Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.4 Bogotá Oct./Dec. 2013
Characterization of patients with non-varicose upper GI bleeding at a Level 3 Hospital in Cundinamarca, Colombia
Daysi Rivera H. MD. (1), Julián David Martínez M., MD (2), José Rafael Tovar C. MD. PhD. (3), Martín Alonso Garzón O. MD. (1), Natan Hormaza A. MD. (1), Jorge I. Lizarazo, MD. (1), Juan Carlos Marulanda G., MD. (1), Juan Carlos Molano V., MD. (1), Mario Humberto Rey Tovar, MD. (1)
(1) Gastroenterology Unit at the Hospital Universitario de la Samaritana in Bogotá, Colombia.
(2) National University of Colombia, Faculty of Medicine, Gastroenterology Unit and the Gastroenterology Unit at the Hospital Universitario de la Samaritana in Bogotá, Colombia.
(3) Epidemiologist at the Universidad del Rosario in Bogotá, Colombia.
Received: 25-02-13 Accepted: 27-08-13
Abstract
Upper gastrointestinal tract bleeding is a common emergency whose most common etiology is a peptic ulcer. Restoration of intravascular volume and blood pressure management are priorities before identifying the cause of bleeding. After initial resuscitation and after hemodynamic stabilization has been achieved, an esophagogastroduodenoscopy (EGD) should be performed to identify the cause of bleeding and determine the treatment needed. This is a study performed at a third level referral hospital in Cundinamarca, Colombia.
Materials and Methods: This is a retrospective study of data from electronic medical records of adult patients admitted to the emergency room of the Hospital Universitario de la Samaritana (HUS) because of upper gastrointestinal tract bleeding which ahd been diagnosed because of hematemesis, melena, rectal bleeding and/or anemia. Patients all underwent EGD between April 2010 and April 2011.
Results: 385 patients with upper gastrointestinal tract bleeding were seen during the study period, but 100 were excluded because of bleeding secondary esophageal varices, incomplete clinical histories and lower gastrointestinal bleeding. A total of 285 patients were included. 69.1 % were older than 60 years, 73.3 % had hypertension, 55.1 % reported use of inflammatory drugs (NSAIDs) and aspirin (ASA), 19.6 % reported previous bleeding episodes, and 17.9 % had hemodynamic instability. 63 patients (22.1 %) required endoscopic hemostasis, and 32 (11.2 %) experienced rebleeding. Overall mortality reported was 13.1 % of which 55.3 % were men. Mortality attributable to gastrointestinal bleeding was 3.1 %.
Conclusions: The majority of patients served by the HUS with upper GI bleeding are adults over 60 years. Peptic ulcers remain the most common diagnosis associated with the use of NSAIDs and ASA. The mortality rate is comparable to international standards.
Keywords
Upper GI bleeding, esophagogastroduodenoscopy, hemostasis, mortality.
INTRODUCTION
High-digestive tract hemorrhaging (HDTH) is defined as hemorrhaging originating in a lesion situated above the Treitz angle. (1) It manifests clinically in the form of hematemesis (vomiting of fresh blood), melenemesis (vomiting of dark colored material), melena or both and less frequently as rectal bleeding (hematochezia). (2) HDTH is divided into hemorrhaging originating in varices and hemorrhaging with origins other than bleeding caused by gastric esophageal varicose veins due to portal hypertension. The most frequent causes of non-varicose HDTH are gastric and duodenal peptic ulcers which account for around 70% of the cases. HDTH may also be originate in acute lesions of the gastric mucous, esophagitis, neoplasias, vascular lesions or Mallory Weiss syndrome. (3) Non-varicose HDTH is frequent in hospital emergencies, with an annual incidence between 50 and 150 cases per 100.000 inhabitants. Nearly 30% of patients with bleeding peptic ulcers present hematemesis, 20% present melena and 50% present both. (1-3)
Patients with HDTH enter the hospital in highly variable clinical conditions which range from the simple presence of melena with blood loss between 50-100 ml without hemodynamic compromise (4) to serious life threatening conditions with massive bleeding and hypovolemic shock (which is defined as blood pressure lower than 90/60 mm Hg and cardiac frequency greater than 100 beats/minute). (5) HDTH is the main reason for emergency admissions to gastroenterology wards despite advances in diagnosis and treatment. Mortality rates have remained stable between 5% and 10% during the last two decades when all patients with non-varicose HDTH are included without differentiating between etiologies. (6)
Esophagogastroduodenoscopy (EGD) is the cornerstone for diagnosing and managing patients since it usually allows establishment of the cause of hemorrhaging, determination of the presence or absence of active bleeding during the exam, and prediction of the occurrence of rebleeding. It offers multiple treatment options for stopping bleeding and preventing reoccurrence. (1) When patients present HDTH, crucial prognostic factors include age: (7) age, presence of associated diseases, and hypovolemic shock. Among patients over 60 years old there is a greater chance of rebleeding and mortality rates can be as high as 39%. Associated diseases and conditions include cardiac insufficiency, chronic obstructive pulmonary disease, renal insufficiency, diabetes mellitus, neurological alterations, and anticoagulation. Patients suffering hypovolemic shock show hemodynamic instability upon admission and have poor prognoses. The main prognostic factor for mortality is premature rebleeding in the first 72 hours. This occurs in up to 20% of the patients. (8) All this is due mainly to the progressive aging of the population and to the increasing proportion of patients of advanced age with associated diseases who use more NSAID and ASA, and whose management presents great challenges because they are less tolerant of hemodynamic alterations. (9) The objective of this study was to describe clinical characteristics, diagnostic and therapeutic interventions, and clinical outcomes among patients who presented HDTH at the Hospital Universitario de la Samaritana (HUS) in Cundinamarca.
MATERIALS AND METHODS
This is a retrospective descriptive study based on data obtained from the computerized clinical history of patients over the age of 18 who had been admitted to the emergency department of the Hospital Universitario de la Samaritana (HUS) because of HDTH. HDTH was diagnosed in patients with hematemesis, melena, rectal bleeding and anemia who were treated in the gastroenterology ward and underwent EGDs between April 2010 and April 2011. Patients who presented hemorrhaging secondary to esophageal varices, patients whose clinical histories were incomplete, and patients who presented HDTH while already hospitalized were excluded. Patients' records for HDTH were used to obtain demographic information, medical backgrounds, characteristics of pathologies that caused bleeding, and information about endoscopic and surgical treatment (Figure 1).
Informed consent was obtained from each patient and/or a relative prior to performance of EGDs. Procedures were performed without sedation but with topical anesthesia. Patients fasted for at least 6 hours before the procedure. Seven gastroenterologists performed the procedures in this study. An Olympus GIF 0150 videoscope with an Exera II CV 180 processor (Japan) was used for procedures and a solution of 1% epinephrine (Sandelson Lab, Colombia) diluted 1:10,000 in normal saline solution (NSS) at was used for hemostasis. The needles used were Willson Cook (USA) LVDI-23, the heat probe was an ERBE ICC 200 (Germany), and the argon plasma equipment used for photocoagulation therapy was an Excell NHP 400/DA (Italy).
After performing the initial endoscopic procedure, physicians determined whether or not rebleeding had occurred. Rebleeding was defined as new hematemesis with fresh red blood and/or melena with hypotension or hemoglobin values below 2g/dl. Endoscopic findings and treatment in cases which required endoscopic hemostasis were documented for each patient in writing by the gastroenterologist who performed the procedures. Follow up for hemostatic procedures was documented when the patients required a second EGD due to rebleeding while hospitalized. Associated comorbidities included arterial hypertension, nephropathy, neuropathy, and pneumopathy. Other information recorded included administration of commonly used non-steroid anti-inflammatories (NSAIDs) including ibuprofen, diclofenac, and naproxen, administration of aspirin (ASA), the use of oral anticoagulants, hemodynamic instability, previous episodes of HDTH, necessary endoscopic treatment, and blood transfusions. Patients were divided into three categories related to transfusions: those who did not require transfusion, those who required less than three packed red blood cell (PRBC) units, and those who required more than 3 PRBC units. Documented mortality within 30 days of an episode of bleeding was divided into two groups. The first consisted of deaths related to HDTH in which bleeding was uncontrollable through endoscopy, patients suffered refractory hypovolemic shock, and for which the death certificate indicated no other diagnosis for the primary cause of death. The second consisted of deaths which were unrelated to bleeding. This group included patients who entered the emergency unit due to HDTH but who presented decompensation from a subjacent pathology and/or complications associated with hospitalization.
STATISTICAL ANALYSIS
The data was analyzed using descriptive statistics and cross tabulations. Patient socio-demographic descriptions were calculated using simple frequency distributions for categorical variables and central tendency and dispersion measurements for quantitative variables. To analyze the relation between clinical variables with causes of high digestive tract hemorrhaging, the patients were grouped into those less than 60 years of age and those over 60 years of age. Association analysis was performed by chi-squared tests. A value of 0.05 was assumed as an acceptable maximum type I error for evaluation of the statistical hypothesis of association. Data analysis was performed with SPSS version 20 for Windows.
RESULTS
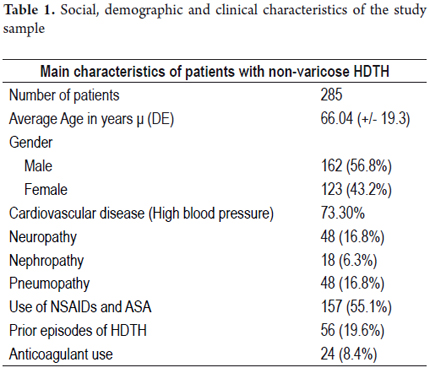
Of the 385 patients who met the initial criteria, 100 were excluded because they presented hemorrhaging secondary to esophageal varices, had incomplete clinical histories or had low digestive tract hemorrhaging. This left a total of 285 patients in the study: 56.8% (n=162) were men, 30.9% were less than 60 years old and 69.1% were over 60. It was observed that 55.3% of the 197 individuals who were over 60 years were men. Greater use of NSAID and ASA was documented (69.5%) in the group of patients over 60. The most relevant backgrounds were cardiovascular diseases including systemic arterial hypertension and ischemic cardiopathy affecting 73.3% of the study population and the use of NSAID and ASA by 55% (n=157 patients). 109 patients used ASA because of cardiovascular diseases and backgrounds of previous cerebrovascular diseases. Out of these patients, 90 were over 60. 48 patients (30.5%) took NSAID due to chronic pain. 19.4% had prior histories of HDTH, and 8.4% of this group received anticoagulants. Administration of warfarin because of backgrounds of deep vein thrombosis and/ or auricular fibrillation was documented. Patients who presented INRs greater than 2.5 received a transfusion of fresh frozen plasma prior to the EGD (Table 1).
All patients received 40mg ampules of omeprazole (Delta, Colombia) prior to the EGD. This was administered through an initial 80mg IV bolus followed by continuous infusion of 8mg/h for at least 48 to 72 hours until oral administration was tolerated at which time doses of 20mg began to be administered every 12 hours.
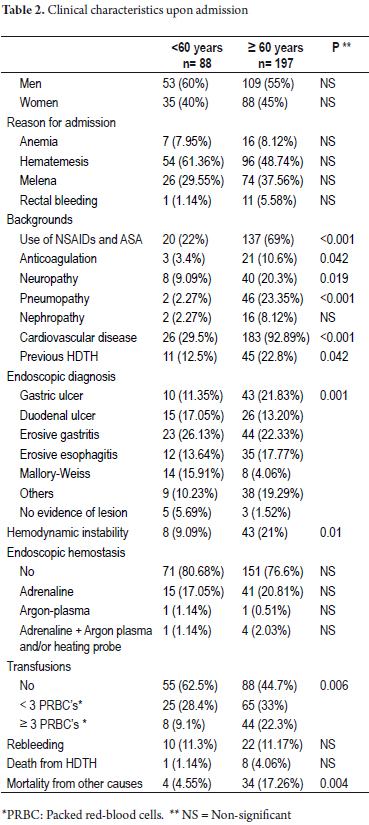
The most frequent reason for consultation was hematemesis (52.6%) followed by melena (35.1%). The lowest percentage suffered from rectal bleeding (4.2%). Twelve patients, seven women and five men, presented initial rectal bleeding. Their average age was 71.9 years (DE +/- 15.2). Five of these patients were documented as having Forrest III gastric ulcers while the rest of the patients had Forrest III duodenal ulcers. None merited endoscopic hemostasis. Fifty-one patients (17.9%), forty-three of whom were over sixty years of age, presented signs of hemodynamic instability. The most frequent diagnosis was a gastric ulcer (30.2%). The most frequently documented endoscopic diagnosis was peptic ulcers which were found in ninety four patients (33%), out of which 18.6% were gastric ulcers and 14.4% were duodenal ulcers. The least frequent endoscopic finding, Mallory Weiss syndrome, was found in 7.7% of the study group. Forty-seven patients (16.6%) presented other less frequent causes: fourteen (29.8%) had advanced gastric cancer, eight (2.8%) had no documented lesions. 142 patients (49.8%) received transfusions of hemoderivatives and fifty-two patients (36.7%) received 3 or more units of packed red blood cells (PRBC). Out of the 142 patients who received transfusion, ninety (63.3%) received less than three units of PRBC. Of these, nine presented rebleeding. Of the fifty-two patients who received more than three units of PRBC, twenty-three (44%) presented rebleeding during hospitalization. No rebleeding was observed in the 143 patients who did not receive transfusions. A total of thirty-two patients (11.2%) out of the entire study population of 285 patients presented rebleeding during hospitalization. All of them received dual endoscopic hemostasis during the second EGD (Table 2).
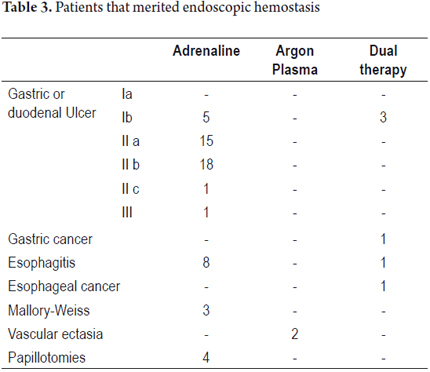
Of the 63 patients (22.1%) that required endoscopic hemostasis, 17 (19.3%) were less than 60 years old and 46 (23.3%) were over 60. The most frequent diagnoses for these patients were gastric and duodenal ulcers (65%) while the least frequent were gastric cancer and esophageal cancer (1.58% each) (Table 3).
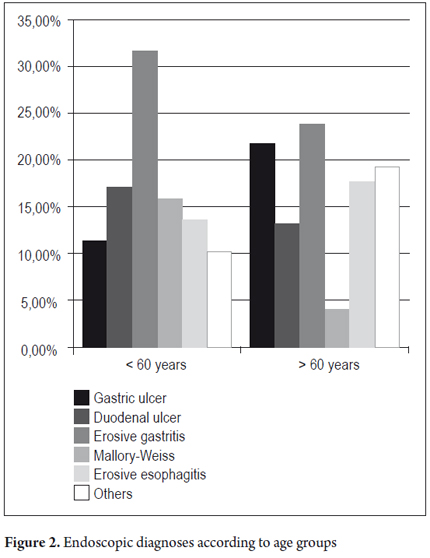
We found that patients over 60 used NSAIDs and ASA more frequently, had more associated comorbidities, and had more episodes of HDTH than those under 60. Also the most frequent endoscopic diagnoses among older patients were peptic ulcers (including both gastric and duodenal ulcers) which were found in 35.03% of these patients while the most common endoscopic diagnoses among younger patients were cases of erosive gastritis which was found in 31.82% of these patients No differences in mortality due to HDTH were found between the two age groups: 1.14% of patients under 60 died, and 4.06% of patients over 60 died (p 0.19). Nevertheless, the 17.26% mortality for all causes among patients over 60 was greater than the 4.55% mortality for all causes among patients under 60 (p 0.004). Global mortality reported during the hospitalization was 13.3%, out of which, 3.1% were due to HDTH. The remaining 10.2% were due to other causes such as associated nosocomial pneumonia and multi-organ failure.
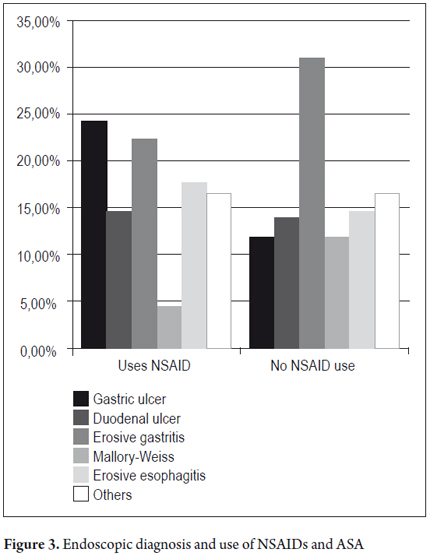
A significant statistical association was observed between bleeding and age (χ2=4.40, p=0.036) and bleeding and use of NSAIDs (χ2=7.261; p=0.007) (Figures 2 and 3).
Among the 53 cases of gastric ulcers, 66% were men, 81.1% were patients over 60, 71.7% reported having used NSAIDs and ADA, 24.5% were admitted to the emergency department with hemodynamic instability, 39.6% required hemostasis, and 66% required transfusions after admission. Out of this group of patients, six patients died. Three deaths were due to hemorrhaging from gastric ulcers, and three were secondary to hemorrhaging associated with decompensation due to associated comorbidities.
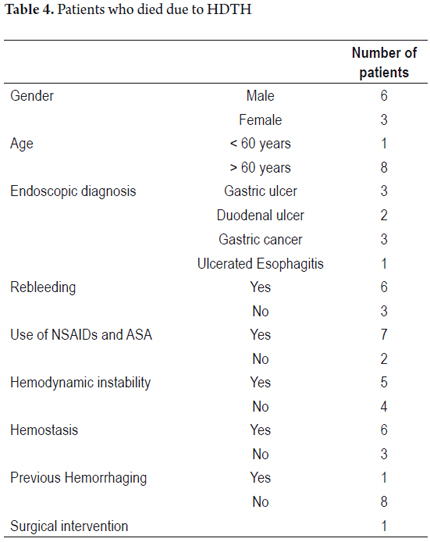
STUDY OF THE NINE DEATH CASES RELATED TO HDTH
Of the patients who died, the main cause of death in nine cases (24%) was HDTH: eight of these patients were over 60. One patient required urgent surgical management due to a perforated duodenal ulcer. The remaining 29 people died because of causes related to HDTH together with other complications associated with base pathologies (Table 4).
DISCUSSION
HDTH, a frequent cause of admission to the emergency department, requires integrated medical management. This study, performed at a referral hospital in the department of Cundinamarca, has shown that most of the patients received in the gastroenterology ward were over 60. This is due to the fact that this is a third-level referral hospital in which most of the patient consists of older adults. These patients also take NSAIDs, ASA and/ or anticoagulants more frequently than younger patients and are more likely to have more than one associated comorbidity. This concurs with studies in the literature. (10-12). It is worth mentioning that NSAIDs and ASA are taken in 55% of the cases, since most patients reported that the main indication for taking these medications was a diagnosis of high blood pressure. 19.6% of the patients reported at least one episode of HDTH prior to hospitalization, and 51 (17.9%) patients presented signs of hemodynamic instability which required stabilization through intravenous liquids (IVL) in order to obtain adequate urination and maintain arterial pressure which is the objective of initial management of patients with HDTH. (11)
The most frequently documented endoscopic diagnosis made with EGD's was a peptic ulcer (either gastric or duodenal). These findings do not differ from those reported globally: peptic ulcers continue to be the main cause of non-varicose HDTH. Nevertheless, it is worth mentioning that in our study, gastric ulcers represented a greater percentage (18.6%) than duodenal ulcers in contrast to what has been reported in most studies. (1) Although in the past peptic ulcers represented up to 70% of HDTH causes, recent studies have reported an important decrease in the percentage of peptic ulcer cases that result in hemorrhaging. The "Analysis of the Clinical Outcomes Research Initiative" reported on a population of patients who underwent EGDs because of high digestive tract hemorrhaging between December 1999 and July 2001. It said that 20.6% of the patients presented duodenal or gastric ulcers as the cause of bleeding. (13) The high percentage of patients whose bleeding was caused by erosive esophagitis, 16.5% of the total population, is worth mentioning. Thirty-five of these patients were over 60. This may be due to the fact that gastroesophageal reflux is more frequent and severe in the elderly. Gastric cancer was also documented in 4.95% of the total population which may be accounted for by the fact that GC is a frequent pathology in the Andean region of Colombia, especially in the high plains of Cundinamarca and Boyacá as reported in a previous study from our institution. (14)
Blood transfusions were given to 49.8% of the patients we reported on. This represents overuse of this resource since transfusions should be reserved for patients that have been previously reanimated through IVL but who remain hypotensive with active bleeding despite reanimation. (15) This is especially so since non-indicated transfusions can lead to greater morbidity and mortality. (16) It is worth mentioning that in our study, patients who received more than 3 units of PRBC presented more rebleeding that those who received less than 3 units (P 0.006). However, they were part of the group of patients who were over 60 and who had more associated comorbidities. The 11.2% of patients who experienced rebleeding in our study is less than the 20% reported in the literature. Possibly this is explained by the energetic reanimation performed at the referring site and in transit to our hospital, by timely endoscopic intervention during the first hours after hemodynamic stabilization, and medical management prior to performance of EGDs. Endoscopic hemostasis with adrenaline and/or argon plasma was required by 22.1% of the patients. Of these, 17 patients (53.1%) presented rebleeding. It is worth mentioning that in the cases that merited endoscopic hemostasis, only 19.6% were treated with endoscopic administration of adrenaline. This was left to the discretion of the gastroenterologist performing the procedure. The fundamental objectives of endoscopic treatment are to achieve hemostasis and to prevent recurrence. This notably decreases the need for surgical treatment and decreases mortality rates. (17) In our study, only the patient who had a perforated duodenal ulcer required urgent surgical management.
Although mortality rates reported in the last decade have oscillated between 5% and 10%, (18) in this study the mortality rate was 3.1%. This may be due to the initial energetic hemodynamic reanimation and to timely endoscopy. Significant statistical associations were observed between bleeding and age (χ2=4.40, p=0.036) and between bleeding and the use of NSAIDs (χ2=7.261; p=0.007). It has been proven that at greater ages patients ingest multiple drugs including NSAIDs and ASA which the literature has reported to be agents that can potentially damage the gastric mucosa. (19-22) This study showed that most patients with non-varicose HDTH who were admitted to the HUS emergency ward are older adults who present multiple associated risk factors including comorbidities such as HTA, nephropathy, and diabetes mellitus. These patients are also likely to have ingested multiple drugs including ASA and NSAIDs which has been positively associated with episodes of HDTH. (23-25) This is why we consider that an effort should also be directed to supportive care and/or to prevention of cardiovascular, renal and pulmonary complications instead of solely focusing on the gastrointestinal system. (9) There are many restrictions in our study. One is that the study was retrospective and descriptive which can lead to selection biases. Since the choice of endoscopic treatment performed was left to the discretion of each gastroenterologist who performed an EGD, a significant analysis regarding the impact of hemostatic methods on the risk of rebleeding cannot be performed with our data. We need to perform prospective studies in our institution in order to evaluate this association definitively. Due to the routine administration of blood transfusions involving more than 3 units of PRBC at the time of emergency department admission, we consider that a unified criterion for determining when patients should receive transfusions is needed.
CONCLUSIONS
In this study, the population admitted to our hospital (HUS) for HDTH consists of patients who are over 60 years old and who often have more than one associated comorbidity. Peptic ulcers, including gastric and duodenal ulcers, continue to be the most frequently diagnosed cause of HDTH. They are associated with the use of NSAIDs and ASA as has been reported in global literature. An exception may be diagnosis of gastric cancer which may have high prevalence because of the Andean region, as was mentioned previously. The success rates of the medical and endoscopic management we reported were similar to those reported in the literature since initial reanimation is fundamental in the management of any patient with HDTH. Documented mortality rates have remained the same in reports over the last two decades.
REFERENCES
1. Laine L, Peterson WL. Bleeding peptic ulcer. N Engl J Med. 1994;331:717-27. [ Links ]
2. Albeldawi M, Qadeer MA, Vargo JJ. Managing acute upper GI bleeding, preventing recurrences. Cleve Clin J Med. 2010;77:131-42. [ Links ]
3. Roberts-Thomson IC, Teo E. The changing face of non-variceal, upper gastrointestinal hemorrhage. J Gastroenterol Hepatol. 2007;22:1-3. [ Links ]
4. Gómez M, Pineda L, Ibáñez M, et al. Escala "UNAL" de predicción para identificar pacientes con hemorragia digestiva alta que necesitan endoscopia urgente. Acta Méd Colomb. 2006;31:389-99. [ Links ]
5. Lee JG, Turnipseed S, Romano PS, et al. Endoscopy-based triage significantly reduces hospitalization rates and costs of treating upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 1999;50:755-61. [ Links ]
6. González-González JA, Vázquez-Elizondo G, García-Compean D, et al. Predictors of in-hospital mortality in patients with non-variceal upper gastrointestinal bleeding. Rev Esp Enferm Dig. 2011;103:196-203. [ Links ]
7. Herrlinger K. [Classification and management of upper gastrointestinal bleeding]. Internist (Berl). 2010;51:1145-56. [ Links ]
8. Llach J, Bordas JM, Salmerón JM, et al. A prospective randomized trial of heater probe thermocoagulation versus injection therapy in peptic ulcer hemorrhage. Gastrointest Endosc. 1996;43:117-20. [ Links ]
9. Sung JJ, Tsoi KK, Ma TK, et al. Causes of mortality in patients with peptic ulcer bleeding: a prospective cohort study of 10,428 cases. Am J Gastroenterol. 2010;105:84-9. [ Links ]
10. Ferguson CB, Mitchell RM. Non-variceal upper gastrointestinal bleeding. Ulster Med J. 2006;75:32-9. [ Links ]
11. Feu F, Brullet E, Calvet X, et al. [Guidelines for the diagnosis and treatment of acute non-variceal upper gastrointestinal bleeding]. Gastroenterol Hepatol. 2003;26:70-85. [ Links ]
12. Kataoka M, Kawai T, Yagi K, et al. Clinical evaluation of emergency endoscopic hemostasis with bipolar forceps in non-variceal upper gastrointestinal bleeding. Dig Endosc. 2010;22:151-5. [ Links ]
13. Boonpongmanee S, Fleischer DE, Pezzullo JC, et al. The frequency of peptic ulcer as a cause of upper-GI bleeding is exaggerated. Gastrointest Endosc. 2004;59:788-94. [ Links ]
14. Martínez JD, Garzón MA, Lizarazo JI, et al. Características de los pacientes con cáncer gástrico del departamento de Cundinamarca, remitidos al Hospital Universitario de la Samaritana entre los años 2004 y 2009. Rev Col Gastroenterol. 2010;25:344-8. [ Links ]
15. Palmer K. Acute upper gastrointestinal haemorrhage. Br Med Bull. 2007;83:307-24. [ Links ]
16. Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368:11-21. [ Links ]
17. Celinski K, Cichoz-Lach H, Madro A, et al. Non-variceal upper gastrointestinal bleeding--guidelines on management. J Physiol Pharmacol. 2008; 59(Suppl 2):215-29. [ Links ]
18. van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22:209-24. [ Links ]
19. Bor S, Dagli U, Sarer B, et al. A retrospective study demonstrating properties of nonvariceal upper gastrointestinal bleeding in Turkey. Turk J Gastroenterol. 2011;22:249-54. [ Links ]
20. de MG, Catalano F, Festini M, et al. [Esophageal non-variceal hemorrhage: a clinical and epidemiological study]. G Chir. 2002;23:199-204. [ Links ]
21. Kovacs TO, Jensen DM. The short-term medical management of non-variceal upper gastrointestinal bleeding. Drugs. 2008;68:2105-11. [ Links ]
22. Pongprasobchai S, Nimitvilai S, Chasawat J, et al. Upper gastrointestinal bleeding etiology score for predicting variceal and non-variceal bleeding. World J Gastroenterol. 2009;15:1099-104. [ Links ]
23. Crooks CJ, West J, Card TR. Upper gastrointestinal haemorrhage and deprivation: a nationwide cohort study of health inequality in hospital admissions. Gut. 2011;61:514-20. [ Links ]
24. Halland M, Young M, Fitzgerald MN, et al. Characteristics and outcomes of upper gastrointestinal hemorrhage in a tertiary referral hospital. Dig Dis Sci. 2010;55:3430-5. [ Links ]
25. Moreno P, Jaurrieta E, Aranda H, et al. Efficacy and safety of an early discharge protocol in low-risk patients with upper gastrointestinal bleeding. Am J Med. 1998;105:176-81. [ Links ]











 text in
text in