Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.3 Bogotá jul./set. 2013
Case Report and Literature Review of Idiopathic Intussusception in an Adult
Gustavo Poveda P., MD. (1), Héctor Adolfo Polanía L., MD. (2), Fermín Canal D., MD. (3), Kevin Fernando Montoya Q., MD. (4), Héctor Conrado Jiménez S., MD. (5)
Hospital Universitario Hernando Moncaleano Perdomo and Universidad Surcolombiana in Neiva, Colombia
(1) General Surgeon, Associate Professor of General Surgery at the Universidad Surcolombiana and the Hospital Universitario Hernando Moncaleano Perdomo in Neiva, Colombia.
(2) Clinical Gastroenterological Surgeon, Epidemiologist, Associate Professor and Chief of the Department of Clinical Sciences at the Universidad Surcolombiana and the Hospital Universitario Hernando Moncaleano Perdomo in Neiva, Colombia.
(3) General Surgeon and Tenured Professor of General Surgery at the Universidad Surcolombiana and the Hospital Universitario Hernando Moncaleano Perdomo in Neiva, Colombia.
(4) Medical Resident III in General Surgery at the Universidad Surcolombiana and the Hospital Universitario Hernando Moncaleano Perdomo in Neiva, Colombia.
(5) General Practitioner from the Universidad del Tolima at the Hospital Universitario Hernando Moncaleano Perdomo in Neiva, Colombia.
Received: 28-01-13 Accepted: 26-06-13
Abstract
Intussusception is a rare cause of intestinal obstruction in adults. Only about 3 cases per million people are reported in the literature each year. It is an uncommon condition that is more prevalent in children. In adults, it is most often associated with neoplasms, postoperative scars, Meckel's diverticulum, foreign bodies or celiac disease, but 20% of these cases have idiopathic causes. We present a case and review of the literature.
Key words
Intussusception, intestinal obstruction, idiopathic.
INTRODUCTION
Only 5% of all cases of intussusceptions occur in adults explains, and intussusceptions account for only 1% to 5% of the causes of intestinal obstruction (1). The pathophysiology of adult intussusception is distinct from pediatric intussusception in several ways. The cause of pediatric intussusception is usually primary and benign and can be resolved with enemas or endoscopically. In this population, reduction of the intussusception is sufficient to treat the condition in 80% of patients (2).
In contrast, nearly 90% of adult intussusception cases are secondary to pathological conditions that serve as a trigger for the process of invagination. This is how neoplasms, polyps, Meckel's diverticulum, colonic diverticula and benign strictures are usually discovered during surgery. All of these can cause this phenomenon (3). Due to the significant risk of associated malignancy, which can be up to 65%, decompression guided by endoscopy or radiology should not be the definitive treatment. For this reason, approximately 70% to 90% of cases of intussusception in adults require surgical treatment (4).
CASE REPORT
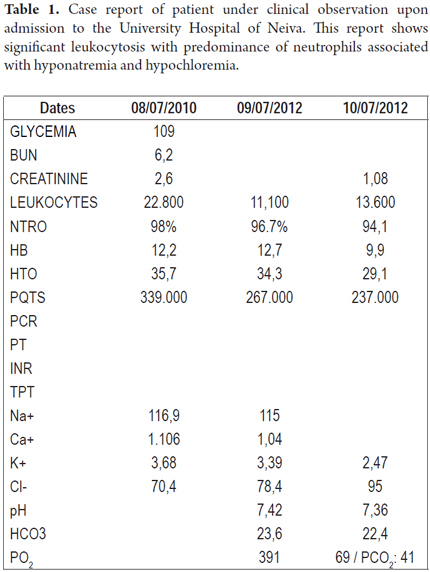
The patient, a teenage boy with a history of mild mental retardation, came to the emergency department of the Hospital Universitario de Neiva in the company of his father after having suffered 15 days progressive hypogastric pain ranging in intensity from 5/10 to 9/10. He experienced bloating and episodes of vomiting, but had had no bowel movement from the onset of symptoms. Physical examination upon admission showed patient was suffering pain and had signs of dehydration grade II without oral tolerance. His blood pressure was 110/70, his heart rate was 125/minute, and his temperature was 37.9o. His oral mucosa was dry and he had tachycardia. His abdomen was distended but was without pains on palpation and Blumberg's sign was absent. There were no overt signs of peritoneal irritation. Bowel sounds were present, but diminished. Paraclinical tests and x-rays were requested (Table 1 and Figure 1).
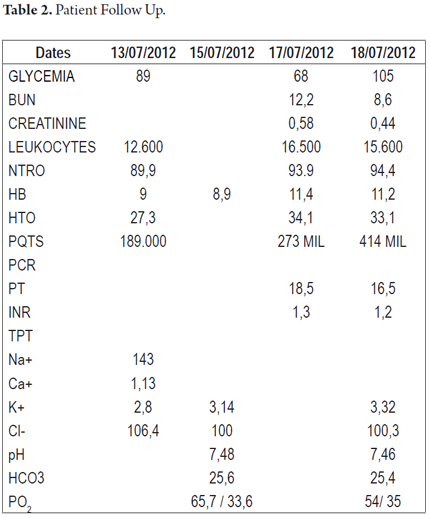
The abdominal x-ray taken upon admission was consistent with intestinal obstruction (Figure 1) and electrolyte disturbance (hyponatremia, hypochloremia, and hypokalemia) (Table 2). After evaluation, a diagnosis of abdominal sepsis was presumed. A nasal-gastric tube was placed, targeted resuscitation began, and antibiotics were administered. A decision was made to perform an exploratory laparotomy which found intestinal intussusception in the jejunum 20 cm away from the ligament of Treitz. The intussusception compromised approximately 50 cm of intestine, but had no apparent cause. During this procedure, no evidence of macroscopic perforation of the compromised segment was found, but patchy areas of necrosis were found.
METHOD
We drained the peritonitis and performed jejunal resection plus an end-to-end jejunal anastomosis (bi-plane) and peritoneal lavage. The strategy of on-demand relaparotomy was adopted and the patient was transferred to the hospital wards.
Patient's development was torpid with bloating and an absence of bowel sounds. Another laparotomy was performed 48 hours later. An abundance of fetid peritoneal fluid and fibrin membranes were found in several different collections. The on-demand relaparotomy strategy was replaced with a strategy of laparotomy in stages combined with use of a vacuum-assisted closure system. This procedure required three serial surgical scrubs and transfer of the patient to the intensive care unit because of hemodynamic instability. Two days later, when the patient became stable, he was transferred to a hospital ward. When morganella morganii and E. coli were found in the culture of peritoneal fluid, the dosage of antibiotics was increased by the addition of 1 gram per day of intravenous ertapenem for fourteen days. The pathology report concluded: segmental resection of the jejunum with extensive necrosis and severe acute inflammation of the serosa plus intussusception. The patient evolved appropriately without signs of systemic inflammatory response. The open incision in the abdomen was managed with the vacuum-assisted closure system. Once the criteria were met for abdominal wall closure, the procedure was performed without complications. Following closure, the patient was released from the general surgery service on condition of outpatient checkups.
DISCUSSION
The telescoping of a segment of the gastrointestinal tract with its mesentery (intususceptum) towards the lumen of a contiguous segment (intususcipiens) is called intussusception.
In adults, the primary cause of idiopathic intussusception occurs in approximately 20% of cases (5). The loops of the small intestinal are most frequently involved. The underlying process can begin from any pathological lesion of the intestinal wall. In a few cases, the process begins with the presence of an irritant in the intestinal lumen that alters normal peristaltic activity. This triggers the onset of intussusception of a segment involved in the bowel. The intussusception could be described as an "internal prolapse" of the proximal bowel and its mesenteric fold. The prolapse of the mesenteric fold into the lumen of the adjacent distal bowel segment results in an alteration of peristalsis which obstructs the free passage of intestinal contents. Most seriously, it compromises the mesenteric vascular flow in the intussuscepted segment (6). The final result is derived from the presence of an intestinal obstruction associated with inflammatory changes along the entire thickness of the intestinal wall. This can cause ischemia and subsequent perforation of the compromised viscera (7).
The most common locations of intussusceptions are the points that share freely moving segments and have fixed attachments to the retroperitoneum. This condition has been classified into four categories according to anatomical locations. Entero-enteral is confined to the small intestine (as in our patient), colo-colic involves the large intestine, and ileo-colic is a prolapse of the terminal ileum into the ascending colon. Ileocecal indicates that the ileocecal valve is the main point of intussusception.
Another system classifies intussusceptions according to underlying causes: benign, malignant and idiopathic. Intussusception may be secondary to the presence of intra-or extra-luminal lesions or conditions such as inflammatory bowel disease, Meckel's diverticulum, postoperative adhesions, lipomas, adenomatous polyps, carcinomas, (lymphomas or metastases) and the presence of foreign bodies in the intestinal lumen. Some of these may be elements related to management of other diseases of the gastrointestinal tract. Neoplasia and malignant tumors, in particular adenocarcinoma, account for up to 30% of cases of intussusception in the small intestine and 66% of those occurring in the large intestine (8).
Clinical evidence indicating adult intussusception varies considerably. Symptoms are non-specific, and in most of the cases chronic symptoms reported are consistent with partial bowel obstruction.
A retrospective study by the Mayo Clinic has shown that the most common symptoms associated with the disease are abdominal pain (94%), nausea (76%), vomiting (65%), diarrhea (30%) and bloody stools (15%). Up to 2% of these patients may be asymptomatic when admitted to the emergency room (9).
The classic presentation of pediatric acute intussusception features a triad of colicky abdominal pain, bloody diarrhea, and the presence of a palpable mass. This situation is rare in adults. The presence of nausea, vomiting, gastrointestinal bleeding and changes in bowel functioning such as constipation or bloating are nonspecific (10).
Preoperative diagnosis of intussusception is made difficult by the variability of clinical presentation and presence of dissimilar characteristics make difficult an accurate. Reijnen et al. reported that only 50% of diagnoses were made prior to surgery, while Eisen et al. reported a rate of preoperative diagnoses of only 40%. (10-11). A flat abdominal x-ray is often the first diagnostic tool to consider, since in most cases the obstructive symptoms dominate the clinical picture. The x-ray can not only help identify whether there is intestinal obstruction, but can also identify the site of obstruction. An image of "stacked coins" or of a "ladder" combined with the presence of fluids is pathognomonic of bowel obstruction. A barium enema may be useful for patients with colo-colic or ileo-colonic intussusception. Images showing a cup presented by a filled defect and those that appear as "spiral" or "coiled springs" are hallmarks of intussusception (12). Ultrasound is a useful tool for diagnosis of intussusception in children and adults. The characteristics of the classic images include the target and donut shapes found in cross section views and pseudo-kidney and pitch fork shapes found in the longitudinal section. Nevertheless, ultrasound images require management and interpretation by an experienced radiologist in order to confirm the diagnosis (13). Computed tomography (CT) is the most sensitive and specific imaging method for diagnosis of intussusception. Its sensitivity ranges from 58% to 100%. A CT scan can show the location, the nature of the mass, and its relationship to surrounding tissues. In addition, a CT scan can be used to stage patients with intussusception secondary to malignancy. The presence of an image within the intestinal loop, with or without mesenteric vessels and fat, is pathognomonic of intussusception. Mesenteric vessels are reported in 68% to 76% of cases while the presence of fat is reported in 54% to 61% of cases. When an image of a target is seen, the intususceptum is at the center, and the edema is seen as the outer rings of the target. The presence and configuration of the head of the intususceptum head, the degree of edema in the wall of the intususcipiens, and the amount of invaginated mesentery are factors that may distort the characteristic radiographic findings (14).
Obesity and the presence of air distending the bowel are conditions that can interfere with the quality of images, and hence the diagnosis of the condition.
For cases of sub-acute or chronic intestinal obstruction in the lower gastrointestinal tract flexible colonoscopy can play a fundamental role in diagnosis since it not only allows the diagnosis of intussusception but also makes it possible to identify the presence of masses or polyps which cause the intussusception. Endoscopic polypectomy is not the best idea for treatment of patients with chronic intussusception in whom polypoid mass has been detected because of the high risk of perforation after resection and the risk tissue ischemia around the polyp. Resecting the intussusception should not be considered if there are signs of ischemia or inflammation in the intestinal lumen (15).
Most surgeons agree that intussusception in adults requires surgical intervention because of the large number of structural anomalies and the high incidence of cancer. Nevertheless, the extent of resection of the intestine and the manipulation of the intussuscepted bowel during resection remain controversial. This contrasts with pediatric patients for whom the source of invagination is benign and primary allowing reduction to be performed with barium or air. For adults, surgery is the definitive treatment. Some theoretical risks of treating the intussuscepted segment are dissemination of the tumor either intraluminally or through blood vessels, dissemination of the tumor to the peritoneal cavity, perforation, and bacteremia (16). The reduction must not be attempted if there are signs of inflammation or ischemia on the intestinal wall. For patients with ileo-colic, ileus-cecal and colo-colic invagination, especially those over 60 years old who frequently have intestinal neoplasia as an etiological factor, resection of the compromised segment of the intestine with appropriate oncological edges should be performed (17).
Azar et al. recommend that resection and primary anastomosis can be performed on unprepared intestines if the invagination is on the right side of the colonic segment. When the invagination is on the left side of the colonic segment or in the binding rectosigmoid, they recommend resection with subsequent ostomy of Hartmann's pouch followed later by repeat anastomosis which they consider safer, especially in the context of an emergency. Nevertheless, when the preoperative diagnosis of the cause of intussusception is a benign tumor, the surgeon can reduce the intussusception by the distal or proximal segment. When intussusception is caused by familial adenomatous polyposis syndromes such as Peutz Jeghers syndromes, a combined approach with limited bowel resections and multiple polypectomies is the treatment of choice.
Several reports of laparoscopic reduction of intussusception have been published. They show that laparoscopy has been used successfully in selected cases. This depends on the availability of experienced surgeons. After laparoscopically establishing the diagnosis of intussusception and its underlying disease, this method can be used to reduce and/or resect en bloque (18). Finally, the relative rarity of this clinical condition in adults combined with multiple differential diagnoses related to abdominal pain can result in missed diagnoses that delay correct treatment. This can result in dire consequences for the patient. This is the reason why we must become familiar with this condition and learn to identify it in specific situations (19).
REFERENCES
1. Azar T, Berger DL. Adult intussusception. Ann Surg 1997; 226: 134-138. [ Links ]
2. Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol 2009; 15(4): 407-11. Review. [ Links ]
3. Akcay MN, Polat M, Cadirci M, Gencer B. Tumor-induced ileo-ileal invagination in adults. Am Surg 1994; 60: 980-981. [ Links ]
4. Behrman RE, Kliegman RM, Jenson HB, Editors, Nelson textbook of pediatrics. 16th ed. Philadelphia: W.B. Saunders; 2000. p. 1142-3. [ Links ]
5. Haas EM, Etter EL, Ellis S, Taylor TV. Adult intussusception. Am J Surg 2003; 186: 75-7. [ Links ]
6. Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 1997; 173: 88-94. [ Links ]
7. Erkan N, Haciyanli M, Yildirim M, Sayhan H, Vardar E, Polat AF. Intussusception in adults: an unusual and challenging condition for surgeons. Int J Colorectal Dis 2005; 20: 452-456. [ Links ]
8. Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, Kuwano H. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol 2003; 36: 18-21. [ Links ]
9. Lindor RA, Bellolio MF, Sadosty AT, Earnest F 4th, Cabrera D. Adult intussusception: presentation, management, and outcomes of 148 patients. J Emerg Med 2012; 43(1): 1-6. [ Links ]
10. Martin-Lorenzo JG, Torralba-Martinez A, Liron-Ruiz R, Flores-Pastor B, Miguel-Perello J, Aguilar-Jiménez J. Intestinal invagination in adults: preoperative diagnosis and management. Int J Colorectal Dis 2004; 19: 68-72. [ Links ]
11. Boyle MJ, Arkell LJ, Williams JT. Ultrasonic diagnosis of adult intussusception. Am J Gastroenterol 1993; 88: 617-618. [ Links ]
12. Gayer G, Apter S, Hofmann C, Nass S, Amitai M, Zissin R, Hertz M. Intussusception in adults: CT diagnosis. Clin Radiol 1998; 53: 53-57. [ Links ]
13. Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, Kohneh-Sharhi N, Lehur PA, Hamy E. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis 2006; 21: 834-839. [ Links ]
14. Bermúdez Ch. Intususcepción intestinal en adultos por lesiones benignas Rev Col Gastroenterol 2011; 26(2): 156-159. [ Links ]
15. Lin BC, Lien JM, Chen RJ, Fang JF, Wong YC. Combined endoscopic and surgical treatment for the polyposis of Peutz-Jeghers syndrome. Surg Endosc 2000; 14: 1185-1187. [ Links ]
16. McKay R. Ileocecal intussusception in an adult: the laparoscopic approach. JSLS 2006; 10: 250-253. [ Links ]
17. Behara S, Ahmed N, Attar BM, Hussein R. Primary intussusception in adult. Am J Gastroenterol 2001; 96: 180. [ Links ]
18. Medina-Franco H, Ramos-de la Medina A, Arista-Nasr J. Intususcepción en adultos: presentación de un caso con etilogía poco común y revisión de la literatura. Rev Gastroenterol Mex 2002; 67: 103-6. [ Links ]
19. Traoré D, Sissoko F, Ongoïba N, Traoré I, Traoré AK. Adult intussusception: diagnostic pitfalls, morbidity and mortality in a developing country AK. J Visc Surg 2012; 149(3): e211-4. [ Links ]











 texto em
texto em