Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.1 Bogotá ene./mar. 2014
Cytomegalovirus pancreatitis in immunocompromised patients: A case report
Lourdes Salazar Huayna MD. (1), Eduardo Vélez Segovia MD. (1), José Ruelas Figueroa MD. (2), Fernando Mendo-Urbina MD. (2), Marco Montiel Gonzales MD. (2)
(1) School of Medicine and Scientific Society of Medical Students at the Universidad Peruana de Ciencias Aplicadas (UPC) in Lima, Perú.
(2) Edgardo Rebagliati Martins National Hospital EsSalud, Infectious Diseases Department in Lima, Perú
Study Location
Edgardo Rebagliati Martins National Hospital in Lima, Perú
Received: 20-05-13 Accepted: 19-12-13
Abstract
We report two cases of pancreatitis secondary to cytomegalovirus infections which were tested by reverse transcription polymerase chain reaction (RT-PCR) in patients with human immunodeficiency virus (HIV). Other causes were ruled out by laboratory findings. Both patients were treated with ganciclovir and improved clinically and as indicated by laboratory findings. This condition should not be ignored in HIV-positive patients in spite of the absence of the clinical characteristics of acute pancreatitis.
Key words
Pancreatitis, cytomegalovirus, immunodeficiency (source DeCs BIREME).
INTRODUCTION
Acute pancreatitis is a common digestive disease whose morbidity and mortality depends directly on its time of evolution. Consequently, early diagnosis is a necessity. The disease is clinically characterized by acute upper abdominal pain which radiates to the flanks and which is associated with nausea and vomiting in most cases. Although biliary lithiasis and excessive alcohol intake are the most common causes, there are other causes such as drug use, surgery and infections.
Gastrointestinal disorders are common in immunocompromised people and require prompt recognition (3, 4). If not diagnosed in time, pancreatitis can be more severe in these patients than in immunocompetent patients (5). Antiretroviral drugs, particularly protease-inhibitors, have been described among the etiologies of pancreatitis for this particular group. Pancreatitis may be either directly related to the use of these drugs or to complications secondary to their use such as hypertriglyceridemia. Opportunistic infections are also another major cause (6). Below we present two cases of acute pancreatitis due to cytomegalovirus (CMV) in immunocompromised persons.
CASE 1
A 21 year old male patient who had been born and raised in Lima entered the emergency department because of liquid stools, six to seven bowel movements per day over the previous four weeks, associated nonspecific abdominal cramps, subjective unquantified increased body temperature, weight loss of 6 kg, nausea and chills for the previous week. The patient had tested positive for Human Immunodeficiency Virus (HIV) but was not receiving Highly Active Antiretroviral Therapy (HAART). According to the patient, he had had syphilis and gonorrhea five years before but had not had tuberculosis or contact with patients with infectious tuberculosis, had not had hepatitis, and did not consume alcohol or other psychoactive drugs.
Upon physical examination his heart rate was 65 bpm, his respiratory rate was 15 bpm and his blood pressure was 90/70 mmHg. In the oral cavity the mucosa of the oropharynx was mildly congested and there was glossitis and white desquamative lesions on the edges of his tongue. Neither visceromegaly nor adenopathies were detected. The abdomen was soft, depressible and mobile with respiratory movements. Bowel sounds were augmented. There was epigastric and hypogastric tenderness. Digital rectal examination revealed a hypotonic sphincter with a delimited anal margin and circular papules that were not painful.
Laboratory test results were as follows: Hemoglobin - 10.50 g/dL; hematocrit - 31%; average corpuscular volume - 76.32 fL; average corpuscular hemoglobin - 25.62 pg; platelet count 33,7400/mm3; white blood cell count 6,500 cells/mm3 with 2% bands; electrolytes - within normal range; HIV viral load - 64,833 copies/ml, and rapid plasma reagin (RPR) - negative.
The blood test for Human T-Lymphotropic Virus (HTLV-1) was negative, as were tests for Hepatitis B and C. The presence of tuberculosis or parasites was ruled out. The CD4 count was 22 cells/uL.
Abdominal ultrasound found an enlarged pancreas. High amylase and lipase enzymes levels were reported, 799 U/L and 1025 U/L respectively. Liver biochemical and function tests showed total bilirubin at 0.27 mg/dL, aspartate aminotransferase (AST) at 37 U/L, alanine aminotransferase (ALT) at 22 U/L and alkaline phosphatase at 145 U/L.
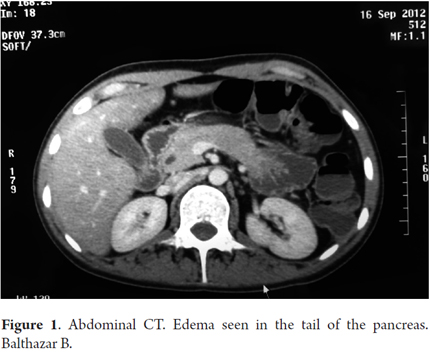
A thoracoabdominal-pelvic CT scan also showed an enlarged pancreas plus a dilated Wirsung's duct (see Figure 1). In accordance with the clinical and radiological evidence the patient was diagnosed with acute pancreatitis. Magnetic resonance cholangiopancreatography (MRCP) confirmed the previous findings. Additional tests had the following results. A toxoplasma and a cytomegalovirus blood test were both negative for IgM while the toxoplasma test was also negative for IgG, but the cytomegalovirus test was positive for IgG. A herpes 1 blood test was negative for IgM, but positive for IgG. A herpes 2 blood test was negative for both IgM and IgG. To evaluate the presence of cytomegalovirus, a real-time polymerase chain reaction (RT-PCR) was also requested. It detected 2887 copies/mL. Administration of ganciclovir was initiated immediately and continued for 12 days leading to a remarkable clinical recovery.
CASE 2
This patient is a 41-year-old female patient from Lima, Peru who has a history of kidney stones, severe depression and psoriasis vulgaris managed with occasional use of topical steroids. She came to the emergency department because she had been suffering shortness of breath with medium exertion and had lost 8 kilograms of weight loss during the previous month. These symptoms were associated with the perception of sporadic body temperature increases. She had no history of arterial hypertension, diabetes mellitus, tuberculosis or sexually transmitted diseases. At the moment of admission to the emergency department her heart rate was 90 bpm, her respiratory rate was 18 bpm and her blood pressure was 130/90mmHg. Physical examination showed notable presence of erythematous and desquamative areas on her face and scalp and also some easily removable white plaques on the surface of her tongue.
Laboratory tests showed hemoglobin at 12.94 g/dL, a white blood cell count of 2,930 cells/mm3, and a platelet count of 73,000/mm3. The patient was hospitalized. During her first week of hospitalization a urine culture showed a urinary tract infection due to Escherichia coli. The infection was treated with ceftriaxone for 10 days. An ELISA test was positive for HIV. The possibility of tuberculosis was explored, but urine, sputum and stool cultures were all negative. In addition, the presence of parasites in stools was ruled out.
During her second week of hospitalization, the patient presented liquid stools with four or five 5 bowel movements per day and sporadic low volume vomiting. Additional tests showed sodium at 143 mmol/L, potassium at 1.25mmol/L and chloride at 114.2 mmol/L. The patient's clinical response was negative despite management of the electrolyte deficit. She presented muscular weakness, hyporeflexia and respiratory arrest associated with severe hypokalemia. The patient was referred to the Intensive Care Unit, where she had a favorable recovery after a few days of fluids and electrolyte replacement. On her 20th day of hospitalization she was referred to the Department of Infectious Disease after presenting abdominal pain (predominantly epigastric pain), nausea and vomiting. Abdominal ultrasound showed only moderate hepatic steatosis. Additional tests showed her amylase at 701 U/L, lipase at 571 U/L, bilirubin at 0.31 mg/dL, AST at 193 U/L, ALT at 96 U/L, and alkaline phosphatase at 169 U/L. Her CD4 count was 9 cells/uL.
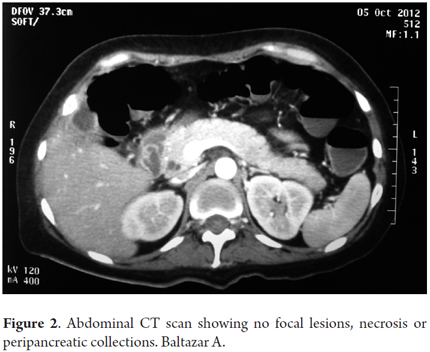
A CAT scan showed no dilation of the biliary tract or pancreatic duct (See Figure 2). Hepatitis B and C blood tests were negative. Upper gastrointestinal endoscopy showed erythematous gastritis and prominent folds in the mucosa of the fundus. Blood tests for Salmonella Typhi and Salmonella Paratyphi antigens and Brucella antigens were non-reactive. Other blood tests showed were negative for cytomegalovirus IgM, positive for cytomegalovirus IgG, negative for toxoplasma IgM and IgG, and negative for both herpes 1 and herpes 2 IgM and IgG. The RPR test was non-reactive.
An additional test showed a CMV viral load of 424 copies/ml. Ten days later a followup test showed 27,126 copies/ml. In accordance with these results, the possibility of a CMV infection associated with the pancreatitis was proposed. Treatment with Ganciclovir was initiated, and clinical recovery was observed in the following days. It is important to point out that HAART was never administered to this patient in the inpatient setting.
DISCUSSION
It is known that cytomegalovirus is able to infect multiple organs and cause various diseases in immunocompromised patients. The most common are ocular, pulmonary, central nervous system and gastrointestinal tract infections. Colitis, esophagitis, gastritis and hepatitis have been described as the most prevalent gastrointestinal tract infections (7).
In the last years, cytomegalovirus has been reported as an etiologic agent for acute pancreatitis. The first report, published more than 20 years ago, describes two probable cases of cytomegalovirus pancreatitis in HIV seropositive patients. Both cases showed an unfavorable response to treatment and the patients died as the result of secondary respiratory insufficiency. Neither of these patients presented clinical characteristics of pancreatitis. Both had high CMV titers, and high amylase and lipase levels. One of them underwent a pancreatic biopsy which revealed the acinar necrosis, inflammation and cytological changes, characteristic of cytomegalovirus (8).
The second report, more than 15 years ago, described the case of a female patient with pancreatitis and markedly elevated amylase and lipase. This patient also presented mild pleural effusions which caused dyspnea. She received support treatment and 5-Fluorouracil. She responded satisfactorily to treatment and fully recovered after approximately two weeks of hospitalization (9).
Cytomegalovirus pancreatitis has also been described patients who present another immunological disorders other than HIV. The most common groups are patients with systemic lupus erythematosus, post kidney transplant patients, and patients who receive corticosteroids or immunosuppressive treatment (10-12).
The two patients described in this report presented markedly elevated levels of amylase and lipase and high CMV viral load titers obtained through RT-PCR. The first case began with a gastrointestinal disorder which was compatible with acute pancreatitis. Even though the clinical picture was not representative of pancreatitis, it was within the clinical spectrum of this pathology. The second case was hospitalized for a longer period of time. She initially presented a urinary tract infection and a severe hydroelectrolytic disorder (hypokalemia). During recovery gastrointestinal symptoms compatible with acute pancreatitis began.
The most common causes of pancreatitis were ruled out in both patients. It is important to note that neither of these patients consumed alcohol on their regular basis and that neither ultrasound nor CAT scans showed alterations in the biliary tract. Although the second case presented high transaminase levels, these enzymes may be elevated due to concomitant hepatic inflammation, due to release from some other tissue, or due to the evolution of acute pancreatitis (8).
Since both patients were HIV seropositive, there were other etiological possibilities for the development of pancreatitis including infectious agents or other undiagnosed disorders. For this reason the pursuit of other etiologies of high prevalence in this population was initiated. Neither patient had been treated with HAART, so serology tests for the most common opportunistic infections were requested. Elevated CMV viral loads were detected, treatment with Ganciclovir was initiated in both cases, and appropriate treatment responses were obtained as evidenced by clinical and supplementary tests.
The gold standard for diagnosing cytomegalovirus infection is direct viral culture in human fibroblasts. However, the practical usefulness of this procedure is limited by its low specificity, duration, and loss of viability in stored samples (12). There are other tests including RT-PCR which is based on the detection of CMV deoxyribonucleic acid (DNA) through amplification of copies of the genetic material. This is not only beneficial because it is a quick process which takes only sixteen to forty-eight hours but also because it requires a smaller amount of volume blood samples and offers a sensitivity of 91% and a specificity of 92.1% (13). RT-PCR was used to diagnose CMV in both cases. In addition, the b therapeutic response obtained after the use of Ganciclovir in both cases strengthens cytomegalovirus as the presumptive etiological agent of pancreatitis.
CONCLUSION
Two cases of CMV pancreatitis with dissimilar clinical characteristics, but both with markedly elevated amylase and lipase levels, high CMV serum titers, subjective body temperature increases and respiratory compromise were presented. Amylase, lipase tests, and CMV serum tests must be considered for every HIV positive patient hospitalized for the study of ambiguous progressive symptoms. The absence of abdominal pain, nausea, vomiting or other characteristic features of pancreatitis cannot exclude a diagnosis of pancreatitis in these patients. Management requires quick decision making, prevention of respiratory failure at all times and treatment of any hydroelectrolytic disorder that may be present.
Acknowledgments
The authors thank Dr. Rosa Nuñez Melgar Yañez and Dr. Eloy Ordaya Espinoza from the Department of Infectious Diseases of Hospital Nacional Rebagliati Martins for their revisions of this manuscript.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Funding source
Self-funded.
REFERENCES
1. Forsmark CE, Baillie J. AGA Institute Clinical Practice and Economics Committee, AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132(5):2022-44. [ Links ]
2. Ledesma-Heyer J, Arias Amaral J. Pancreatitis Aguda. Med Int Mex. 2009;25(4):285-94. [ Links ]
3. Kelesidis T. Gastrointestinal symptoms among ambulatory HIV patients: appropriate symptom management requires improved symptom recognition. Ann Gastroenterol. 2012;25(3):186. [ Links ]
4. Thompson T, Lee M, Clarke T, Mills M, Wharfe G. Prevalence of gastrointestinal symptoms among ambulatory HIV patients and a control population. Ann Gastroenterol 2012; 25 (3): 243-48. [ Links ]
5. Manocha AP, Sossenheimer M, Martin SP, Sherman KE, Venkatesan T, Whitcomb DC, et al. Prevalence and predictors of severe acute pancreatitis in patients with acquired immune deficiency syndrome (AIDS). Am J Gastroenterol. 1999;94(3):784-9. [ Links ]
6. Bush ZM, Kosmiski LA. Acute pancreatitis in HIV-infected patients: are etiologies changing since the introduction of protease inhibitor therapy? Pancreas. julio de 2003;27(1):e1-5. [ Links ]
7. Drew WL. Nonpulmonary manifestations of cytomegalovirus infection in immunocompromised patients. Clin Microbiol Rev. 1992;5(2):204-10. [ Links ]
8. Wolf P, Reiser JR, Fellow JE, Haghighi P. Pancreatitis in patients with AIDS presumptively due to CMV. J Clin Lab Anal. 1989;3(3):152-5. [ Links ]
9. Toribio-Rosario I, Gonzáles-Suero J, García-Díaz L, Núñez-Minaya P, Almonte-Cabrera P, Cruz I. Pancreatitis aguda por citomegalovirus: reporte de un caso. Rev Med Dom. 1995;56(1):36-40. [ Links ]
10. Perdan-Pirkmajer K, Koren-Kranjc M, Tomsic M. A successfully treated pancreatitis caused by a CMV infection in a lupus patient. Lupus. 2011;20(10):1104-5. [ Links ]
11. Terada T. Cytomegalovirus-associated severe fatal necrotizing pancreatitis in a patient with interstitial pneumonitis treated with steroids. An autopsy case. JOP. marzo de 2011;12(2):158-61. [ Links ]
12. Kamalkumar BS, Agarwal SK, Garg P, Dinda A, Tiwari SC. Acute pancreatitis with CMV papillitis and cholangiopathy in a renal transplant recipient. Clin Exp Nephrol. 2009;13(4):389-91. [ Links ]
13. González-Calixto C, Ruiz-Tachiquín ME, Burgueño-Ferreira J, Aguilera P, Espinoza-Rojo M. Detección temprana y altamente sensible de citomegalovirus en muestras de plasma humano VIH-positivas. Bioquimia 2009;34(3):129-36. [ Links ]
14. Kalkan IH, Dağli U. What is the most accurate method for the diagnosis of cytomegalovirus (CMV) enteritis or colitis? Turk J Gastroenterol. 2010;21(1):83-6. [ Links ]











 texto en
texto en