Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.2 Bogotá Apr./June 2013
Case study of a sphincterotomy to remove stones from the common bile duct cholelithiasis biliary in a patient with total situs inversus
Denny Javier Castro, MD (1), Alejandro De Faria, MD (1), Lisbeth Fuenmayor, MD (1)
(1) Dr Luis E Anderson Center for Gastrointestinal Cancer Control in San Cristobal, Tachira State, Venezuela.
Received: 11-02-13 Accepted: 16-04-13
Abstract
Situs inversus is an autosomal recessive condition characterized by of thoracic and abdominal organs in mirror image locations. It is classified into total and partial situs inversus. There is a complete transposition of thoracic and abdominal organs in total situs inversus while there is partial transposition of one or more organs in partial situs inversus. The incidence of this condition ranges from 0.002% to 1%. Although this entity does not usually affect an individual's longevity, the patient's clinical picture is different than that of other people. Consequently when the condition has not already been diagnosed, an endoscopist or surgeon is likely to be surprised. We report the case of a 38 year old female patient who consulted for pain in the left upper abdominal quadrant. She suffered from biliary colic and had an altered liver profile. Abdominal ultrasound showed transposition of the liver and common bile duct to the upper left abdominal quadrant as well as a dilated common bile duct with gallstones. ERCP (endoscopic retrograde cholangiopancreatography) was requested. Cardiovascular assessment with chest x-ray showed dextrocardia. Abdominal computed tomography corroborated the diagnosis of total situs inversus. An MRCP (Magnetic Resonance Cholangiopancreatogram) showed dilation of the distal common bile duct within which were two stones. An ERCP showed that the papilla was larger on the right and was rotated 180°. A sphincterotomy was performed, and the cholesterol stones were extracted. This case shows the importance of preoperative diagnosis for addressing the bile duct in patients with situs inversus.
Keywords
Total situs inversus, choledocholithiasis.
INTRODUCTION
Situs inversus is an autosomal recessive entity expressed in the transposition of the abdominal and thoracic organs. It is classified as total or partial. Total situs inversus consists of complete reversal of both thoracic and abdominal organs while partial situs inversus only affects one or more organs (1, 2). The incidence of situs inversus varies from 0.002% to 1%, but is more common in men. Although this condition does not affect life expectancy or quality of life (1,3), it does demand greater attention from surgeons and endoscopists because diagnosis can be confusing and because this condition influences approach and/or invasive procedures such as ERCP. For this reason we present the case of a patient with choledocholithiasis who came to the Dr Luis E Anderson Center for Gastrointestinal Cancer Control in San Cristobal, Tachira State, Venezuela.
CLINICAL CASE
A 38 year old female patient from Edo Tachira who had suffered from cramping pain in the left upper quadrant of the abdomen from January 13, 2012 was referred for treatment. She had developed jaundice in late January and then developed intense itching on February 10, 2012. Upon admission to the Hospital Central de San Cristobal she was referred to the CCCGI for assessment and management.
Family History: The patient's mother had died from lung cancer and her father had died of Chagas disease (American trypanosomiasis).
Personal History: The patient said she had no medical conditions, surgery or drug allergies.
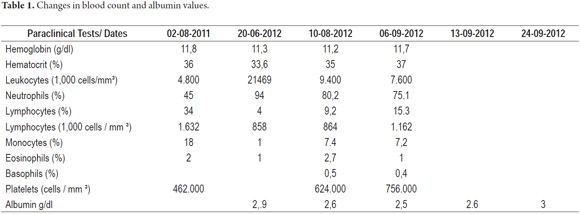
Physical examination: the patient was clinically stable with jaundiced skin and conjunctiva. Patient experienced pain on deep palpation of the left upper abdominal quadrant. A complete blood count and a liver profile reported the listed in Table 1.
Hepatobiliary ultrasound: Cholelithiasis (gall stones), dilated common bile duct, liver and gallbladder transposed to the left upper abdominal quadrant.
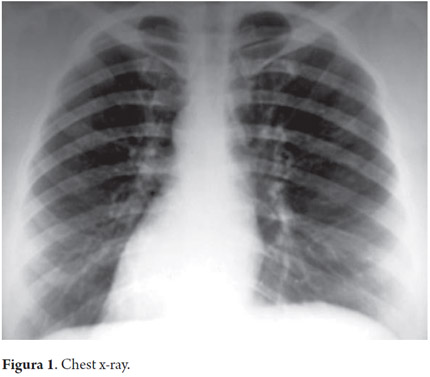
Given that clinical and paraclinical examinations indicated extrahepatic cholestasis, it was decided to perform ERCP. A posteroanterior chest x-ray during preoperative cardiovascular assessment showed dextrocardia (Figure 1).
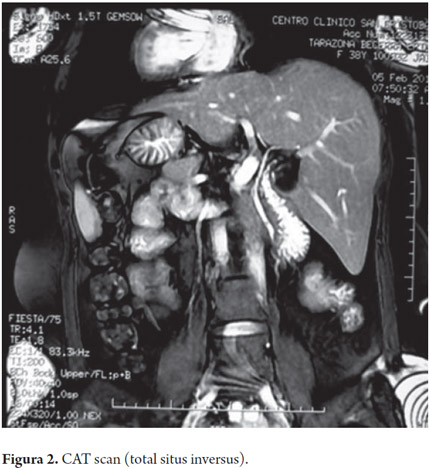
An abdominal CAT scan corroborated total situs inversus (Figure 2). Cholangioresonance showed limited dilation of the distal common bile duct with two images of lesions inside (Figure 3).
An ERCP was scheduled (Figure 4). A biliary sphincterotomy was performed in a 1 to 3 maneuver with a 180° orientation to the left. The biliary duct was entered and the defects observed in images of the distal third were extracted with a Fogarty balloon. They were cholesterol gallstones.
DISCUSSION
Situs inversus is an uncommon condition. This case presented total situs inversus in a female patient. This is similar to the case described by Serna et al., although in that case the patient was partially situs inversus (1), but contrasts to findings in the literature in which this entity most often occurs in men (1, 2, 3). Aristotle discovered this alteration in animals while in humans it was first described by Fabricius in 1600. Vehemeyer first identified situs inversus in 1867 with X-rays (4, 5). Clinical manifestations depend on the location of the compromised organ. In this case, it was a biliary obstruction in the upper left abdominal quadrant. In 1949, Blegen reported diagnostic errors in 45% of all patients with situs inversus with incorrect incisions in 31% of patients operated on for gall stones. Currently this type of error has been minimized because we have an arsenal of noninvasive imaging methods to arrive at preoperative diagnoses when there is a clinically suspect premise (5). We have presented this case for these reasons and to emphasize the importance of physical examination combined with imaging studies for diagnosis in order to achieve a diagnosis prior to an invasive procedure. In this case the ERCP was performed after taking care to modify the usual approach to the papilla via the basic anatomical variant.
REFERENCES
1. de la Serna-Higuera C, Pérez-Miranda M, Flores-Cruz G, Gil-Simon P, Caro-Patton A. Endoscopic retrograde cholangiopancreatography in situs inversus partialis. Endoscopy 2010; 42: E98. [ Links ]
2. Melchor JM, Pérez R, Torres M, Rodríguez V. Situs inversus: Reporte de dos casos. Cir Ciruj 2000; 68: 72-75. [ Links ]
3. Venu RP, Geenen JE, Hogan WJ, Johnson GK, Taylor AJ, Stewart ET, et al. ERCP and endoscopic sphincterotomy in patients with situs inversus. Gastrointestinal Endosc 1985; 31: 338-340. [ Links ]
4. Fiocca F, Donatelli G, Ceci V, Cereatti F, Romagnoli F, Simonelli L, et al. ERCP in total situs inversus viscerum. Case Rep Gastroenterol 2008; 2: 116-120. [ Links ]
5. Blegen HM. Surgery in situs inversus. Ann Surg 1949; 129: 244-259. [ Links ]











 text in
text in