Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.4 Bogotá oct./dic. 2013
Anorectal Amelanotic Melanoma: A Case Report
Alexandra Núñez-Garbín, MD. (1), Cesia Córdova-Pantoja, MD. (1), Suzanne Patiño-Ascona, MD. (1), Juan Santillana-Callirgos, MD. (2)
(1) School of Medicine at the Universidad Peruana de Ciencias Aplicadas in Lima, Perú.
(2) Hospital Edgardo Rebagliati Martins in Lima, Perú.
Received: 24/07/13 Accepted: 27/08/13
Abstract
We present the case of a 60 year old patient suffering pain and the sensation of a foreign body in the anal region associated with traces of blood in stools. Digital rectal exam (DRE) revealed a hardened lesion located on the wall of the anal canal. Colonoscopy revealed a raised proliferating lesion with a blackish color which was about 2 inches in diameter. This was compatible with an anal canal malignancy. We proceeded to a biopsy and immunohistochemistry study which tested positive for S-100 and negative for HMB-45. A multi-slice helical chest, abdominal and pelvic CAT scan ruled out metastatic tumors and lymphadenopathy. The patient underwent local transanal excision of the partially pigmented tumor. Post- surgical histopathological results confirmed the diagnosis of malignant anal amelanotic melanoma positive for S-100. The sample tested weakly positive for Melan-A and positive for KI-67. The favorable outcome of the procedure led to the patient's discharge 3 days after surgery.
Keywords
Anal neoplasms, melanoma amelanotic, Peru.
INTRODUCTION
Anal tumors are rare neoplasms of the digestive tract. Anal cancer accounts for 4 % of all malignancies of the lower gastrointestinal tract. (1, 2) Approximately 80 % are of squamous cell origin, 10% are adenocarcinoma and the remainder consists of other types of malignant tumors such as sarcoma, lymphoma, and melanoma. (3) In this group with the lowest percentage, each type of tumor has specific characteristics: lymphoma is a lymphoid tissue tumor, sarcoma has possible mesenchymal origins, (4) and melanoma originates in the melanocytes. (5) Melanoma may or may not be pigmented and can be found in any part of the body. It is frequently located on the skin, followed by the eye and the anus. (6) Although the anus is the third location and is the most common location for gastrointestinal primary melanoma, its presentation is rare. (7)
The aim of this case report is to describe the clinical presentation, course, and treatment of malignant anal amelanotic melanoma in an older patient in a national referral hospital of the Peruvian Social Security system in Lima, Peru. In addition, this is a rare and previously unpublished condition in our environment.
CASE DESCRIPTION
The patient was a 60 year old man from Ica with no important pathological background. The patient began to suffer pain and the sensation of a foreign body in the anal region ten months prior to surgery. Two months after onset of the first symptoms, stool with bright red blood traces at the end of defecation appeared. Patient had no weight loss or alteration in bowel habits. He then consulted with a private gastroenterologist in a province of southern Peru.
Although the perianal region was found to be normal during physical examination, a rectal examination showed a hardened 2 cm in diameter lesion located in the anterior wall of the anal canal. For this reason he was referred for a colonoscopy.
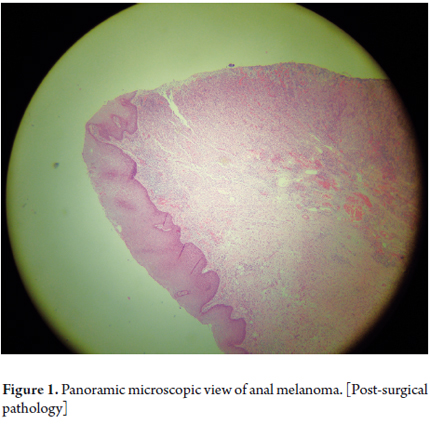
The colonoscopy performed five days later showed a blackish, highly proliferative lesion of about 2 cm in diameter which was compatible with a malignant neoplasm of the anal canal associated with prolapsed hemorrhoids next to the lesion. There were no other alterations found in the colonic mucosa. Histopathological diagnosis of a biopsy confirmed epithelial malignant anal amelanotic melanoma (Figure 1).
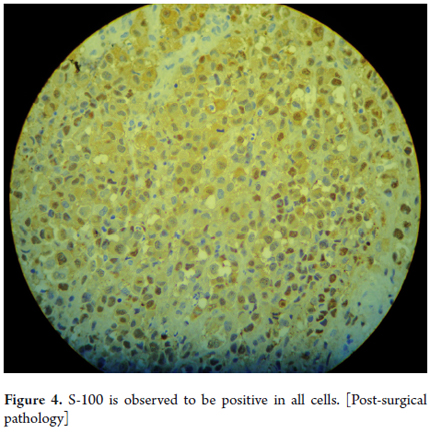
Physical examination, colonoscopy and biopsy were confirmed by another higher level facility in the city of Lima eight months after the first consultation. Further immunohistochemistry was positive for S-100 positive and negative for HMB-45 n.
Subsequently, a multicut helical thoracic abdominopelvic CT scan ruled out the presence of tumors and metastatic lymph nodes. With the diagnosis confirmed, the patient underwent a partial transanal local excision of the pigmented tumor. The lesion was located between the anal base and the dentate line and occupied 60 % of the circumference with small three millimeter in diameter satellite nodes in the surrounding mucosa. The patient's outcome was favorable, and he was discharged three days later.
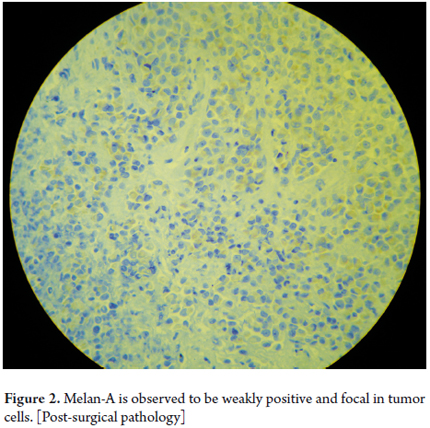
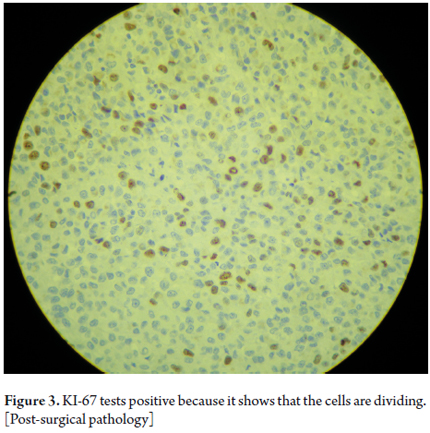
The postsurgical histopathological results were positive for S -100, weakly positive for Melan-A and positive Ki-67 and confirmed a diagnosis of malignant anal amelanotic melanoma (Figures 2, 3 and 4).
DISCUSSION
Malignant anal amelanotic melanoma is a rare entity which accounts for between 0.5 % to 2 % of all anal malignancies and less than 2% of melanomas in general. (8) It has been reported that this entity is more common in women and occurs most often from the fifth decade of life onwards. It is mainly spread via the lymphatic system and evolves rapidly with extensive local invasion. (9) The prognosis for this very aggressive cancer is bad. Despite surgery, patients have median survival time of only 20 months, and most patients die within 5 years of diagnosis. (10) Death usually occurs due to patients' advanced ages and early metastases. (11, 12). According to reported cases, the most frequent dissemination location is in the lungs (40 % of cases) followed by the central nervous system (CNS) (38% of cases) and less often to places such as the liver, bones and intestine. (6, 7, 13)
Clinically, patients present rectal bleeding or diarrhea with tenesmus. (12) The most common lesion is a nodular mass protruding through the anus. It can be pigmented or amelanotic (lacking pigment or with minimal residual pigmentation). (14) It is worth adding that, because the main symptom is rectal bleeding, many of these lesions are confused with hemorrhoid disease or external hemorrhoid thrombosis. This confusion delays diagnosis. (2) Furthermore, the differential diagnosis must consider multiple anal conditions such as anal squamous cell carcinoma, basal cell carcinoma, Bowen's disease and Paget's disease. In this case, the patient initially presented pain and the sensation of a foreign body followed later by stools with traces of blood. He was later diagnosed with malignant anal amelanotic melanoma associated with hemorrhoids.
A biopsy is necessary for diagnosis of malignant anal amelanotic melanoma. Immunohistochemistry markers highly suggestive of melanoma such as S -100 protein, HMB-45, and the expression of Melan-a are very useful for diagnosis. The S -100 protein has a high sensitivity (97% to 100 %) but a low specificity (75% to 85 %) while HMB -45 melanoma antigen is very specific and less sensitive (69% to 93 %). (13) In this patient tests for these markers were requested in order to confirm the diagnosis. The resulting positive S-100 and negative HMB-45 indicated that the lesion was amelanotic melanoma.
We also found that only 48% of patients had definitive pathological diagnoses before surgery. This indicates that the diagnosis of this disease is complex and requires the use of various tests for confirmation. (2)
The treatment of choice for this type of cancer is surgery. (5) In a study comparing the median survival time and disease-free time of local excision versus abdominal-perianal resection, similar results were obtained for the two techniques. (15) In addition, adjuvant melanoma treatment including radiation therapy and interferon can be considered (16) although it should be noted that this was not included in this patient's treatment.
One limitation of this study is that we have not been able to follow the evolution of the patient over time, so we will not know if there is a recurrence of the malignancy. Also, no brain image study was done to rule out central nervous system metastases, one of the most common locations. On the other hand, since this was a patient referred from an isolated rural area, there is no clinical history of the first health facility he went to nor any information about this patient's evolution during the months he waited for treatment in Lima.
According to the literature, in most reported cases of malignant anal amelanotic melanoma patients are in advanced stages due to metastases which implies a poor prognosis. For this reason it is important to encourage medical practitioners to perform digital rectal exams as part of clinical examinations and to perform colonoscopies to screen for colon cancer in the entire adult population over 50 years for early detection and treatment of this cancer.
Finally, from the case report and literature review we conclude that malignant anal amelanotic melanoma is a rare disease that is usually detected in later stages. However, despite the development of various forms of adjuvant therapy and improvements in surgical techniques, it continues to present poor prognoses. Therefore, it is highly important to consider this disease during differential diagnosis for early diagnosis and management.
Acknowledgments
To Dr. Domingo Morales Moon for his assistance in obtaining the histopathological slides. To Dr. Edward Mezones-Holguin for his advice during the writing of this report.
Funding
Self-financed.
Declaration of conflict of interest
The authors declare no conflicts of interest.
REFERENCES
1. Leonard D, Beddy D, Dozois EJ. Neoplasms of anal canal and perianal skin. Clin Colon Rectal Surg. 2011;24:54-63. [ Links ]
2. Bleier J. Primary anorectal amelanotic melanoma presenting as internal hemorrhoids. Gastroenterol Hepatol(N Y). 2009;5:519-20. [ Links ]
3. Back MF. Cutaneous malignant melanoma En: Baert AL, Brady LW, Heilmann HP, et al. Radiation oncology. 1st ed. Mauer, Germany: Springer; 2008, p. 515-26. [ Links ]
4. Lahat G, Lazar A, Lev D. Epidemiología y etiología de los sarcomas: posibles factores ambientales y genéticos. Surg Clin N Am. 2009;88:451-81. [ Links ]
5. Acosta AE, Fierro E, Velásquez VE, et al. Melanoma: patogénesis, clínica e histopatología. Rev Asoc Col Dermatol. 2009;17:87-108. [ Links ]
6. Singer M, Mutch MG. Anal melanoma. Clin Colon Rectal Surg. 2006;19:78-87. [ Links ]
7. Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. Cancer. 1998;83:1664-78. [ Links ]
8. Bullard KM, Tuttle TM, Rothenberger DA, et al. Surgical therapy for anorectal melanoma. J Am Coll Surg. 2003;196:206-11. [ Links ]
9. Brady MS, Kavolius JP, Quan SHQ. Anorectal melanoma. A 64-year experience at Memorial Sloan Kettering Cancer Center. Dis Colon Rectum. 1995;38:146-51. [ Links ]
10. Droesch JT, Flum DR, Mann GN. Wide local excision of abdominoperineal resection as the initial treatment for anorectal melanoma. Am J Surg. 2005;189:446-9. [ Links ]
11. Podnos YD, Tsai NC, Smith D, et al. Factors affecting survival in patients with anal melanoma. Am Surg. 2006;72:917-20. [ Links ]
12. Correia M, Amonkar D, Ramani A, et al. Anal melanoma - a case report and review of literature. Internet J Surg. 2009;19:13. [ Links ]
13. Cogir B, Whithenford M. Changing epidemiologist of anorrectal melanoma. Dis Colon Rectum. 1999;42:1203-8. [ Links ]
14. Wain EM, Stefanato CM, Barlow RJ. A clinicopathological surprise: amelanotic malignant melanoma. Clin Exp Dermatol. 2008;33:365-6. [ Links ]
15. Kiran RP, Rottoli M, Pokala N, et al. Long-term outcomes after local excision and radical surgery for anal melanoma: data from a population database. Dis Colon Rectum. 2010;53:402-8. [ Links ]
16. Hernández C, Ruiz A, Reigosa A, et al. Reunión de consenso en melanoma maligno. Rev Venez Oncol. 2005;17:56-65. [ Links ]











 texto en
texto en