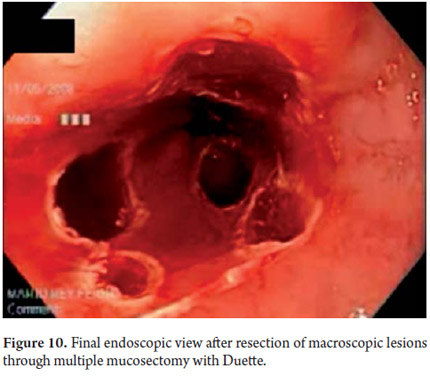
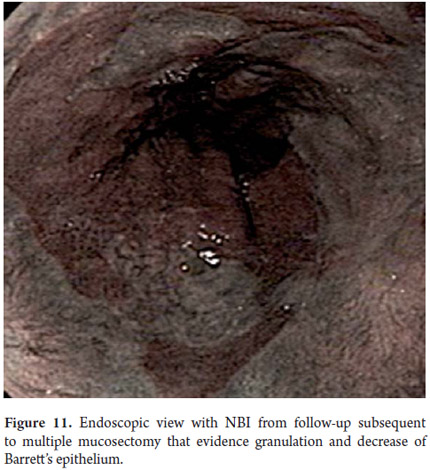
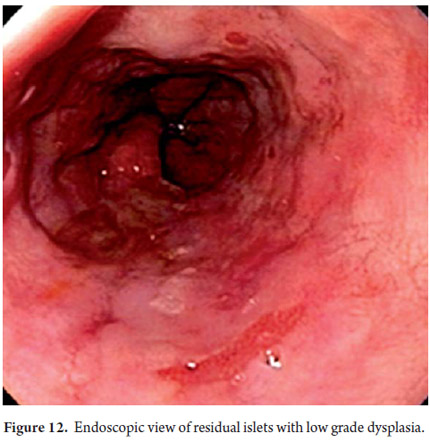
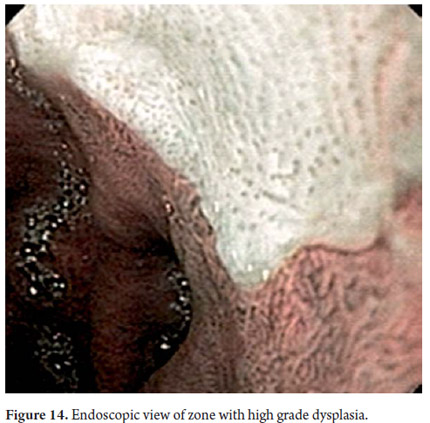
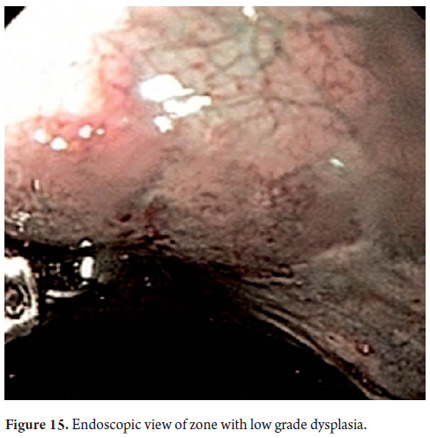
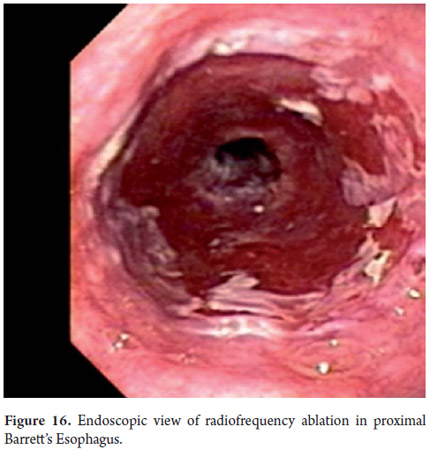
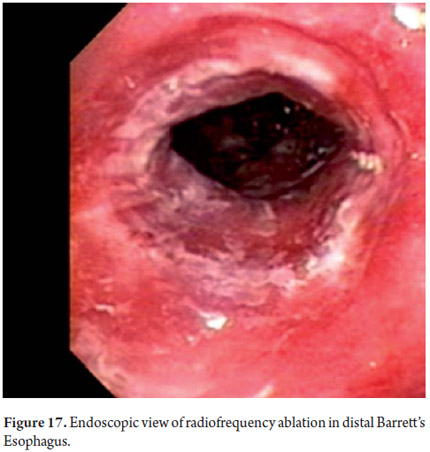
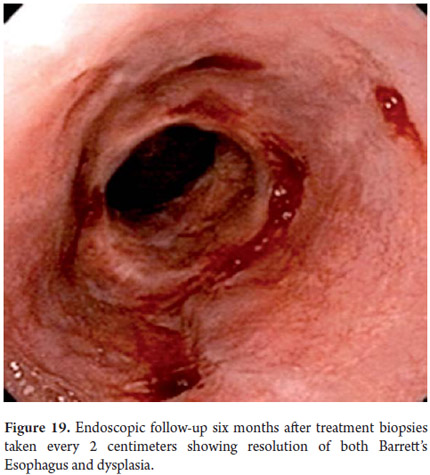
Three areas with low grade dysplasia were confirmed as lesions with neovascularization and mucosal dysplasia identified through endoscopic NBI. One area of high grade dysplasia was found in an elevated lesion of 1 mm (Figures 4, 5, 6 and 7). In February 2008 multiple mucosectomy with suction and elastic band ligature was performed together with resectioning using the Duette system to completely remove the lesions in six 1.2 cm diameter segments. Pathology results for all biopsies had negative margins (Figure 8, 9). One month later endoscopic examination showed adequate healing (Figure 10). Later examinations identified three islets of Barrett's esophagus which progressed to low grade dysplasia over the next three years. In September 2011 a point focus of high grade dysplasia without elevated lesions was identified (Figures 11, 12, 13 and14). On November 10, 2011 radiofrequency ablation using the HALO 360 degree system was performed with the patient under deep sedation. A 6 cm (33 to 40 cm) area of Barrett's esophagus had been found in an esophagus that was 3.1 cm in diameter. A 28mm balloon was used for ablation since the 30 cm balloon would have extended to the gastric creases of the hernia. The fibrin was removed with a cup and then the device was used without complications (Figures 15 and 16). Patient was put on a liquid diet followed by a soft and analgesic treatment for 3 days. Since the procedure the patient has had follow-up examinations every 3 months at which the protocol calls for biopsies every 2 cm. 16 biopsies taken from the first follow-up and 12 biopsies taken from the second follow-up showed only mild esophagitis or normal mucosa thus confirming complete eradication of Barrett's esophagus and both low and high grade dysplasia (Figures 17, 18 and19).
DISCUSSION
Barrett's esophagus is considered to be a pre-malignant lesion. Patients have risks of 10 to 150 times that of the general population of developing esophageal cancer. Level of risk depends on whether or not dysplasia is present, and on the grade dysplasia (11-13). Current recommendations for patients with Barrett's esophagus include esophagogastroduodenoscopy plus biopsies from 4 quadrants every 2 cm of the columnar epithelium every 3 to 5 years when dysplasia is absent. Biopsies should be taken every 6 to 12 months in cases with low grade dysplasia and every 3 months in cases of high grade dysplasia that have not been eradicated (7). Indisputably the treatment outlined above has important costs. This is also true for studies of biomarkers to improve diagnosis of low grade dysplasia and determine disease progression through estimation of aneuploidy although this method has not yet been approved for routine use (14).
Although esophagectomies are commonly accepted for management of patients with both high grade dysplasia and Barrett's esophagus, they have a 50% morbidity rate and 5% surgical mortality rate even at medical centers with great amounts of experience in this type of procedures (15,16). The most recent reports show that only 12% of these surgical specimens have invasive adenocarcinoma while it has also been demonstrated that surgical treatment and endoscopic treatment of this type of patients have the same survival rates (17,18). Since m1 and m2 intramucosal lesions in these patients have no possibility of lymph node involvement, since m3 lesions involve the lymph nodes in only 4% of cases, less invasive endoscopic resection could be a valid alternative for treatment of this condition (19).
Focal endoscopic resection of the mucosa has obtained complete remission in 97% to 100% of patients with high grade dysplasia and carcinoma in situ with 5 year survival rates of 84% to 98% (20-22). Recurrences or meta-chronic lesions reported in 21.5% of these patients can also be managed this way (23). Management of metaplastic esophageal mucosa through circumference resection has achieved complete eradication in up to 97.5% of cases (24, 25). Even though endoscopic resection of the submucosa has shown better data than conventional mucosal resection techniques with respect to margins free of metaplastic tissue, endoscopic resection is a technically demanding technique which presents frequent major complications when used for the eradication of Barrett's esophagus. The principal disadvantages of circumferential resections or those covering more than 75% of the diameter are high frequency of stenosis which require dilatation, bleeding, and in the case of submucosal endoscopic resections a higher incidence of perforations with low applicability in the west (26-28).
Ablation has a demonstrated impact on the development of adenocarcinoma avoiding 1 case out of every 20 patients with high grade dysplasia (29). The use of the Nd-YAG (neodymium-doped yttrium aluminum garnet) lasers, photodynamic therapy and cryotherapy have demonstrated their capacity to eliminate dysplastic mucosa as well as remaining metaplastic mucosa in BE, but they have two undesirable effects. The first is the impossibility of collection of tissue which has the consequence of preventing oncological confirmation. The second is the high incidence of stenoses subsequent to treatment (30, 31). In addition there can be complications such as photosensitization and development of metaplasia with dysplasia under the regenerated epithelium (32).
La ARF ha demostrado ser un método efectivo erradicando la mucosa pre-maligna con una duración sostenida en el tiempo (2 a 5 años) y escasa presentación de metaplasia bajo el epitelio regenerado, así mismo ha mostrado tener una baja frecuencia de complicaciones como estenosis o sangrado e incluso ya se cuenta con estudios que sugieren dicho procedimiento como costo-efectivo al compararlo con el seguimiento endoscópico en pacientes seleccionados (33-39).
Radiofrequency ablation has demonstrated itself to be an effective method for eradicating the pre-malign mucosa for sustained periods of two to five years with limited occurrences of metaplasia under the regenerated epithelium. Similarly, it has shown a low frequency of complications such as stenosis or bleeding. There are even studies that suggest that this procedure is more cost-effective than endoscopic follow-up for selected patients (33-39).
This has motivated the development of a technique combining resection of focal mucosa with the Duette type device followed by radiofrequency ablation of BE (40). This offers benefits similar to surgical management for eradication of metaplastic tissue, eliminating the possibility of metachronic lesions and avoiding wide resection of the mucosa. It has good results in terms of long term disappearance of the metaplastic mucosa (23, 26, 35, 36, 41-44).
The case reported herein is the first in our country with endoscopic and pathological demonstration of 7 cm BE with both high and low grade dysplasia. Both types of dysplasia were completely eradicated as confirmed by normal esophageal mucosa found in follow-up examinations which once again confirms the favorability of this combined approach.
R.E. Pouw's retrospective study of 169 patients with average 32 months follow up showed the superiority of combined management for resection of visible lesions associated with RFA for complete eradication of Barrett's mucosa. The study showed absence of Barrett's mucosa in the short and medium term and a low recurrence rate of 6% in cases of BE without dysplasia. The study showed a complete response in 100% of cases of carcinoma in situ (35). In addition this technique resulted in a lower frequency of complications such as perforations and stenosis than did circumferential mucosal resections.
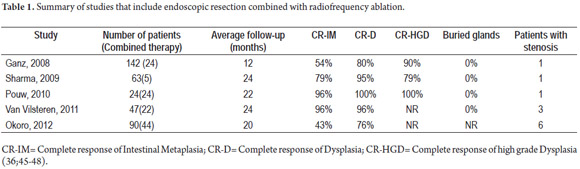
All of the above points toward taking combined therapy into consideration for multiple reasons. First, focal mucosal resection of visible lesions provides a surgical piece which is evaluable to the pathologist and which provides the security of correct oncological management. Second, it avoids complications derived from extensive circumferential mucosal resections and the complication of stenosis with respect to the submucosa. Third, the incidence of Barrett's mucosa under the regenerated epithelium is practically nonexistent, unlike for other ablative therapies. Fourth, it offers the possibility of eradicating all Barrett's epithelium thus limiting the appearance of synchronous or metachronous lesions and providing for integral management of the situation. Studies of RFA combined with mucosal resection prior to appearance of visible lesions have shown this technique to be safe and efficient. Follow-up periods up to 60 months have shown eradication rates of intestinal metaplasia of 54% to 100%, eradication of dysplasia from 79% to 100%, frequency of buried glands from 0% to 5.1% and frequency of stenosis from 0% to 14% subsequent to this type of treatment (Table 1).
Given that this combined therapy has been demonstrated to be safe and effective for the treatment of Barrett's esophagus associated with high grade dysplasia, we ask ourselves whether we should continue waiting in the face of this cancer precursor, or if to the contrary we should remember our experience with resection of colorectal polyps and use this type of management for select patients with Barrett's esophagus and low grade dysplasia. If we do we will avoid complications derived from circumferential mucosal resections including the risk of future development of synchronous and metachronous lesions in the premalignant epithelium in cases when eradication is incomplete and including performing radical surgery required when there is a diagnosis of reappearance of neoplasia.
REFERENCES
1. Barrett NR. Chronic peptic ulcer of the oesophagus and oesophagitis'. Br J Surg 1950; 38(150): 175-82. [ Links ]
2. Brown LM, Devesa SS. Epidemiologic trends in esophageal and gastric cancer in the United States. Surg Oncol Clin N Am 2002; 11(2): 235-56. [ Links ]
3. Sharma P. Clinical practice. Barrett's esophagus. N Engl J Med 2009; 361(26): 2548-56. [ Links ]
4. Sharma P, Falk GW, Weston AP, Reker D, Johnston M, Sampliner RE. Dysplasia and cancer in a large multicenter cohort of patients with Barrett's esophagus. Clin Gastroenterol Hepatol 2006; 4(5): 566-72. [ Links ]
5. Wani S, Mathur S, Sharma P. How to manage a Barrett's esophagus patient with low-grade dysplasia. Clin Gastroenterol Hepatol 2009; 7(1): 27-32. [ Links ]
6. Rastogi A, Puli S, El-Serag HB, Bansal A, Wani S, Sharma P. Incidence of esophageal adenocarcinoma in patients with Barrett's esophagus and high-grade dysplasia: a meta-analysis. Gastrointest Endosc 2008; 67(3): 394-8. [ Links ]
7. Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association medical position statement on the management of Barrett's esophagus. Gastroenterology 2011; 140(3): 1084-91. [ Links ]
8. Soehendra N, Seewald S, Groth S, Omar S, Seitz U, Zhong Y, et al. Use of modified multiband ligator facilitates circumferential EMR in Barrett's esophagus (with video). Gastrointest Endosc 2006; 63(6): 847-52. [ Links ]
9. Ganz RA, Utley DS, Stern RA, Jackson J, Batts KP, Termin P. Complete ablation of esophageal epithelium with a balloon-based bipolar electrode: a phased evaluation in the porcine and in the human esophagus. Gastrointest Endosc 2004; 60(6): 1002-10. [ Links ]
10. Smith CD, Bejarano PA, Melvin WS, Patti MG, Muthusamy R, Dunkin BJ. Endoscopic ablation of intestinal metaplasia containing high-grade dysplasia in esophagectomy patients using a balloon-based ablation system. Surg Endosc 2007; 21(4): 560-9. [ Links ]
11. Murray L, Watson P, Johnston B, Sloan J, Mainie IM, Gavin A. Risk of adenocarcinoma in Barrett's oesophagus: population based study. BMJ 2003; 327(7414): 534-5. [ Links ]
12. Jankowski JA, Perry I, Harrison RF. Gastro-oesophageal cancer: death at the junction. BMJ 2000; 321(7259): 463-4. [ Links ]
13. Hameeteman W, Tytgat GN, Houthoff HJ, van den Tweel JG. Barrett's esophagus: development of dysplasia and adenocarcinoma. Gastroenterology 1989; 96(5 Pt 1): 1249-56. [ Links ]
14. Moyes LH, Going JJ. Still waiting for predictive biomarkers in Barrett's oesophagus. J Clin Pathol 2011; 64(9): 742-50. [ Links ]
15. Heitmiller RF, Redmond M, Hamilton SR. Barrett's esophagus with high-grade dysplasia. An indication for prophylactic esophagectomy. Ann Surg 1996; 224(1): 66-71. [ Links ]
16. Hulscher JB, van Sandick JW, de Boer AG, Wijnhoven BP, Tijssen JG, Fockens P, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med 2002; 347(21): 1662-9. [ Links ]
17. Zehetner J, DeMeester SR, Hagen JA, Ayazi S, Augustin F, Lipham JC, et al. Endoscopic resection and ablation versus esophagectomy for high-grade dysplasia and intramucosal adenocarcinoma. J Thorac Cardiovasc Surg 2011; 141(1): 39-47. [ Links ]
18. Prasad GA, Wang KK, Buttar NS, Wongkeesong LM, Krishnadath KK, Nichols FC, III, et al. Long-term survival following endoscopic and surgical treatment of high-grade dysplasia in Barrett's esophagus. Gastroenterology 2007; 132(4): 1226-33. [ Links ]
19. Konda VJ, Ross AS, Ferguson MK, Hart JA, Lin S, Naylor K, et al. Is the risk of concomitant invasive esophageal cancer in high-grade dysplasia in Barrett's esophagus overestimated? Clin Gastroenterol Hepatol 2008; 6(2): 159-64. [ Links ]
20. Ell C, May A, Pech O, Gossner L, Guenter E, Behrens A, et al. Curative endoscopic resection of early esophageal adenocarcinomas (Barrett's cancer). Gastrointest Endosc 2007; 65(1): 3-10. [ Links ]
21. Pech O, Behrens A, May A, Nachbar L, Gossner L, Rabenstein T, et al. Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett's oesophagus. Gut 2008; 57(9): 1200-6. [ Links ]
22. May A, Gossner L, Pech O, Muller H, Vieth M, Stolte M, et al. Intraepithelial high-grade neoplasia and early adenocarcinoma in short-segment Barrett's esophagus (SSBE): curative treatment using local endoscopic treatment techniques. Endoscopy 2002; 34(8): 604-10. [ Links ]
23. Gondrie JJ, Pouw RE, Sondermeijer CM, Peters FP, Curvers WL, Rosmolen WD, et al. Stepwise circumferential and focal ablation of Barrett's esophagus with high-grade dysplasia: results of the first prospective series of 11 patients. Endoscopy 2008; 40(5): 359-69. [ Links ]
24. Pouw RE, Seewald S, Gondrie JJ, Deprez PH, Piessevaux H, Pohl H, et al. Stepwise radical endoscopic resection for eradication of Barrett's oesophagus with early neoplasia in a cohort of 169 patients. Gut 2010; 59(9): 1169-77. [ Links ]
25. Chennat J, Konda VJ, Ross AS, de Tejada AH, Noffsinger A, Hart J, et al. Complete Barrett's eradication endoscopic mucosal resection: an effective treatment modality for high-grade dysplasia and intramucosal carcinoma--an American single-center experience. Am J Gastroenterol 2009; 104(11): 2684-92. [ Links ]
26. Peters FP, Kara MA, Rosmolen WD, Ten Kate FJ, Krishnadath KK, van Lanschot JJ, et al. Stepwise radical endoscopic resection is effective for complete removal of Barrett's esophagus with early neoplasia: a prospective study. Am J Gastroenterol 2006; 101(7): 1449-57. [ Links ]
27. Seewald S, Akaraviputh T, Seitz U, Brand B, Groth S, Mendoza G, et al. Circumferential EMR and complete removal of Barrett's epithelium: a new approach to management of Barrett's esophagus containing high-grade intraepithelial neoplasia and intramucosal carcinoma. Gastrointest Endosc 2003; 57(7): 854-9. [ Links ]
28. Shaheen NJ, Overholt BF, Sampliner RE, Wolfsen HC, Wang KK, Fleischer DE, et al. Durability of radiofrequency ablation in Barrett's esophagus with dysplasia. Gastroenterology 2011; 141(2): 460-8. [ Links ]
29. Wani S, Puli SR, Shaheen NJ, Westhoff B, Slehria S, Bansal A, et al. Esophageal adenocarcinoma in Barrett's esophagus after endoscopic ablative therapy: a meta-analysis and systematic review. Am J Gastroenterol 2009; 104(2): 502-13. [ Links ]
30. Brandt LJ, Kauvar DR. Laser-induced transient regression of Barrett's epithelium. Gastrointest Endosc 1992; 38(5): 619-22. [ Links ]
31. Overholt BF, Panjehpour M, Haydek JM. Photodynamic therapy for Barrett's esophagus: follow-up in 100 patients. Gastrointest Endosc 1999; 49(1): 1-7. [ Links ]
32. Pouw RE, Wirths K, Eisendrath P, Sondermeijer CM, Ten Kate FJ, Fockens P, et al. Efficacy of radiofrequency ablation combined with endoscopic resection for barrett's esophagus with early neoplasia. Clin Gastroenterol Hepatol 2010; 8(1): 23-9. [ Links ]
33. Das A, Wells C, Kim HJ, Fleischer DE, Crowell MD, Sharma VK. An economic analysis of endoscopic ablative therapy for management of nondysplastic Barrett's esophagus. Endoscopy 2009; 41(5): 400-8. [ Links ]
34. Gray NA, Odze RD, Spechler SJ. Buried metaplasia after endoscopic ablation of Barrett's esophagus: a systematic review. Am J Gastroenterol 2011; 106(11): 1899-908. [ Links ]
35. Lyday WD, Corbett FS, Kuperman DA, Kalvaria I, Mavrelis PG, Shughoury AB, et al. Radiofrequency ablation of Barrett's esophagus: outcomes of 429 patients from a multicenter community practice registry. Endoscopy 2010; 42(4): 272-8. [ Links ]
36. Pouw RE, Wirths K, Eisendrath P, Sondermeijer CM, Ten Kate FJ, Fockens P, et al. Efficacy of radiofrequency ablation combined with endoscopic resection for Barrett's esophagus with early neoplasia. Clin Gastroenterol Hepatol 2010; 8(1): 23-9. [ Links ]
37. Shaheen NJ, Frantz DJ. When to consider endoscopic ablation therapy for Barrett's esophagus. Curr Opin Gastroenterol 2010; 26(4): 361-6. [ Links ]
38. Shand A, Dallal H, Palmer K, Ghosh S, MacIntyre M. Adenocarcinoma arising in columnar lined oesophagus following treatment with argon plasma coagulation. Gut 2001; 48(4): 580-1. [ Links ]
39. Van Laethem JL, Peny MO, Salmon I, Cremer M, Deviere J. Intramucosal adenocarcinoma arising under squamous re-epithelialisation of Barrett's oesophagus. Gut 2000; 46(4): 574-7. [ Links ]
40. Soehendra N, Seewald S, Groth S, Omar S, Seitz U, Zhong Y, et al. Use of modified multiband ligator facilitates circumferential EMR in Barrett's esophagus (with video). Gastrointest Endosc 2006; 63(6): 847-52. [ Links ]
41. Beaumont H, Gondrie JJ, McMahon BP, Pouw RE, Gregersen H, Bergman JJ, et al. Stepwise radiofrequency ablation of Barrett's esophagus preserves esophageal inner diameter, compliance, and motility. Endoscopy 2009; 41(1): 2-8. [ Links ]
42. Fleischer DE, Overholt BF, Sharma VK, Reymunde A, Kimmey MB, Chuttani R, et al. Endoscopic radiofrequency ablation for Barrett's esophagus: 5-year outcomes from a prospective multicenter trial. Endoscopy 2010; 42(10): 781-9. [ Links ]
43. Gondrie JJ, Pouw RE, Sondermeijer CM, Peters FP, Curvers WL, Rosmolen WD, et al. Effective treatment of early Barrett's neoplasia with stepwise circumferential and focal ablation using the HALO system. Endoscopy 2008; 40(5): 370-9. [ Links ]
44. Pouw RE, Gondrie JJ, Sondermeijer CM, Ten Kate FJ, van Gulik TM, Krishnadath KK, et al. Eradication of Barrett esophagus with early neoplasia by radiofrequency ablation, with or without endoscopic resection. J Gastrointest Surg 2008; 12(10): 1627-36. [ Links ]
45. Sharma VK, Jae KH, Das A, Wells CD, Nguyen CC, Fleischer DE. Circumferential and focal ablation of Barrett's esophagus containing dysplasia. Am J Gastroenterol 2009; 104(2): 310-7. [ Links ]
46. Okoro NI, Tomizawa Y, Dunagan KT, Lutzke LS, Wang KK, Prasad GA. Safety of prior endoscopic mucosal resection in patients receiving radiofrequency ablation of Barrett's esophagus. Clin Gastroenterol Hepatol 2012; 10(2): 150-4. [ Links ]
47. Ganz RA, Overholt BF, Sharma VK, Fleischer DE, Shaheen NJ, Lightdale CJ, et al. Circumferential ablation of Barrett's esophagus that contains high-grade dysplasia: a U.S. Multicenter Registry. Gastrointest Endosc 2008; 68(1): 35-40. [ Links ]
48. van Vilsteren FG, Pouw RE, Seewald S, Alvarez HL, Sondermeijer CM, Visser M, et al. Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett's oesophagus with high-grade dysplasia or early cancer: a multicentre randomised trial. Gut 2011; 60(6): 765-73. [ Links ]











 text in
text in