Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.4 Bogotá oct./dic. 2013
Gastrointestinal Hemorrhaging Secondary to Diverticular Disease of the Jejunum: Case Report and Literature Review
John Ospina Nieto, MD., MSCC., MSCG., MSCED. (1)
(1) Gastrointestinal Surgeon and Gastrointestinal Endoscopist, Scientific Director of UNESDI, Gastroenterology and Endoscopy Unit at the Clínica Colombia and at the Centro de Enfermedades Digestivas in Bogotá, Colombia. Mail: Johnosni@yahoo.com
Received: 29-07-13 Accepted: 27-08-13
Abstract
Small bowel diverticula are rare and usually occur in the seventh decade of life. They are five to eight times more common in the ileum than in the jejunum. More than one diverticula occur together in 75 % of patients. Although they occur infrequently, they are highly relevant because of the potential lethal risks include bleeding. Until the year 2000 less than 70 cases had been described. In this paper we present the case of an 80 year old patient suffering from hypovolemic shock secondary to jejunal hemorrhaging due to diverticular disease. This required multiple transfusions and surgical management after diagnosis by enteroscopy. This article presents a brief review of the literature highlighting the importance of enteroscopy for the study and handling this type of pathology.
Keywords
Diverticulum, jejunal, enteroscopy, hemorrhaging.
INTRODUCTION
Diverticula in the small intestine are a rare entity that usually appears in the seventh decade of life. They have an incidence of 0.3% to 4.5% at autopsy and are five to eight times more common in the jejunum than in the ileum. 75% of these patients have multiple diverticula. (1-4) Complications are infrequent even though they are of great significance when they do occur because of their risks to the life of the patient. (5) Among potential complications is bleeding which had been described in less than 70 cases up described until 2000. (5, 6) In fact, a 2011 search of PubMed which used the Medical Subject Headings "intestine, small", "hemorrhage", "diverticulum" and "jejunum" as search terms, and which had no time limit, found only 47 citations. (5)
CLINICAL CASE
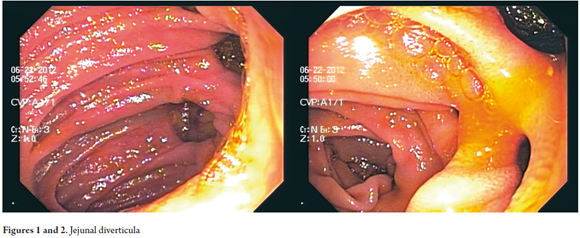
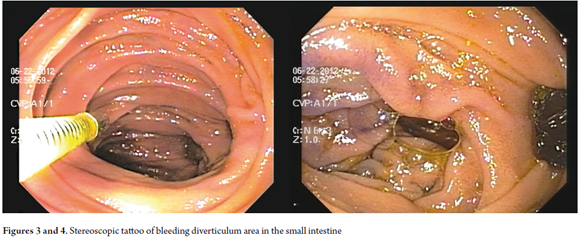
The patient was an 80-year old woman with a history of hypertension and irritable bowel syndrome who was admitted to the emergency department of the Reina Sofia Clinic in Bogotá, Colombia. The patient presented hematochezia indicating lower gastrointestinal bleeding. The patient's evaluation showed hypotension, tachycardia, hemoglobin decreased to 8 and hematocrit decreased to 28.5. The patient was stabilized hemodynamically, given a transfusion and prepared for colonoscopy and endoscopy. The endoscopy report was "antral atrophic gastritis?", and the colonoscopy report showed severe colon diverticulum disease. The colonoscopy also showed the presence of abundant fresh red blood residue although it was unable to identify a site of bleeding up to the cecum. During the second day of hospitalization the patient experienced rebleeding with hemoglobin decreased to 6, hematocrit decreased to 20, rectal bleeding and hemodynamic instability. This required another transfusion of 4 units of red blood cells. Another endoscopy and another colonoscopy were performed but could not document the bleeding area despite thorough cleaning. Nevertheless, hematic material was found in the terminal ileum. The patient was stabilized but presented another episode of rebleeding on the third day which required transfer to the ICU and multiple transfusions. Given these findings and the patient's critical condition, enteroscopy was performed (with an Olympus balloon enteroscope). This revealed the presence of numerous wide-mouthed diverticula in the proximal and medial jejunum (figures 1 and 2). One of these showed recent bleeding. The tissue was hardened and marked with an Indian ink tattoo (figures 3 and 4). The patient's case was presented to the board which decided on performance of a surgical procedure. The tattooed area, a 15cm jejunal segment, was excised through laparoscopic intestinal resection. Following the intervention the patient's recovery was good, and she was discharged from the clinic on the eight day. At present, the patient's one year follow-up and monitoring have shown no recurrences of bleeding.
DISCUSSION
Small bowel diverticula are a rare entity whose complications are even rarer. (1-5) The first reports of jejunal-ileal diverticular disease were made by Sommervit in 1794, and first reports of early complications were presented by Virchow in 1853. (6, 7) However, it was Sanpson and Gordinier who described the first patient who underwent surgery for jejunal diverticulosis in 1906. (7, 8) The prevalence of this entity at autopsy has been reported to be from 0.06 % to 4.5 % while its presence in contrasting radiological studies is reported to be from 0.5 % to 2.3 %. (1, 7-9) This condition occurs primarily in patients in their sixth and seventh decades of life. (1, 7) Jejunal diverticulosis normally presents multiple lesions which are more numerous than ileal diverticula and which are associated with diverticulosis in the esophagus (2.3% of patients), duodenum (30 %, of patients) and the colon (up to 61% of patients). (7,8 ,11-14)
Even though its etiology is unclear, there are many theories. Among them, one hypothesis that should be highlighted is the theory that the formation of diverticula occur due to dysfunction or dyskinesia of the smooth muscle of the jejunum which triggers an alteration in its contractions. (7, 15) In a study with jejunal manometry, Kongara reported that following food intake there are contractions of greater amplitude and duration than normal. This disorder can simultaneously lead to increased pressure in the intestinal lumen and predisposition to the formation of diverticula. (15, 16) Several studies have documented changes indicative of visceral myopathy and degeneration of neurons and axons of the myenteric plexus in intestinal pieces with diverticula. These findings support the theory that the diverticula are a result of a small intestinal motor dysfunction. (9, 13, 15)
Clinical manifestations are related to complications of diverticula which occur in 15% to 20 % of patients. Of these only 10% require surgical treatment. (10, 16) Among manifestations and complications we find diverticulitis and perforations in 2.3 % to 6.4 % of patients, obstructions in 2.3% to 4.6 % of cases and hemorrhaging in 3.4 % to 8.1 % of patients. Hemorrhaging may be caused by erosion and ulceration of the mucosa which compromises the mesenteric vessels around the neck of the diverticulum. This clinical bleeding can be acute rectal bleeding (as in the case reported here), melena or hematemesis, or it can be chronic such as deficiency anemia and evident or obscure occult bleeding. (7, 17, 18)
The diagnosis of bleeding from jejunal diverticulosis is difficult and is only made during surgery in many cases. In a series of 35 patients published prior to 1969, diagnosis was made intraoperatively or during autopsy. (2, 4) Nuclear medicine studies and arteriography usually do not provide the expected results although thanks to new imaging and endoscopic techniques this is now changing. Although tagged red blood cell scintigraphy may be useful for patients with intermittent lower gastrointestinal bleeding, it is considered to be very helpful when colonoscopy is not complete and when it detects the arrival of blood from the terminal ileum. (9) The study can locate the probable site of bleeding when there is more than 0.1 ml/min of active bleeding and can then be used to guide selective angiography. This requires bleeding volume that is greater than 0.5 ml/min. The extravasation site may be evident in less than one hour, or it may take as much as 24 hours to become known. (4, 5, 21) At present, double or balloon enteroscopy and capsule endoscopy are considered to be the ideal diagnostic methods for these patients. In addition, enteroscopy offers appropriate therapeutic options for controlling bleeding either by injection and/or hemoclips or as a tool to guide surgery when it is required. (14, 16, 20, 22)
REFERENCES
1. Amaya Rocha E, Milán Revollo G, Vargas B. Enfermedad diverticular del intestino delgado. RMHV. 2008;1:71-4. [ Links ]
2. Cunningham SC, Gannon CJ, Napolitano LM. Small bowel diverticulosis. Am J Surg. 2005;190:37-8. [ Links ]
3. Tarhan OR, Baryt L, Cerci C. An interesting coexistence: Small bowel volvulus and small bowel diverticulosis. Turk J Gastroenterol. 2006;17:300-4. [ Links ]
4. Chiu EJ, Shyr YM, Su CH, et al. Diverticular disease of the small bowel. Hepatogastroenterology. 2000;47:181-4. [ Links ]
5. Córdoba López A, Monterrubio Villar J, Bueno Álvarez-Arenas I, et al. Shock hemorrágico secundario a sangrado por diverticulosis yeyunal. Med. Intensiva [revista en la Internet]. 2008;32:97-8. [ Links ]
6. Zapata R, Rojas C, Gaete F. Diverticulosis yeyunal: una causa infrecuente de hemorragia digestiva. Caso clínico. Rev Med Chile. 2000;128:1133-8. [ Links ]
7. Pedraza N, Roa A. Diverticulosis del yeyuno: Complicaciones y manejo. Reporte de caso y revisión de la literatura. Rev Col Cirugía. 2010;25:48-55. [ Links ]
8. Patel V, Jefferis H, Harris S, et al. Jejunal diverticulosis is not always a silent spectator: a report of 4 cases and review of the literature. World J Gastroenterol. 2008;14:5916-9. [ Links ]
9. Steenvorde P, Schaardenburgh P, Viersma J. Enterolith ileus as a complication of jejunal diverticulosis. Dig Surg. 2003;20:57-9. [ Links ]
10. Kassahun W, Fangmann J, Harms J, et al. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007;13:2240-2 [ Links ]
11. Koger K, Clayton S. Perforated jejunal diverticula. Am Surg. 1996;62:26-30. [ Links ]
12. Crace P, Grisham A, Kerlakian G. Jejunal diverticular disease with unborn enterolith presenting as a small bowel obstruction: a case report. Am Surg. 2007;73:703-5. [ Links ]
13. El-Haddawi F, Civil I. Adquired jejuno-ileal diverticular disease: a diagnostic and management challenge. ANZ J Surg. 2003;73:584-9. [ Links ]
14. Rodríguez H, Ziauddin F, Quiros E, et al. Jejunal diverticulosis and gastrointestinal bleeding. J Clin Gastroenterol. 2001;33:412-4. [ Links ]
15. Kavita K, Edy S. Intestinal motility in small bowel diverticulosis: a case report and review of the literature. J Clin Gastroenterol. 2000;30:84-6. [ Links ]
16. Staszewicz W, Christodoulou M, Proietti S, et al. Acute ulcerative jejunal diverticulitis: case report of an uncommon entity. World J Gastroenterol. 2008;14:6265-7. [ Links ]
17. Lempinen M, Salmela K, Kemppainen E. Jejunal diverticulosis: a potentially dangerous entity. Scand J Gastroenterol. 2004;39:905-9. [ Links ]
18. Woods K, Williams E, Melvin W, et al. Acquired jejunoileal diverticulosis and its complications: a review of the literature. Am Surg. 2008;74:849-50. [ Links ]
19. Chow LW, Ong CL, Png DJ. Massive rectal bleeding from an ulceration in a jejunal diverticulum. J Clin Gastroenterol. 1993;17:85-6. [ Links ]
20. Schwesinger WH, Sirinek KR, Gaskill HV 3r.d, et al. Jejunoileal causes of overt gastrointestinal bleeding: diagnosis, management, and outcome. Am Surgeon. 2001;67:383-7. [ Links ]
21. De Markles M, Murphy J. Acute lower gastrointestinal bleeding. Med Clin N Am. 1993;77:1085-10. [ Links ]











 texto en
texto en