Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.1 Bogotá Jan./Mar. 2014
A Case Report of Complete Intraoperative Double-balloon Enteroscopy Assisted by Laparoscopy to treat of Peutz-Jeghers Syndrome
Rómulo Darío Vargas R. MD. (1), Valeria Atenea Costa B. MD. (2), Gonzalo Moros MD. (3), Jaime Alvarado Bestene MD. (4)
(1) Internist and Gastroenterologist at San Ignacio University Hospital in Bogotá, Colombia.
(2) Internist and Gastroenterology Fellow at Pontificia Universidad Javeriana and San Ignacio Hospital in Bogotá, Colombia.
(3) Associate Professor of Laparoscopic and Minimally Invasive Surgery at the Hospital Universitario San Ignacio in Bogotá, Colombia.
(4) Internist, Gastroenterologist and Professor at the Pontificia Universidad Javeriana and San Ignacio University Hospital in Bogotá, Colombia.
Received: 16-09-13 Accepted: 19-12-13
Abstract
Peutz-Jeghers syndrome is characterized by hamartomatous polyps primarily located in the small intestine. Most of these patients undergo several endoscopic or surgical resections. This study reports the case of a female patient who underwent double balloon enteroscopy assisted by intraoperative laparoscopy for resection of polyps.
Keywords
Peutz-Jeghers, double balloon enteroscopy, laparoscopy.
INTRODUCTION
Hamartomatous polyptous polyposis syndromes constitute a group of at least six different rare diseases that require endoscopic management. Although there are no prospective surveys available that would prove the validity of therapeutic approaches, knowledge of genetic bases and pathological manifestations of these diseases can be used to adapt interventional and monitoring approaches for affected patients (1).
Hamartomatous polyptous polyposis syndromes include juvenile polyposis, Bannayan-Riley-Ruvalcaba Syndrome, Peutz-Jeghers Syndrome, Cowden disease and a few mixed polyposis syndrome which are characterized by adenomas, hyperplasic polyps and other lesions (1).
Peutz-Jeghers syndrome is an autosomal dominant condition characterized by the development of hamartomatous polyps throughout the gastrointestinal tract which are associated with mucocutaneous pigmentation (2).
Classic surgical management with multiple enterotomies and polyp removal has been replaced in recent years by endoscopic surgery.
The endoscopic surgery performed on this patient will be explained in the review.
CASE REPORT
This is the case of 14-year-old female patient who had been diagnosed with PeutzJeghers syndrome at the age of 10 years. The patient had no family history of gastrointestinal tract disease.
When first diagnosed, her symptoms indicated that she had suffered from the syndrome for about one year. Every 3 months she had had intermittent abdominal pain located primarily in the epigastrium which appeared after eating and which lasted approximately 2 hours. The pain was relieved without medication. She also suffered from occasional constipation.
She had consulted with her physician on many occasions because of similar symptoms, and had been told to change her diet and to take aluminum hydroxide. Despite this, she had not improved. On one occasion she presented abdominal pain, vomiting and weight loss after constipation with fecal impaction that had been treated with enemas and diet.
Due to the persistence of abdominal pain, an intestinal obstruction was considered. She was evaluated by a pediatric gastroenterologist who found lentigines on her lips in addition to the findings previously described. These findings were consistent with Peutz Jeghers Syndrome (Figure 1).
When a colonoscopy was performed, a giant 5 cm pedunculated polyp was observed in the sigmoid colon. When the polyp was resected, the biopsy showed a hamartomatous polyptous polyp with focal high grade dysplasia whose margins were free from dysplasia. When an upper endoscopy was performed, 20 sessile polyps measuring 2 to 4 mm in diameter were found. Biopsies of these lesions were compatible with hyperplasic polyps.
When retrograde double balloon enteroscopy was performed, a small sessile polyp was observed in the ascending colon with nodular lesions in the terminal ileum. Based on all of this, a diagnosis of Peutz-Jeghers was made.
In 2009 the first infraumbilical laparotomy and resection of the small intestine was performed, and the patient's postoperative evolution was appropriate. A month later the patient underwent enteroclysis (double contrast study of the small intestine) the results of which were normal.
A year after diagnosis of Peutz Jeghers Syndrome, the patient developed another intestinal obstruction which required laparotomy. Then, in 2011, an ileo-ileal intussusception without acute abdomen or obstruction was diagnosed. Magnetic resonance enterography showed onion-like stratification of the layers of the loop inside of another loop without secondary ischemia. A new laparotomy with enterotomy, polypectomy and disinvagination was performed.
Hyperplasic gastric polyps recurred without evidence of Helicobacter pylori. During the last enteroscopy 5 polypoid masses were resected from the small intestine, the largest of which had a diameter of 3.5cm. Biopsies were compatible with hamartomatous polyps without dysplasia.
The patient came to Hospital San Ignacio for scheduled laparoscopically guided enteroscopic polypectomy. The physical examination showed HR: 78 and RR: 18. The patient's general appearance was good and she was well hydrated and had no fever. She had hyperpigmented facial and labial macules, a soft abdomen that could be depressed without pain. Her surgical wounds were fine.
During the laparoscopy she was diagnosed with intussusception. Adhesions were removed, a jejunostomy was performed, and polyps were resected. The procedure lasted 5 hours.
An intestinal loop was exteriorized, a purse-string ligature was tied with vycryl 3-0 suture, and a 2cm enterotomy was cut.
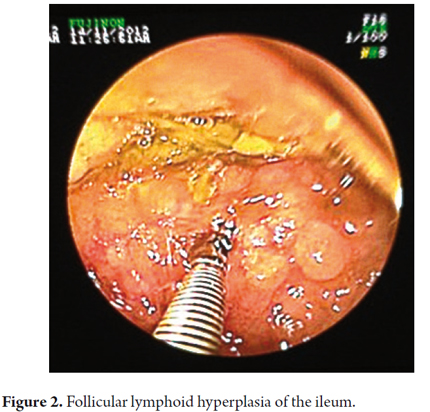
The enteroscope was inserted through the opening of the enterotomy and advanced toward the ileocecal region. The laparoscopic surgeon used a technique to advance the enteroscope that consisted of bunching up the intestine like the sleeve of a shirt to shorten it and allow the instrument to advance further than it otherwise would be able to. The same procedure was performed in the opposite direction toward the angle of Treitz. The procedure revealed a cobblestone pattern of nodular mucosa in the terminal ileum which suggested lymphoid nodules. Biopsies were taken (Figure 2). A 3mm polyp was observed in the terminal ileum 50cm from the valve. It was resected with a loop. Another soft and slightly irregular anastomotic area was observed in the proximal ileum and biopsied.
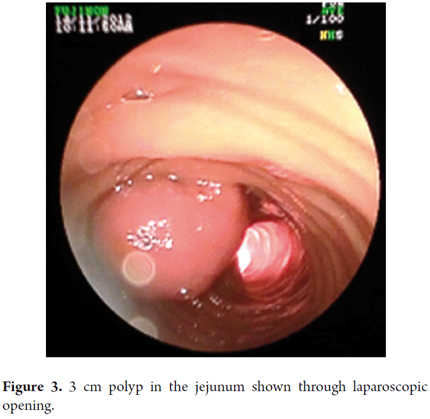
In the middle jejunum a 3cm pseudo-pedunculated polyp was found that corresponded to the head of the intussusception. It was endoscopically resected (Figure 3).
The polyp was raised with submucosal injection and resected with a diathermic loop in a one-step procedure. The region was checked through laparoscopy but no perforation was found.
Serosal lacerations were found in three different locations at the end of the procedure and were repaired with vycryl 3-0 sutures.
The ostomized intestinal segment was resected while outside of the body and a side-to-side anastomosis was created. The enterotomy was closed with the double staple technique, and the borders were reinforced. The trocars were extracted under laparoscopic vision, the pneumoperitoneum was evacuated and the skin was closed.
Surgical findings included viscera-visceral and viscera-parietal adhesion syndromes which were predominant in the infraumbilical region, old intestinal sutures located at 180cm, 230cm and 300cm after the Treitz ligament, and an area of intussusception in the middle jejunum 180cm after the Treitz ligament. It was completely reduced.
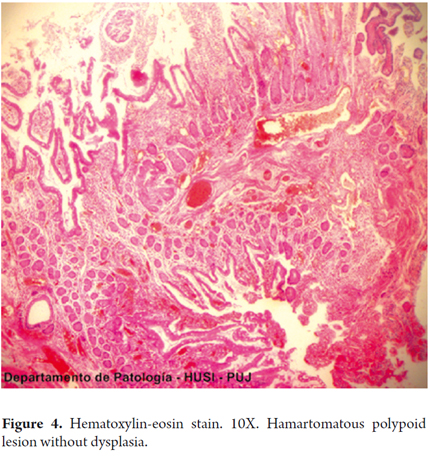
Anatomical and pathological diagnoses showed hamartomatous polyps with no evidence of dysplastic alterations or malignancy in the jejunum and distal ileum. Alterations of the ileal mucosa were compatible with follicular hyperplasia (Figure 4).
The patient's postoperative evolution was successful and without complications.
DISCUSSION
Opinion and diagnosis
This syndrome was named after Peutz who observed a relationship between intestinal polyps and mucocutaneous macules in 1921. Jeghers was added in the 1940s. The syndrome's occurrence has a male to female ratio of 1:1, and the average age at the moment of diagnosis is 23 years old in males and 26 years old in females (1).
Peutz-Jeghers syndrome is a rare disorder: with an incidence of 1 per 8,300 to 29,000 live births it is less common than adenomatous polyposis (2).
Although hamartomatous polyps are typically benign lesions, they are responsible for the majority of complications in Peutz-Jeghers syndrome including intussusception, bowel obstructions and bleeding (2).
Distinguishing this syndrome from other forms of polyposis is usually not problematic since the polyps are bigger and are more numerous in the small intestine. This condition typically begins with an intestinal obstruction or invagination in the second or third decade of life. The risk of intussusception before 20 years of age is 50% (3, 4).
The diagnostic criteria for Peutz-Jeghers syndrome are two or more hamartomatous polyps, one hamartomatous polyp and pigmented mucocutaneous lesions, or the presence of a typical polyp in a patient with a family history of the syndrome (3).
Polyps do not have specific endoscopic features and can only be differentiated from other types of polyposis by histopathology (5).
Family history is absent in up to 45% of cases. Mutations in LKB1 (STK11) in chromosome 19p13 are found in approximately 50% of affected families. The phenotype is more severe in families with missense mutations than in those with nonsense mutations (2).
Clinical features
The main clinical features of Peutz-Jeghers syndrome are the result of gastrointestinal polyposis which can cause abdominal pain, intussusception and bleeding. Hamartomatous polyps can be detected in 88% of patients with Peutz-Jeghers syndrome. The majority of them are detected in the small intestine (6).
They are most likely to be found in the jejunum, followed by the duodenum, the colon and the stomach. A third of the patients experience symptoms secondary to polyps in the small intestine during the first decade of life, and 50% to 60% of patients experience symptoms, especially those due to intestinal obstructions and intussusception, before they are 20 years old (6).
Histology
- The cells of a hamartomatous polyp typically derive from stromal or mesenchymal stem cells. However ectodermic and endodermic cells can also be involved (5).
- Although the majority of polyps are hamartomatous, in some cases polyps have adenomatous changes and focal features of adenocarcinoma (7).
- Dysplasia is very uncommon, though a sequence of hamartomatous polyp-adenoma-carcinoma has been suggested (2, 4).
- Polyps are typically multilobular with papillary surfaces, and they resemble tubulovillous adenomas. These polyps are covered by hyperplasic epithelium. There may be displacement of the epithelial tissue so that it secretes mucin into the submucosa, muscularis propria and beyond the bowel wall. When this occurs it causes the polyp to mimic well differentiated and mucinous adenocarcinoma (2).
- Typical histological features of hamartomatous polyps include smooth muscle cells branching like a tree but covered with normal epithelium (3).
Cancer risk
Patients with this syndrome have increased risks of cancer and malignant tumors outside of the colon in the pancreas, stomach, breasts, ovaries, testicles (Sertolli cell tumor) and cervix (4).
The risk of developing cancer by the age of 70 is 85%. One study including 419 patients reported a risk of developing gastrointestinal cancer by the age of 70 of 57%. Colorectal cancer was the most common cancer with a lifetime risk of 39%, while the cumulative risk of pancreatic cancer was 11% (4).
The risks of developing gastric cancer, cancer of the small intestine and biliary cancer have also increased. The range of risks reported for the development of breast cancer is 31% to 50% (4).
Giardiello has provided the best analysis of the risk of cancer in Peutz-Jeghers syndrome in a study of 210 patients. The relative risk for any cancer during the lifetime of these patients is 15.2, with risks in all parts of the intestine, lung, breast, uterus and gonads. The cumulative risk for any cancer among 15-64 year olds is a staggering 93% (1).
Treatment
Some researchers have suggested that polyps larger than 1.5 cm should be removed when detected. However, a survey carried out in Taiwan showed that some patients who underwent abdominal surgery for polyp removal experienced postoperative complications such as short bowel syndrome and ileus which led to undernourishment and poor quality of life (7).
Classically, complications secondary to small intestine polyposis were managed with exploratory laparotomies, reductions of areas of intussusception, surgical polypectomies, multiple enterotomies and resections of small intestine segments. External palpation and transillumination were conventionally used for identification of small polyps during surgery, but these methods led to repeated laparotomies and additional resections of the small intestine. This exposed patients to the high risks of morbidity and mortality associated with multiple surgical procedures and also occasionally resulted in short bowel syndrome (2).
The recommended follow up for these patients consists of contrast x-rays every two followed by an enteroscopy to resect polyps larger than 15 mm (8).
The diagnostic value of video capsule endoscopy has been studied in patients with Peutz-Jeghers syndrome and found to be generally safe, well tolerated and useful for detection of polyps in the small intestine. Although the video capsule can detect polyps smaller than 5mm, it cannot precisely determine the location and size of polyps. In addition, the video capsule frequently produces false negatives, and there is growing evidence that even large lesions can be missed. A Portuguese survey reported that 20% (5/26) of the polyps larger than 11mm were not diagnosed by video capsules in 14 patients (3).
Since x-rays and video capsules are purely diagnostic, therapeutic options for small intestine polyps have been limited to double-balloon enteroscopy and laparoscopic enteroscopy. The first is less invasive and can be performed on an outpatient basis without requiring surgical assistance. The shape of the intestines may limit the ability to resect large polyps endoscopically (8).
According to the literature, double balloon enteroscopy has been successfully performed in children as young as two years old. The facts that the abdominal cavity is smaller, the intestinal walls are thinner, and the intestinal lumen is narrower must be taken into consideration. Performing this procedure in children is technically more difficult than in adults and requires better skills to guarantee successful performance (9).
Many patients with Peutz-Jeghers syndrome have had previous abdominal surgery with subsequent formation of intra-abdominal adhesions. As the technique of double-balloon enteroscopy requires free movement of the intestine within the abdominal cavity, it is limited by the formation of post-surgical intra-abdominal adhesions (8).
The classical surgical approach through multiple enterotomies and removal of polyps has been modified in recent years by the use of an approach which uses endoscopic surgery (2).
Ohmiya et al. were the first to describe the use of double-balloon enteroscopy for diagnosis and treatment of Peutz-Jeghers syndrome. They resected multiple polyps measuring from 10mm to 60mm from the jejunums and ileums of two patients without producing bleeding or perforation. Since then, several studies have reported high diagnostic and therapeutic yields from double-balloon enteroscopy in patients with Peutz-Jeghers syndrome (3).
Yamamoto and Sugano developed a technique of double-balloon enteroscopy to improve access to the small intestine within a relatively short period of time. The double-balloon method not only allows endoscopic visualization of the entire small intestine but also allows removal of tissue samples and interventional therapies, including balloon dilation of benign stenoses and polypectomy (10).
Obstruction of the small intestine in a patient with Peutz-Jeghers syndrome can be managed successfully with minimally invasive techniques. Treatment of an obstruction in these patients consists of removing the hamartomatous polyp. Repeated episodes of intussusception occur in at least 10% of these cases. This can be treated intraoperatively with colonoscopy and enteroscopy assisted with laparoscopy. Once polyps have been removed from the gastrointestinal tract, a follow-up examination is recommended in two to three years. Polyps larger than 1.5 cm in diameter require another complete gastrointestinal evaluation with endoscopic removal of polyps (10).
Generally, the rate of complications after double-balloon enteroscopy is estimated at 0.8%, the most severe of which is acute pancreatitis with a risk of 0.2% to 0.3% after treatment with an antegrade approach (3).
As with conventional endoscopy, the risk of serious complications is higher in therapeutic enteroscopy (4.3%) than in diagnostic endoscopy, mainly due to bleeding (3%) (3).
Consequently, the use of serial double balloon enteroscopy provides a means to perform prophylactic polypectomy in patients with Peutz-Jeghers syndrome that prevents complications such as intussusception and bleeding (11).
A Japanese institution has developed a therapeutic strategy for patients with Peutz-Jeghers syndrome that begins with endoscopic resection of polyps in the small intestine. Polyps with diameters greater than 20 mm are prioritized to reduce the risk of intussusception. Only large or irregularly shaped polyps are recovered for histopathological examination. Most small polyps have been resected without recovery (11).
If all large polyps cannot be resected during the first session, the next session is scheduled 6 months later. Endoscopic follow-up is carried out at regular annual intervals once all large polyps have been resected (11).
The Japanese study evaluated the effectiveness of this strategy of endoscopic treatment of small intestine polyps in patients with Peutz Jeghers syndrome (11). Fifteen patients treated from 2000 to 2009 were included in the study. A total of 88 double balloon enteroscopies were conducted in these patients during the period. The average number of double balloon enteroscopies per patient was 5.9, with a range between 3 and 10 (11).
Double-balloon enteroscopy has high success rates for inspection of the entire small intestine. Success rates for total enteroscopy range from 40% to 80%. The success rate for total enteroscopy in this study was 70.0% (11).
Several important aspects of intraoperative enteroscopy can vary. They include the choice of laparotomy versus laparoscopy for intra-abdominal access, the endoscope used and the technique used to insert the endoscope (12).
The standard procedure involves a laparotomy followed by enterotomy, usually in the middle of the small intestine, or two small incisions through which the endoscope is introduced. The preferred tool is a standard pediatric colonoscope, but a push enteroscope or even a standard gastroscope can be used (12).
Intraoperative enteroscopy through an enterotomy offers the best option to examine the small intestine as a whole and to minimize trauma (12).
Intraoperative enteroscopy can be performed via laparotomy or assisted by laparoscopy. Although these approaches allow overall inspection of the bowel and resection of polyps in one single procedure, surgical manipulation of the intestine can be significant and lead to intraoperative intestinal dilation as well as serious postoperative ileus (8).
The combined endoscopic surgical technique was first described in 1985 by Mathus Vliegen and Tytgat who treated five patients with 5 to 20 individual polypectomies. This was followed by several reports of the use of similar techniques to manage the small intestine intraoperatively. The use of the combined technique provides a clean small intestine with maximum control of polyposis. This approach decreases the rate of laparotomies and short bowel syndrome, and prolongs the asymptomatic period in these patients. Similarly, excision of small polyps that may be missed when only surgery is accomplished (2).
Laparoscopic reduction has been described in patients with complicated polyposis with intussusception, and cases of laparoscopically assisted enteroscopy in patients with intestinal bleeding have also been reported (2, 10, 13, 14).
By combining double balloon enteroscopy with laparoscopy, a one-step minimally invasive procedure has been developed that can be used to monitor small intestine polyps and to treat patients with Peutz-Jeghers syndrome (8).
Complications
The rate of acute pancreatitis in patients who underwent double balloon enteroscopy treatment was 2.7%, 2.7% suffered bleeding after the procedure, 1.4% experienced perforations and the overall rate of complications was 6.8% (11).
Complication rates of intraoperative enteroscopy have ranged from 0% to 52% and include intramural hematomas, mucosal laceration, perforations, mesenteric hemorrhaging, ileus, pancreatitis, intestinal ischemia, intestinal obstructions, infections of incisions and postoperative pulmonary infections (12).
Dutch authors have described 29 diagnostic and therapeutic double-balloon enteroscopy procedures in 13 patients with Peutz-Jeghers syndrome with multiple polypectomies of 10mm polyps. No complications occurred during the procedures or during follow-up. However, two other studies reported a complication rate of up to 6.8%, including acute pancreatitis (2.7%) and post-polypectomy syndrome (5%) (3).
Another study assessed the feasibility and usefulness of double-balloon enteroscopy in the management of bowel diseases in five children with Peutz-Jeghers syndrome whose average age was 12.9 years. Complete enteroscopies were achieved and polypectomies were successful in two of the five patients. Although there were no complications related to enteroscopy, one patient who underwent a double balloon enteroscopy assisted by laparoscopy developed a pelvic abscess. Since there was no intestinal perforation, this was probably a complication of laparoscopy (3).
Although most studies have report no mortality; mortality related to the procedure or to postoperative complications has been reported in 11%. In one study, one patient died of peritonitis after resection of the small intestine and the development of an anastomotic fistula (12).
We consider it important to report this case because in the search of the literature on the subject, we found no reported cases of patients with Peutz-Jeghers syndrome in Colombia who had undergone elective polypectomy by laparoscopic-guided double-balloon enteroscopy.
The purpose of presenting the case is related to show the relevance of multidisciplinary management of a patient minimally treated, despite several prior interventions.
The procedure has now been shown to be technically possible, safe, and reproducible with excellent results.
REFERENCES
1. Shin SK, Boland CR. Endoscopic Management in Juvenile Polyposis, Peutz-Jeghers Syndrome, and Other Hamartomatous Polyposis Syndromes. Techniques in Gastrointestinal Endoscopy. 2006;8(3):119-25. [ Links ]
2. Amaro R, Diaz G, Schneider J, Hellinger MD, Stollman NH. Peutz-Jeghers syndrome managed with a complete intraoperative endoscopy and extensive polypectomy. Gastrointest Endosc. 2000;52(4):552-4. [ Links ]
3. Korsse SE, Dewint P, Kuipers EJ, van Leerdam ME. Small bowel endoscopy and Peutz-Jeghers syndrome. Best Pract Res Clin Gastroenterol. 2012;26(3):263-78. [ Links ]
4. Jass JR. Gastrointestinal polyposes: clinical, pathological and molecular features. Gastroenterol Clin North Am. 2007;36(4):927-946, viii. [ Links ]
5. Kopacova M, Tacheci I, Rejchrt S, Bures J. Peutz-Jeghers syndrome: diagnostic and therapeutic approach. World J Gastroenterol. 2009;15(43):5397-408. [ Links ]
6. Ohmiya N, Taguchi A, Shirai K, Mabuchi N, Arakawa D, Kanazawa H, et al. Endoscopic resection of Peutz-Jeghers polyps throughout the small intestine at double-balloon enteroscopy without laparotomy. Gastrointest Endosc. 2005;61(1):140-7. [ Links ]
7. Chen T-H, Lin W-P, Su M-Y, Hsu C-M, Chiu C-T, Chen P-C, et al. Balloon-assisted enteroscopy with prophylactic polypectomy for Peutz-Jeghers syndrome: experience in Taiwan. Dig Dis Sci. 2011;56(5):1472-5. [ Links ].
8. Ross AS, Dye C, Prachand VN. Laparoscopic-assisted double-balloon enteroscopy for small-bowel polyp surveillance and treatment in patients with Peutz-Jeghers syndrome. Gastrointest Endosc. 2006;64(6):984-8. [ Links ].
9. Lin TK. Enteroscopy in the pediatric population. Techniques in Gastrointestinal Endoscopy. 2013;15(1):36-40. [ Links ]
10. Gonzalez AMM, Clapp B. Laparoscopic management of small bowel intussusception in a 16-year-old with Peutz-Jeghers syndrome. JSLS. 2008;12(3):332-4. [ Links ]
11. Sakamoto H, Yamamoto H, Hayashi Y, Yano T, Miyata T, Nishimura N, et al. Nonsurgical management of small-bowel polyps in Peutz-Jeghers syndrome with extensive polypectomy by using double-balloon endoscopy. Gastrointest Endosc. 2011;74(2):328-33. [ Links ]
12. Schulz H-J, Schmidt H. Intraoperative enteroscopy. Gastrointest Endosc Clin N Am. 2009;19(3):371-9. [ Links ]
13. Zanoni ECA, Averbach M, Borges JLA, Corrêa PAFP, Cutait R. Laparoscopic treatment of intestinal intussusception in the Peutz-Jeghers syndrome: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2003;13(4):280-2. [ Links ]
14. Kong S-S, Taib NA, Mahadeva S. Successful management of intussusception with total polyp clearance in Peutz-Jeghers syndrome using a combined endoscopic and surgical approach. BMJ Case Rep. 2009;2009. [ Links ]











 text in
text in