Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.1 Bogotá ene./mar. 2014
Survey results regarding variations in care of patients with inflammatory bowel disease
Fabián Juliao Baños MD. (1), Yineth Agudelo Zapata MD. (2), Carlos Yepes Delgado, MD. (1)
(1) Inflammatory Bowel Disease Consultation Coordinator in the Gastroenterology and Digestive Endoscopy Section of the Hospital Pablo Tobon Uribe and Professor at the University of Antioquia and Universidad Pontificia Bolivariana in Medellin, Colombia. email: fabianjuliao@hotmail.com
(2) Internal Medicine Resident at the University of Antioquia in Medellin, Colombia.
(3) Research Unit Epidemiologist at the Hospital Pablo Tobon Uribe and Professor at the University of Antioquia in Medellin, Colombia.
Received: 31-03-13 Accepted: 19-12-13
Abstract
Objectives: The quality of care of our patients with inflammatory bowel disease (IBD) is the principal mechanism through which we can offer an appropriate level of health care for our population. Therefore, it is important to determine variations in care provided for patients by specialists with expertise in the management of IBD in Colombia.
Methods: This is a descriptive statistical analysis of responses to a survey with 13 questions related to quality of care provided to patients with IBD. The survey was conducted in 2011 among specialists who are interested in the management of patients with IBD.
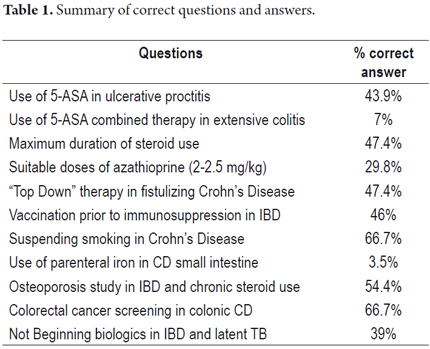
Results: Fifty seven gastroenterologists and coloproctologists answered all 13 questionnaire questions. Among the most interesting results is the fact that 44 % of the respondents use topical 5-ASA drugs as monotherapy for treatment of mild ulcerative proctitis. 30% use correct doses of azathioprine (2.0 to 2.5 mg /kg). Only 47 % of these specialists prefer to start with top down biological therapy in patients with fistulizing Crohn's disease (CD). Fifty four percent vaccinate their patients with IBD prior to the start of immunosuppressive therapy. Sixty seven percent think that patients with CD should suspend smoking, but 21% do not give patients any recommendation about smoking. Only 54 % of respondents screen for osteoporosis in individuals with IBD and chronic steroid use. Finally, 67% screen for colorectal cancer in patients with CD which is similar to the recommendations for ulcerative colitis (UC).
Conclusion: Treatment and preventive care for patients with IBD varies greatly within our environment, this represents a great opportunity for continuous improvement in our daily practice. Greater adherence to guidelines and recommendations for proper management of our patients with IBD is required.
Keywords
Inflammatory bowel disease, Crohn's disease, ulcerative colitis, quality of care.
INTRODUCTION
Inflammatory bowel disease (IBD) includes two entities, Crohn's disease (CD) and ulcerative colitis (UC). These are chronic and idiopathic inflammatory bowel diseases that significantly affect the quality of life of those who suffer from them. Moreover, they and are costly to the health care system (1). Numerous published guidelines based on clinical evidence provide recommendations for diagnosis and treatment of IBD and its complications (2-7). The recently published Colombian Inflammatory Bowel Disease consensus provides multiple IBD management recommendations adapted to our environment (31). Despite this, care of IBD patients varies greatly in terms of diagnosis, treatment, preventive care and recommendations for colorectal cancer monitoring (8-10). We see in physicians' daily practice over-use, under-use and poor use of the medical resources that we have at our disposal. The quality of care of our patients with IBD, based on accepted international standards, is the main mechanism through which we can offer an appropriate level of health care to our population. Recognizing variation in IBD management is the first step toward improving the quality of medical care for our patients with IBD (11). Given this we designed a survey to determine the variation in the care of patients with IBD in Colombia by specialists with expertise in the management of this entity.
MATERIALS AND METHODS
A descriptive study was conducted with the answer to a survey conducted during 2011 to clinical gastroenterologists, coloproctologists and surgeon endoscopists in the cities of Bogota, Cali, Medellin and Barranquilla with an interest in the management of patients with IBD. This survey was conducted for specialists attending IBD update conferences in the listed cities. In total 57 experts answered the complete and a statistical analysis of their answers was performed.
For the IBD quality survey 13 questions were selected (Appendix 1) based on the recommendations of international scientific associations such as the AGA (American Gastroenterology Association) and the CCFA (Crohn's & Colitis Foundation of America) on quality of care of IBD patients. In addition, questions suggested by the authors of this study were included taking into account the recommendations of a previous publication (11). Regarding the result of the survey the analysis divided the questions in: quality treatment topics, knowledge of preventive care and a question of appropriate colorectal cancer monitoring in CD.
A descriptive statistical analysis was performed, the percentages of each of the survey items were obtained, and the results were analyzed using SPSS statistical software.
RESULTS
A total of 57 experts answered the IBD quality survey. Sixty-three % are clinical gastroenterologists, 21% are coloproctologists and 16 % are surgical endoscopists. The largest number of respondents work in Bogotá (39%), and the rest practice in Cali (25%), Barranquilla (23%) and Medellín (14%).
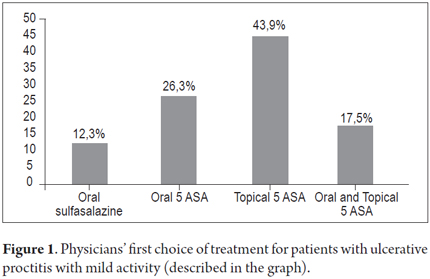
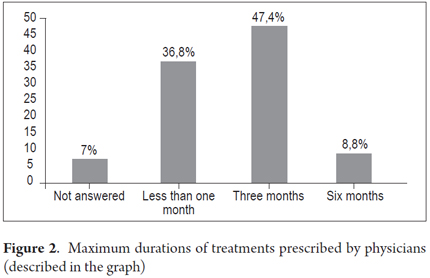
Responses to survey questions about quality recommendations regarding treatment showed that 44% of respondents used topical 5-ASA drugs as monotherapy for treatment of mild ulcerative proctitis. It is noteworthy that 30% of the respondents never use topical 5-ASA therapy for these patients (Figure 1). Similarly, only 7% of respondents use topical therapy with 5- ASA when patients do not respond to oral 5-ASA treatment for extensive colitis. The majority (63 %) prefer to use oral steroids. In addition, while 49 % of the specialists replied that the maximum exposure time to a cycle of oral steroids should be 3 months, 9% of them continue to use them for up to 6 months (Figure 2).
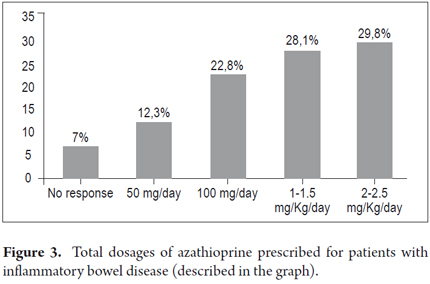
Thirty-seven percent of respondents started administration of immunosuppressants after two cycles of steroids, 30% wait for 3 cycles and 10 % start azathioprine after 3 cycles. Thirty percent of respondents use the correct dose of azathioprine (2.0-2.5 mg/kg) while 28 % of them use subtherapeutic doses of 1-1.5 mg/kg. It is noteworthy that 35 % use standard doses of 50 or 100 mg/day regardless of the weight of the patient (Figure 3). In addition, only 47 % of specialists consider top down biological therapy for patients with fistulizing CD.
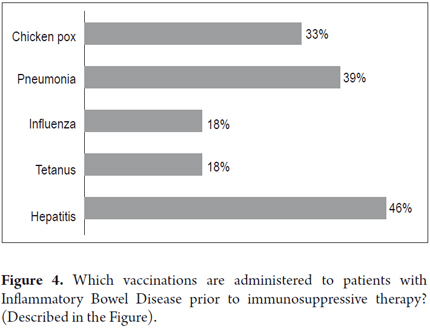
Responses to questions related to preventive care for IBD showed that 54% vaccinated their IBD patients prior to the start of immunosuppressant therapy. Forty-six percent vaccinated against hepatitis B, 39% against streptococcus pneumoniae, 33 % against varicella and only 18 % against influenza and tetanus (Figure 4).
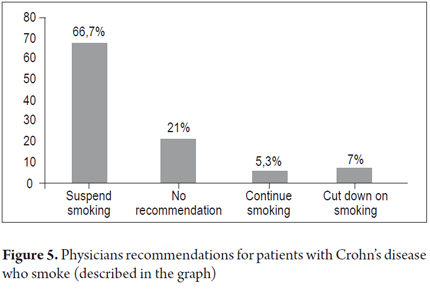
Sixty-seven percent recommended that their patients with Celiac Disease stop smoking while 21% do not make any recommendations to their patients about smoking (Figure 5). Only 3.5 % use parenteral iron to manage severe iron deficiency anemia in patients with Celiac Disease whose small intestines are extensively compromised, but 67 % prefer to administer iron orally. Only 54 % of respondents screen for osteoporosis in individuals with IBD who chronically use steroids.
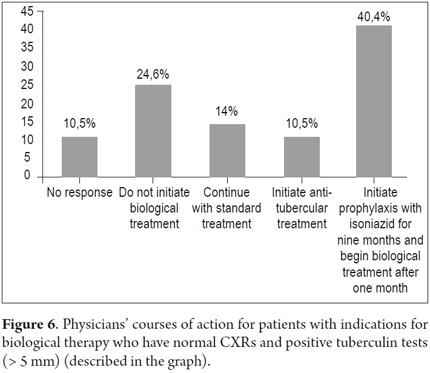
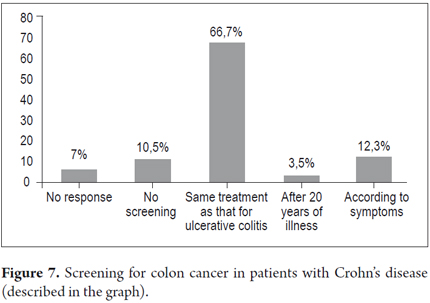
Thirty-nine percent of respondents prefer to start and continue standard therapy for patients with indications for biological therapy who have normal chest x-rays and more than 5 mm on the tuberculosis skin test while 40% perform isoniazid chemoprophylaxis and start biological therapy (Figure 6). Finally, sixty-seven percent screened celiac disease patients for colorectal cancer in a manner similar to recommendations for screening of ulcerative colitis patients (Figure 7). A summary of the correct questions and answers is presented in Table 1.
DISCUSSION
This study shows great variation in the care of IBD provided by medical specialists in gastroenterology and coloproctology in the different cities of Colombia. This problem is local since it also occurs in other countries. In Boston, MA USA, a study of 64 patients examined in follow-up appointments assessed adherence to established guidelines and found that 75% of patients with distal ulcerative colitis were not receiving topical 5-ASA. In our study this figure was 56 %. In addition, 82% of the Boston patients using azathioprine received subtherapeutic doses. This figure was 70 % in our survey (8). Similarly, a retrospective study in China found that only 54% of patients with distal colitis received topical 5-ASA and only 19.6% of patients with indications for treatment with thiopurines were receiving them. Of these 57 % received suboptimal doses (12). The well-established dosage of azathioprine required for maintaining clinical remission in CD is 2.5 mg/kg/day. A Cochrane review found that the OR of effectiveness at this dose is 4.1, while it is 3.0 for doses of 2.0 mg/kg/day, and 1.2 for doses of 1.0 mg/kg/day (16).
Recent international and national guidelines indicate that the first-line treatment for patients with ulcerative proctitis is topical 5-ASA therapy, preferably suppository enemas (3, 31). In addition, a recent meta-analysis of four studies (14) demonstrated that the combination of oral 5-ASA plus topical 5-ASA drugs is more effective for inducing remission in mildly and moderately active ulcerative colitis than oral 5-ASA alone (RR 0.65, NNT 5). In our study 63 % of respondents prefer to add topical steroids before 5-ASA for these patients.
A survey about CD management that was answered by 186 gastroenterologists who are members of the American Gastroenterological Association (AGA) found a high rate of prescription of 5-ASA drugs especially among physicians who are not experts in IBD management (75 % vs 44 %, P: 0.002). This practice continues to be common despite the fact that there is little clinical evidence supporting its use (13).
On the other hand, since steroids should not be used continuously for more than 16 weeks, patients who require more than 2 courses of treatment with steroids per year and patients who are steroid dependent require steroid-sparing treatment such as immunosuppressants or biological therapy (15). In this regard, 41 % of respondents expect patients will have more than 2 cycles of steroids before they start immunosuppressants.
A study in Los Angeles, CA USA found that only 45 % of IBD patients had received tetanus booster vaccinations in the prior 10 years, 28 % received annual vaccinations against influenza, 9% received annual vaccinations against streptococcus pneumoniae, and only 33 % of at risk patients had hepatitis B immunizations (17). In our study, 46% of responding specialists contemplated vaccinating IBD patients prior to the use of immunosuppressant therapy. A more recent Canadian study found that only 14.3 % of the gastroenterologists surveyed determine IBD patients' immunization histories while 23.1 % of them did not know that live attenuated vaccines should be avoided in immunosuppressed patients and 18.6 % did not know which type of vaccine should be applied before the start of immunosuppressant therapy (18). These practices are common despite the availability of published guides on immunization of IBD patients (19, 20).
Smoking is a risk factor for Crohn's Disease that has been associated with higher rates of relapse and hospitalization and greater needs for immunosuppressants and surgery compared to non-smokers. A prospective French study of 59 patients showed that those who quit smoking decreased the rate of relapse within the first year of follow-up by 65 % over individuals with CD who continued to smoke (21). In our study, 67 % of specialists recommended that their CD patients stop smoking.
To treat IBD patients who also anemia, the simplest method is oral iron therapy. An oral dose of 100 mg/day of elemental iron is sufficient considering that only 10 mg/day are absorbed. However, this is not recommended for patients with Crohn's disease. Because of small intestine compromise, local Fenton reactions can produce free radicals that can lead to increased inflammation. Consequently, the preferred method is parenteral administration of iron for more rapid and prolonged responses which improve patient quality of life better than oral iron can (22-24). In our survey, 67% prefer to start oral iron and only 3.5 % preferred parenteral iron as first line therapy for CD patients with extensive small intestine compromises.
After 6 months of corticosteroid treatment at doses of more than 7.5 mg/day there is a 50 % risk of osteoporosis and a 50 % risk of fractures. It is recommended that patients who have had previous fractures, patients who have first-degree relatives with osteoporosis, patients who have used steroids previously (prednisone doses of more than 7.5 mg/day for more than 3 months), postmenopausal women, men who are over 50 years old, and those with body mass indices below normal should undergo bone densitometry to rule out osteoporosis. This should be repeated every 2 to 3 years (25-26). In this study, 54% of respondents performed bone densitometry on IBD patients with chronic steroid use.
Patients with latent tuberculosis (positive tuberculosis test with greater than 5mm induration or an abnormal chest x-ray) should be treated with 300 mg/day of isoniazid for 9 months beginning at least one month before the start of the first application of anti-TNF. This has been shown to reduce tuberculosis by 70 %. In case active tuberculosis develops, anti-TNF should be discontinued immediately (27). It is striking that 39 % of respondents do not start anti-TNF therapy and do not use isoniazid chemoprevention for latent tuberculosis.
CD patients with colonic compromises of at least one third the length of the colon require colonoscopies to screen for colorectal cancer 8 to 10 years after onset of CD and preferably when the disease is in remission. Patients who test negative for neoplasia require follow-ups every 1 or 2 years. From the twentieth year after onset an annual colonoscopy is recommended (28-30). 67 % of our respondents screen for colorectal cancer in patients who have had colonic CD for 8 years or more.
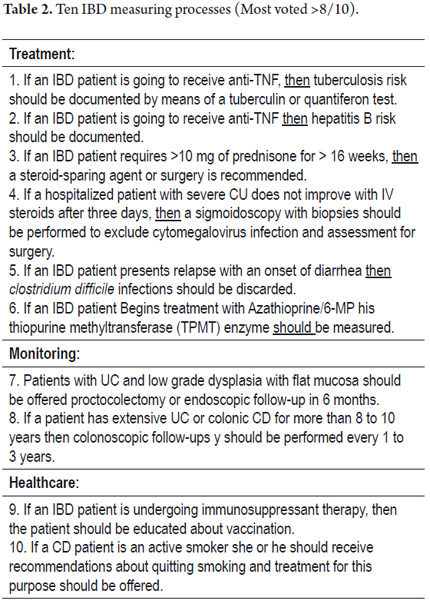
A recent publication (32) suggests the application of 10 measurable processes as quality indicators for IBD. Based on a consensus of experts, the ten indicators were chosen from more than 500 potential processes. These indicators should be applied in our daily clinical practice for the care and benefit of our IBD patients. A summary of these processes is presented in Table 2.
In conclusion, there is great variability in treatment and preventive care of IBD patients in our environment. This represents a great opportunity for continuous improvement of our daily practice. What is needed is greater adherence to international and national guidelines for the proper management of IBD patients combined with persistence in organizing and attending continuing medical education events for IBD backed by scientific associations.
Acknowledgments
We would like to thank all of our colleagues who answered the survey. Their responses provided us the feedback necessary to help of our IBD patients. Thanks to my wife Lina and to my daughters Paulina and Susana for their time.
APPENDIX 1
Quality of IBD Patient Care in Colombia Survey
Date: _____________________.
City: _____________________.
Mark with an X:
Clinical Gastroenterologist: __. Endoscopic Surgeon: __.
Coloproctologist: __. Other: ___________________.
* Quality recommendations regarding treatment:
1. In patients with ulcerative proctitis with mild activity, your first choice of treatment is:
a) Oral Sulfasalazine.
b) Oral 5-ASA oral.
c) Topical 5-ASA.
d) Oral 5-ASA plus topical 5-ASA.
2. In patients with mild ulcerative colitis who are unresponsive to oral 5-ASA, your behavior is:
a) Add azathioprine.
b) Add steroids.
c) Add biologics.
d) Add topical 5- ASA.
3. When you start steroids in patients, the maximum duration of treatment that you use is:
a) < 1 month.
b) 3 months.
c) 6 months.
d) > 1 year.
4. In patients with inflammatory bowel disease requiring repetition of steroids, after how many cycles do you use immunosuppressants (azathioprine):
a) 1 cycle.
b) 2 cycles.
c) 3 cycles.
d) > 3 cycles.
5. The total dose of azathioprine that you use for patients with inflammatory bowel disease is:
a) 50 mg/day.
b) 100 mg/day.
c) 1-1.5 mg/Kg/day.
d) 2-2.5 mg/Kg/day.
6. Would you begin top down entry biological therapy in patients with fistulizing Crohn's disease?
Yes _________ No ______________
* Preventive care recommendation topics:
7. At present, are you applying any type of vaccine to patients with inflammatory bowel disease prior to immunosuppressant therapy?
Yes _________ No ______________
8. What type of vaccine are you applying to patients with inflammatory bowel disease prior to immunosuppressant therapy?
Hepatitis B: Yes: ____ No: _____
Tetanus: Yes: ____ No: _____
Influenza: Yes: ____ No: _____
Pneumococcus: Yes: ____ No: _____
Varicella: Yes: ____ No: _____
9. Regarding smoking in Crohn's disease, your recommendation to a patient is:
a) Suspend it.
b) Do not give any recommendation.
c) Continue as usual.
d) Lower its quantity.
10. In patients with severe anemia (Hb <10 g / dl) by of extensive small intestine Crohn's disease, your behavior is:
a) Observe it.
b) Begin oral iron.
c) Begin parenteral iron.
d) Begin erythropoietin.
11. Do you perform an osteoporosis study in patients with inflammatory bowel disease with chronic steroid use?
Yes: _______________ No: _____________
12. In a patient with indication for biological therapy with normal CXR and POSITIVE tuberculin test (>5) your behavior is:
a) Do not Begin biologics.
b) Continue with standard therapy.
c) Begin anti-tuberculosis treatment.
d) Begin prophylaxis with 300 mg isoniazid for 9 months and after one month begin biological therapy.
* Appropriate colorectal cancer monitoring:
13. Regarding colon cancer screening in patients with CD and colonic compromise your behavior is:
a) Never perform it because the risk is the same as for general population.
b) Perform it in the same way as in ulcerative colitis.
c) Start it after 20 years of the disease.
d) Start it according to the patient's symptoms.
REFERENCES
1. Kappelman MD, Rifas-Shiman SL, Porter CQ, Ollendorf DA, Sandler RS, Galanko JA, et al. Direct health care costs of Crohn's disease and ulcerative colitis in US children and adults. Gastroenterology. 2008;135(6):1907-13. [ Links ]
2. Kornbluth A, Sachar DB, Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105(3):501-523; quiz 524. [ Links ]
3. Dignass A, Lindsay JO, Sturm A, Windsor A, Colombel J-F, Allez M, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. J Crohns Colitis. 2012;6(10):991-1030. [ Links ]
4. Lichtenstein GR, Hanauer SB, Sandborn WJ, Practice Parameters Committee of American College of Gastroenterology. Management of Crohn's disease in adults. Am J Gastroenterol. 2009;104(2):465-483; quiz 464, 484. [ Links ]
5. Dignass A, Van Assche G, Lindsay JO, Lémann M, Söderholm J, Colombel JF, et al. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: Current management. J Crohns Colitis. 2010;4(1):28-62. [ Links ]
6. Mowat C, Cole A, Windsor A, Ahmad T, Arnott I, Driscoll R, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011;60(5):571-607. [ Links ]
7. Rahier JF, Ben-Horin S, Chowers Y, Conlon C, De Munter P, D'Haens G, et al. European evidence-based Consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2009;3(2):47-91. [ Links ]
8. Reddy SI, Friedman S, Telford JJ, Strate L, Ookubo R, Banks PA. Are patients with inflammatory bowel disease receiving optimal care? Am J Gastroenterol. 2005;100(6):1357-61. [ Links ]
9. Esrailian E, Spiegel BMR, Targownik LE, Dubinsky MC, Targan SR, Gralnek IM. Differences in the management of Crohn's disease among experts and community providers, based on a national survey of sample case vignettes. Aliment Pharmacol Ther. 2007;26(7):1005-18. [ Links ]
10. Spiegel BMR, Ho W, Esrailian E, Targan S, Higgins PDR, Siegel CA, et al. Controversies in ulcerative colitis: a survey comparing decision making of experts versus community gastroenterologists. Clin Gastroenterol Hepatol. 2009;7(2):168-174, 174.e1. [ Links ]
11. Juliao F. Calidad en el manejo de enfermedad inflamatoria intestinal. Rev Col Gastroenterol. 2011;26:211-20. [ Links ]
12. Zhu Q, Cao Q, Si J-M. Quality of care for patients with inflammatory bowel disease in East China. World J Gastroenterol. 2008;14(4):612-6. [ Links ]
13. Esrailian E, Spiegel BMR, Targownik LE, Dubinsky MC, Targan SR, Gralnek IM. Differences in the management of Crohn's disease among experts and community providers, based on a national survey of sample case vignettes. Aliment Pharmacol Ther. 2007;26(7):1005-18. [ Links ]
14. Ford AC, Khan KJ, Achkar J-P, Moayyedi P. Efficacy of oral vs. topical, or combined oral and topical 5-aminosalicylates, in Ulcerative Colitis: systematic review and meta-analysis. Am J Gastroenterol. 2012;107(2):167-176; author reply 177. [ Links ]
15. Panaccione R, Rutgeerts P, Sandborn WJ, Feagan B, Schreiber S, Ghosh S. Review article: treatment algorithms to maximize remission and minimize corticosteroid dependence in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2008;28(6):674-88. [ Links ]
16. Prefontaine E, Sutherland LR, Macdonald JK, Cepoiu M. Azathioprine or 6-mercaptopurine for maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 2009;(1):CD000067. [ Links ]
17. Melmed GY, Ippoliti AF, Papadakis KA, Tran TT, Birt JL, Lee SK, et al. Patients with inflammatory bowel disease are at risk for vaccine-preventable illnesses. Am J Gastroenterol. 2006;101(8):1834-40. [ Links ]
18. Yeung JH, Goodman KJ, Fedorak RN. Inadequate knowledge of immunization guidelines: a missed opportunity for preventing infection in immunocompromised IBD patients. Inflamm Bowel Dis. 2012;18(1):34-40. [ Links ]
19. Sands BE, Cuffari C, Katz J, Kugathasan S, Onken J, Vitek C, et al. Guidelines for immunizations in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2004;10(5):677-92. [ Links ]
20. Melmed GY. Vaccination strategies for patients with inflammatory bowel disease on immunomodulators and biologics. Inflamm Bowel Dis. 2009;15(9):1410-6. [ Links ]
21. Cosnes J, Beaugerie L, Carbonnel F, Gendre JP. Smoking cessation and the course of Crohn's disease: an intervention study. Gastroenterology. 2001;120(5):1093-9. [ Links ]
22. Gasche C, Lomer MCE, Cavill I, Weiss G. Iron, anaemia, and inflammatory bowel diseases. Gut. 2004;53(8):1190-7. [ Links ]
23. Gasche C, Berstad A, Befrits R, Beglinger C, Dignass A, Erichsen K, et al. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm Bowel Dis. 2007;13(12):1545-53. [ Links ]
24. Lee TW, Kolber MR, Fedorak RN, van Zanten SV. Iron replacement therapy in inflammatory bowel disease patients with iron deficiency anemia: a systematic review and meta-analysis. J Crohns Colitis. 2012;6(3):267-75. [ Links ]
25. Lichtenstein GR, Sands BE, Pazianas M. Prevention and treatment of osteoporosis in inflammatory bowel disease. Inflamm Bowel Dis. 2006;12(8):797-813. [ Links ]
26. Bernstein CN, Leslie WD, Leboff MS. AGA technical review on osteoporosis in gastrointestinal diseases. Gastroenterology. 2003;124(3):795-841. [ Links ]
27. Papa A, Mocci G, Bonizzi M, Felice C, Andrisani G, De Vitis I, et al. Use of infliximab in particular clinical settings: management based on current evidence. Am J Gastroenterol. 2009;104(6):1575-86. [ Links ]
28. Itzkowitz SH, Present DH, Crohn's and Colitis Foundation of America Colon Cancer in IBD Study Group. Consensus conference: Colorectal cancer screening and surveillance in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11(3):314-21. [ Links ]
29. Farraye FA, Odze RD, Eaden J, Itzkowitz SH. AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138(2):746-774, 774.e1-4; quiz e12-13. [ Links ]
30. Cairns SR, Scholefield JH, Steele RJ, Dunlop MG, Thomas HJW, Evans GD, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010;59(5):666-89. [ Links ]
31. Hani AC, Galiano MT, Albis R, Marquez JR, Juliao F, et al. Consenso Colombiano de Enfermedad Inflamatória Intestinal. Rev Col Gastroenterol 2012;27:S1-S44. [ Links ]
32. Melmed GY, Siegel CA, Spiegel BM, Allen JI, Cima R, Colombel J-F, et al. Quality indicators for inflammatory bowel disease: development of process and outcome measures. Inflamm Bowel Dis. 2013;19(3):662-8. [ Links ]











 texto en
texto en