Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.2 Bogotá Apr./June 2014
Clinical Aspects of Fatty Liver Disease at a Tertiary Medical Center in Bogotá from 2009 to 2013
Jhon E. Prieto Ortiz, MD. (1), Santiago Sánchez Pardo, MD. (2), Leonardo Rojas Díaz, MD. (2), Sandra Huertas Pacheco, MD. (3)
(1) Gastroenterologist and Hepatologist at the Clínica Universitaria Colombia in Bogotá, Colombia.
(2) Physician at the Fundación Universitaria Sanitas in Bogotá, Colombia.
(3) Pathologist and Epidemiologist at the Clínica Universitaria Colombia in Bogota, Colombia.
Received: 11-12-13 Accepted: 08-05-14
Abstract
Introduction: Nonalcoholic fatty liver disease (NAFLD), or simply fatty liver, is a major cause of hepatic disease worldwide: its prevalence is approximately 30% in adults. In our environment the clinical characteristics of these patients are not known.
Methodology: This was a descriptive and retrospective review of medical records from January 1, 2009 to May 31, 2013 of 266 patients diagnosed with fatty liver disease in the hepatology outpatient service at the Clínica Universitaria Colombia.
Results: Of the 266 patients included in this study, 52.3 % were men and 47.7 % were women. The mean age at diagnosis was 51.6 years. The most frequently found antecedent of importance to the development of NAFLD was dyslipidemia which was found in 113 patients (42.5 %). 127 (47.8%) patients had nonalcoholic steatohepatitis (NASH), and 108 (40.6%) had simple steatosis. Thirty-one patients (11.6%) had cirrhosis which was classified according to CHILD scale: 22 (70.9%) were classified as A, 8 (25.8%) were classified as B, and one (3.2 %) was classified as C. Liver biopsies were taken from 31 patients (11.6%).
Conclusions: Elements of metabolic syndrome, especially dyslipidemia, are often identified in our patients with FLD. Since most of these patients are in early stages of the disease with a low percentage of cirrhotic patients, it may be that the disease progresses more slowly in our environment than elsewhere. This is a hypothesis that should be validated in other studies.
Keywords
Fatty liver, risk factors, NASH, NAFLD, hepatic steatosis, liver cirrhosis, fibrosis.
INTRODUCTION AND DEFINITION
Fatty liver or non-alcoholic fatty liver disease (NAFLD) was originally described in the eighties by Ludwig (1). Its asymptomatic form is frequently found when a blood test reports elevated transaminases, but it is also one of the main causes of liver disease worldwide (2, 4).
Definition
From a histological point of view the term fatty liver or NAFLD encompasses a spectrum ranging from simple fatty steatosis (benign condition) to fatty liver with transaminase elevation or NASH (nonalcoholic steatohepatitis) in which steatosis is accompanied by the phenomenon of ballooning and inflammation. It also includes progressive fibrosis which can lead to cirrhosis with its inherent complications (2-6).
Fatty liver is defined as an ultrasound finding of hepatic steatosis with or without inflammation and/or a finding of fibrosis in the absence of the secondary causes listed below (5-6):
- Alcohol consumption greater than 20 g/day for men and 10g/day for women
- Use of hepatotoxic drugs such as glucocorticosteroids, isoniazid, methotrexate, amiodarone, and tamoxifen within the 6 months prior to the study
- Positive serology for hepatitis B or C
- Ferritin concentration > 1000 mg/L.
- Anti smooth muscle antibodies serum titers > 1:160 or anti mitochondrial antibodies > 1:140
PREVALENCE
Worldwide the prevalence of NAFLD in adults has been estimated to be between 20% and 30%. Prevalence varies according to the population studied and the method used for diagnosis (ultrasonography, liver biopsy or elevated liver enzymes) (7-10). It is much more common in industrialized countries where most patients are diagnosed between the ages of 40 and 50 years, although it is being diagnosed more and more frequently in children (11).
NAFLD is associated with risk factors such as obesity and alcoholism in 30% to 100 % of cases, type 2 diabetes mellitus in 10% to 75 % of cases, dyslipidemia in 90% of cases, and metabolic syndrome (MS) in 25 % of cases. Fatty liver is the hepatic manifestation of this syndrome: 90% of patients with NAFLD have at least one characteristic of metabolic syndrome, and a third have all of the criteria (3, 4-6). It is important to note that NAFLD can occur in patients who are not overweight (12). and that fatty liver is associated with an increased risk of death from any cause. It is a predictor of future cardiovascular events regardless of the person's age, gender, LDL levels, smoking and metabolic syndrome (13-16). Several studies have demonstrated a link between fatty liver and the onset of diabetes regardless of the presence of conventional risk factors such as obesity, insulin resistance and metabolic syndrome. This suggests that fatty liver may have a causal relationship with the genesis of diabetes which is probably associated with insulin resistance in the liver (17-20). This entity's ethnic distribution shows that Hispanics are most affected (58 %) followed by Caucasians (44 %) and finally African Americans (35 %) (9, 13, 14). Recent data shows increasing incidence parallel to the worldwide increase in obesity and diabetes which are both elements of metabolic syndrome (9, 13, 17).
NATURAL HISTORY
We know that simple steatosis may progress to NASH and then to cirrhosis. The risk for progression to cirrhosis from simple steatosis after 10 to 20 years is 0% to 4 %, but 5% to 10% of patients with NASH can develop cirrhosis in approximately 5 years (2, 4, 5, 6, 13, 21, 22, 40). A study by Rahman concludes that approximately 20 % of cases progress from simple fatty steatosis to NASH, 20% of these progress to cirrhosis, and some develop into hepatocellular carcinoma (23). Hepatocellular carcinoma has even been described in patients with NASH but without cirrhosis which establishes that fatty liver is a risk factor for this tumor (23, 24).
PATHOGENESIS
Although the pathogenesis of fatty liver has not been fully elucidated, the best supported theory involves a sequence of two main events.
1. Insulin resistance and a progressive accumulation of fatty acids in hepatocytes. Lipids accumulating as glycerolipids, glycerophospholipids and sterols
2. Alterations of the mitochondrial function of the hepatocytes which generate accumulation of the aforementioned fatty acids and results in an inability to maintain the B- oxidation, reduction in VLDL secretion, increased oxidative stress, lipid peroxidation, apoptosis, increased inflammatory response mediated by the release of tumor necrosis factor (TNF) involved in ballooning, fibrosis and Mallory's hyaline (3-6, 25-26). Dysfunction of insulin signaling responsible for lipid peroxidation and oxidative stress which causes inflammation and apoptosis through transcription factors and kinase-dependent signaling pathways (27-29).
CLINICAL AND LABORATORY FINDINGS
Most patients are asymptomatic although isolated cases have fatigue, weakness and pain in the right upper quadrant. In advanced stages NAFLD is associated with clinical complications of portal hypertension and cirrhosis (2, 4, 6, 13).
Elevation of transaminases is usually mild to moderate, but normal levels do not exclude a diagnosis of NAFLD. Elevation of ALT is clinically relevant as it has been proven to be a predictor of the genesis of insulin resistance, diabetes mellitus, cardiovascular disease and metabolic syndrome in patients with fatty livers (30, 40). Other relevant laboratory findings include alkaline phosphatase (ALP) three times or more than its normal value and elevated ferritin (31). Albumin, bilirubin and clotting times are only altered during cirrhosis (6, 13, 32-34).
LIVER BIOPSIES
A liver biopsy is considered to be the best tool for confirming a diagnosis of NAFLD, for assessing inflammation and fibrosis, and for providing information about prognosis (6, 10, 32). Some authors suggest that liver biopsies should even be performed on patients in high-risk groups such as obese and diabetic patients, those over the age of 45 years, and patients with AST/ALT ratio > 1, insulin resistance , hypertension and/or hypertriglyceridemia (8, 22, 35, 36). Given the limitations of liver biopsies and controversies about their use, various biomarkers have been studied as measures of the degree of fibrosis for diagnosis of fatty liver. These include alpha-fetoprotein, ALT, GGT, non-esterified fatty acids, and altered glucose levels. None of these provide the same level of information about a patient's prognosis as a liver biopsy which encourages continued systematic use of biopsies (32, 33, 35, 36). A histological finding of fatty liver disease on the basis of fat infiltration can be classified as mild when infiltration into hepatocytes is between 5% and 33 %, moderate when it is between 34% and 66 %, and severe when it is over 66 %. Other relevant histological findings include lobular inflammation, ballooning and fibrosis (36-39).
TREATMENT
Treatment is based on modification of lifestyle and risk factors including encouragement of exercise, weight loss, a healthy low-calorie diet, and continuous monitoring for early detection of fibrosis and/or cirrhosis. In addition, effective therapies with minimal side effects have been developed to control the progression of the disease. These include administration of antioxidants such as vitamins E and C which have been shown to reverse high levels of transaminases, cholesterol and hyaluronic acid although they do not reverse elevated levels of cytokines and inflammation does not improve (4, 6, 18, 41). Weight loss, even when it is the sole factor, is associated with histological improvement (41, 42). The Greek Atorvastatin and Coronary-heart-disease Evaluation (GREACE) demonstrated that lipid-lowering agents such as statins can benefit patients with NAFLD as well as reducing cardiovascular risks (43).
Other interventions such as administration of angiotensin II receptor (ARB ) inhibitors, ursodeoxycholic acid, and L-carnitine which carries lipids in the mitochondria can also be useful. Peripheral insulin sensitizers such as biguanides and thiazolidenediones have been shown to normalize transaminase levels, inflammatory response and hepatic steatosis. Probiotics reduce the intestinal bacterial translocation and decrease the inflammatory response in the liver (44-50). Surgical interventions such as the specific combination of restrictive and malabsorptive bariatric surgery using the technique of Roux-en-Y gastric bypass (RYGBP) and a modified Fobi- Capella technique have shown benefits and improvements of inflammation demonstrated by liver biopsies (51).
Clinical characteristics of patients diagnosed with fatty liver disease and their relation to metabolic diseases were unknown in our environment and we did not have proper statistics. Consequently, the epidemiological data presented here is based on international literature, but this study describes the clinical features of fatty liver in a series of 266 patients at the Clinica Universitaria Colombia.
OBJECTIVE
The objective of this study is to describe the clinical characteristics of 266 patients diagnosed with fatty liver disease in the hepatology service at the Clinica Universitaria Colombia in Bogotá, Colombia during the study period.
METHODOLOGY
All medical records of patients diagnosed with fatty liver disease attending the outpatient department of hepatology at the Clinica Universitaria Colombia during the period from January 1, 2009 to May 31, 2013 were reviewed. A descriptive analysis of each of the variables studied was made. For continuous variables means and standard deviations were estimated, for categorical variables proportions were estimated and presented in text, tables and/or graphs employing EXCEL and SPSS.
Design, population and definition of variables
A descriptive, retrospective study with review of the medical records of adult patients diagnosed with fatty liver who attended the department of hepatology of Clinica Universitaria Colombia. The study only included patients with a fatty liver diagnosis based on ultrasound findings and/or increased transaminases and/or liver biopsy. Data from the physical examination and laboratory test, demographic characteristics, reason for patient referral, background information regarding the clinical history were pooled and tabulated.
Ethical Considerations
This is a retrospective study using data from the medical records of patients. No intervention or intentional modification of the biological, physiological, psychological or social variables of individuals was performed. It was conducted according to the principles stated in the Eighteenth World Medical Assembly (Helsinki, 1964). The identification data of the patients and their diagnoses were not entered in the publications and the investigators handled all medical history data with complete confidentiality.
RESULTS
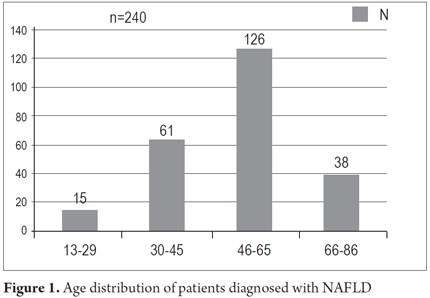
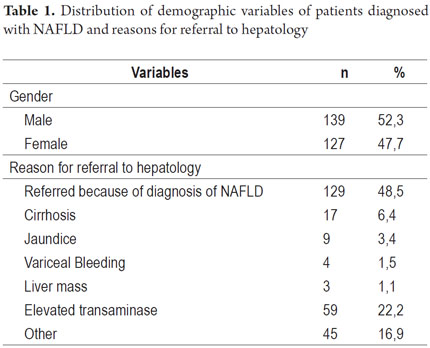
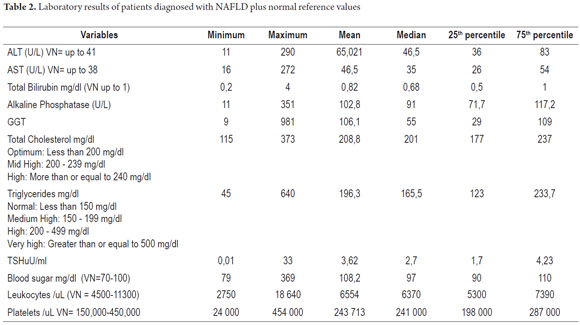
The average age of the 266 patients diagnosed with fatty liver disease was 51.6 years. The age range was 13 to 86 years. Age distribution was as follows: 13 to 29 years - 15 patients, 30 to 45 years - 61 patients, 46 to 65 - 126 patients, and 66 to 86 years - 38 patients (Figure 1). There were 139 male patients (52.3 %) and 127 female patients (47.7%) The main reasons for referral to the hepatology department were diagnoses of fatty liver disease (129 patients, 48.5%), elevated transaminases (59 patients, 22.2%), cirrhosis (17 patients, 6.4%), jaundice (9 patients 3.4%), variceal bleeding (4 patients, 1.5%), liver masses (3 patients, 1.1%) and other reasons (45 patients, 16.9%) (Table 1). Laboratory parameters during patient admission are presented in Table 2. Average transaminase levels should be highlighted. Average ALT was 65 U/L and average AST was 46 U/L while the highest ALT level was 290 U/L and the highest AST was 272 U/L. Cholesterol and triglycerides had mean levels of 208 and 196 with maximum values of 373 and 640 mg/dl respectively. The average fasting blood glucose value was 108.2 mg/dl while the highest level was 369 mg/dl. Demographic characteristics of patients are presented in Table 1.
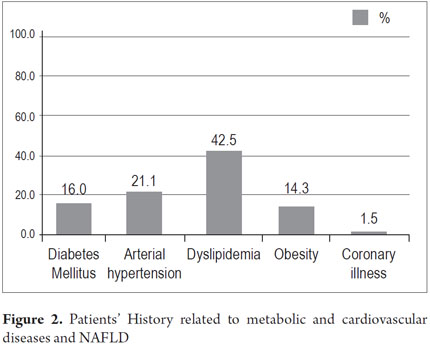
Patients' medical histories related to fatty liver disease and metabolic syndrome showed dyslipidemia in 113 patients (42.5%), hypertension in 56 (21.1%), diabetes mellitus in 46 (16 %), obesity in 38 (14.3%), and coronary artery disease in 4 (1.5%) (Figure 2). Some patients had more than 1 factor. The average Body Mass Index (BMI), a measure of whether and how much patients are overweight and/or obese, was 27kg/m2. The highest BMI was 45 kg/m2 (Figure 2).
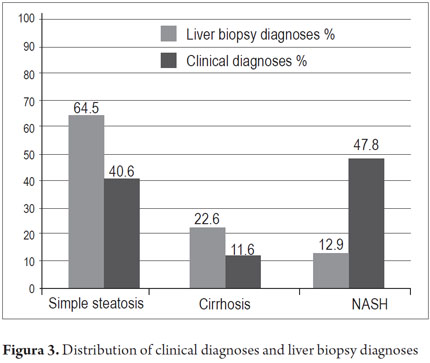
Of 266 patients diagnosed with NAFLD, 127 presented NASH (47.8 %), 108 simple steatosis (40.6%) and 31 cirrhosis (11.6%). The latter were classified according to the CHILD scale: 22 classified as A (70.9%), 8 classified as B (25.8%) and 1 classified as C (3.2 %).
Liver Biopsies were performed on 31 patients (11.6%), of whom 20 (64.5%) were diagnosed with non-significant fatty alterations or simple steatosis (<5 %), 4 with NASH (12.9%), and 7 patients with cirrhosis (22.6%). All data is presented in Figure 3.
DISCUSSION
The average age of all patients was 51.3 years and the age range in which NAFLD was most commonly diagnosed was 46 to 65 years. This is consistent with international studies in which the average age of diagnosis is between 40 and 50. The distribution by gender behaved similarly: NAFLD diagnoses were more common among men (52.3%) than among women (47.7 %) (5, 6, 10). Dyslipidemia was found in 42.5% of the patients, hypertension in 21.1 %, diabetes in 16%, obesity in 14.3% and coronary heart disease in 1.5% of the patients. All of these are factors in metabolic syndrome consistent with the link in the literature between NAFLD and metabolic diseases (6-25, 26). Only 1.5 % of patients had a history of coronary heart disease. Transaminase and lipid values found in this study agree with those reported in the international literature (5, 30, 40).
Cirrhosis was clinically diagnosed in 31 patients (11.6%). Most of them were classified Child A. Of these 31 select patients, cirrhosis was confirmed histologically in 22.6%. Although this data might create an idea that the natural history of NAFLD is relatively benign, it should be remembered that it currently affects up to 30% of the world's population, and we should be alert to the possible of a late diagnosis. Measures must be taken to diagnose this condition early and to prevent it (4, 6, 13). As a final note, it should be pointed out that none of the patients were diagnosed with hepatocellular carcinoma despite the risk in this group of patients. Patients with cirrhotic fatty liver disease should be screened for this condition every 6 months.
In conclusion, a high frequency of factors involved in metabolic syndrome was found in our patients with NAFLD. Prospective studies need to be done in Colombia to provide guidelines for early detection and intervention against this disease.
REFERENCES
1. Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55(7):434-8. [ Links ]
2. McCullough AJ. The clinical features, diagnosis and natural history of nonalcoholic fatty liver disease. Clin Liver Dis. 2004;8(3):521-533, viii. [ Links ]
3. Mavrogiannaki AN, Migdalis IN. Nonalcoholic Fatty liver disease, diabetes mellitus and cardiovascular disease: newer data. Int J Endocrinol. 2013;2013:450639. [ Links ]
4. Santos LF, Hernandez G, Varon A, Betran O, Botero RC, Mejia G. Enfermedad hepática por infiltración grasa noalcohólica. La nueva pandemia del milenio. Rev Col Gastroenterol. 2010; 25(4):380-98. [ Links ]
5. Lewis JR, Mohanty SR. Nonalcoholic fatty liver disease: a review and update. Dig Dis Sci. 2010;55(3):560-78. [ Links ]
6. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Am J Gastroenterol. 2012;107(6):811-26. [ Links ]
7. Lazo M, Clark JM. The epidemiology of nonalcoholic fatty liver disease: a global perspective. Semin Liver Dis. 2008;28(4):339-50. [ Links ]
8. Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatol Baltim Md. 2004;40(6):1387-95. [ Links ]
9. Younossi ZM, Stepanova M, Afendy M, Fang Y, Younossi Y, Mir H, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2011;9(6):524-530.e1; quiz e60. [ Links ]
10. Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140(1):124-31. [ Links ]
11. Rashid M, Roberts EA. Nonalcoholic steatohepatitis in children. J Pediatr Gastroenterol Nutr. 2000;30(1):48-53. [ Links ]
12. Omagari K, Kadokawa Y, Masuda J-I, Egawa I, Sawa T, Hazama H, et al. Fatty liver in non-alcoholic non-overweight Japanese adults: incidence and clinical characteristics. J Gastroenterol Hepatol. 2002;17(10):1098-105. [ Links ]
13. Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34(3):274-85. [ Links ]
14. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA J Am Med Assoc. 2010;303(3):235-41. [ Links ]
15. Bellentani S, Saccoccio G, Masutti F, Crocè LS, Brandi G, Sasso F, et al. Prevalence of and risk factors for hepatic steatosis in Northern Italy. Ann Intern Med. 2000;132(2):112-7. [ Links ]
16. Falck-Ytter Y, Younossi ZM, Marchesini G, McCullough AJ. Clinical features and natural history of nonalcoholic steatosis syndromes. Semin Liver Dis. 2001;21(1):17-26. [ Links ]
17. Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013;5(5):1544-60. [ Links ]
18. Attar BM, Van Thiel DH. Current concepts and management approaches in nonalcoholic fatty liver disease. ScientificWorldJournal. 2013;2013:481893. [ Links ]
19. Ahmed MH, Barakat S, Almobarak AO. Nonalcoholic fatty liver disease and cardiovascular disease: has the time come for cardiologists to be hepatologists? J Obes. 2012;2012:483135. [ Links ]
20. Lv W-S, Sun R-X, Gao Y-Y, Wen J-P, Pan R-F, Li L, et al. Nonalcoholic fatty liver disease and microvascular complications in type 2 diabetes. World J Gastroenterol WJG. 2013;19(20):3134-42. [ Links ]
21. Powell EE, Cooksley WG, Hanson R, Searle J, Halliday JW, Powell LW. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatol Baltim Md. 1990;11(1):74-80. [ Links ]
22. Caldwell SH, Crespo DM. The spectrum expanded: cryptogenic cirrhosis and the natural history of non-alcoholic fatty liver disease. J Hepatol. 2004;40(4):578-84. [ Links ]
23. Rahman RN and Ibdah JA, Nonalcoholic fatty liver disease without cirrhosis is an emergent and independent risk factor of hepatocellular carcinoma: a population based study. Hepatology. 2012. [ Links ]
24. Ertle J, Dechêne A, Sowa J-P, Penndorf V, Herzer K, Kaiser G, et al. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int J Cancer J Int Cancer. 2011;128(10):2436-43. [ Links ]
25. Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatol Baltim Md. 2003;37(4):917-23. [ Links ]
26. Gastaldelli A, Cusi K, Pettiti M, Hardies J, Miyazaki Y, Berria R, et al. Relationship between hepatic/visceral fat and hepatic insulin resistance in nondiabetic and type 2 diabetic subjects. Gastroenterology. 2007;133(2):496-506. [ Links ]
27. Cusi K. The role of adipose tissue and lipotoxicity in the pathogenesis of type 2 diabetes. Curr Diab Rep. 2010;10(4):306-15. [ Links ]
28. Kawano Y, Cohen DE. Mechanisms of hepatic triglyceride accumulation in non-alcoholic fatty liver disease. J Gastroenterol. abril de 2013;48(4):434-41. [ Links ]
29. Malaguarnera M, Di Rosa M, Nicoletti F, Malaguarnera L. Molecular mechanisms involved in NAFLD progression. J Mol Med Berl Ger. 2009;87(7):679-95. [ Links ]
30. Ghamar-Chehreh ME, Amini M, Khedmat H, Moayed Alavian S, Daraei F, Mohtashami R, et al. Elevated alanine aminotransferase activity is not associated with dyslipidemias, but related to insulin resistance and higher disease grades in non-diabetic non-alcoholic fatty liver disease. Asian Pac J Trop Biomed. 2012;2(9):702-6. [ Links ]
31. Kowdley KV, Belt P, Wilson LA, Yeh MM, Neuschwander-Tetri BA, Chalasani N, et al. Serum ferritin is an independent predictor of histologic severity and advanced fibrosis in patients with nonalcoholic fatty liver disease. Hepatol Baltim Md. 2012;55(1):77-85. [ Links ]
32. Ahmed MH. Biochemical markers: the road map for the diagnosis of nonalcoholic fatty liver disease. Am J Clin Pathol. 2007;127(1):20-2. [ Links ]
33. Haukeland JW, Konopski Z, Linnestad P, Azimy S, Marit Løberg E, Haaland T, et al. Abnormal glucose tolerance is a predictor of steatohepatitis and fibrosis in patients with non-alcoholic fatty liver disease. Scand J Gastroenterol. 2005;40(12):1469-77. [ Links ]
34. Kara M, Genc H, Tapan S, Meral C, Ercin CN, Erdal M, et al. Alpha fetoprotein levels and its relationship with histopathological findings in patients with non-alcoholic fatty liver disease. Eur Rev Med Pharmacol Sci. 2013;17(11):1536-41. [ Links ]
35. Brunt EM, Kleiner DE, Wilson LA, Unalp A, Behling CE, Lavine JE, et al. Portal chronic inflammation in nonalcoholic fatty liver disease (NAFLD): a histologic marker of advanced NAFLD-Clinicopathologic correlations from the nonalcoholic steatohepatitis clinical research network. Hepatol Baltim Md. 2009;49(3):809-20. [ Links ]
36. Neuschwander-Tetri BA, Clark JM, Bass NM, Van Natta ML, Unalp-Arida A, Tonascia J, et al. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatol Baltim Md. 2010;52(3):913-24. [ Links ]
37. Brunt EM, Tiniakos DG. Alcoholic and nonalcoholic fatty liver disease. En: Odze RD, Goldblum JR, Editores. Surgical pathology of the GI tract, liver, biliary tract and pancreas. 2009; 2.a Edición, Elsevier. Philadelphia. p.1007. [ Links ]
38. Pais R, Charlotte F, Fedchuk L, Bedossa P, Lebray P, Poynard T, et al. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol. 2013;59(3):550-6. [ Links ]
39. Dam-Larsen S, Franzmann M, Andersen IB, Christoffersen P, Jensen LB, Sørensen TIA, et al. Long term prognosis of fatty liver: risk of chronic liver disease and death. Gut. 2004;53(5):750-5. [ Links ]
40. Fracanzani AL, Valenti L, Bugianesi E, Andreoletti M, Colli A, Vanni E, et al. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes. Hepatol Baltim Md. 2008;48(3):792-8. [ Links ]
41. Musso G, Gambino R, Cassader M, Pagano G. A meta-analysis of randomized trials for the treatment of nonalcoholic fatty liver disease. Hepatol Baltim Md. 2010;52(1):79-104. [ Links ]
42. Promrat K, Kleiner DE, Niemeier HM, Jackvony E, Kearns M, Wands JR, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatol Baltim Md. 2010;51(1):121-9. [ Links ]
43. Athyros VG, Tziomalos K, Gossios TD, Griva T, Anagnostis P, Kargiotis K, et al. Safety and efficacy of long-term statin treatment for cardiovascular events in patients with coronary heart disease and abnormal liver tests in the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) Study: a post-hoc analysis. Lancet. 2010;376(9756):1916-22. [ Links ]
44. Sanyal AJ, Chalasani N, Kowdley KV, McCullough A, Diehl AM, Bass NM, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362(18):1675-85. [ Links ]
45. Ratziu V, Charlotte F, Bernhardt C, Giral P, Halbron M, Lenaour G, et al. Long-term efficacy of rosiglitazone in nonalcoholic steatohepatitis: results of the fatty liver improvement by rosiglitazone therapy (FLIRT 2) extension trial. Hepatol Baltim Md. 2010;51(2):445-53. [ Links ]
46. Masterton GS, Plevris JN, Hayes PC. Review article: omega-3 fatty acids - a promising novel therapy for non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2010;31(7):679-92. [ Links ]
47. Leuschner UFH, Lindenthal B, Herrmann G, Arnold JC, Rössle M, Cordes H-J, et al. High-dose ursodeoxycholic acid therapy for nonalcoholic steatohepatitis: a double-blind, randomized, placebo-controlled trial. Hepatol Baltim Md. 2010;52(2):472-9. [ Links ]
48. Xiao J, Guo R, Fung ML, Liong EC, Tipoe GL. Therapeutic approaches to non-alcoholic fatty liver disease: past achievements and future challenges. Hepatobiliary Pancreat Dis Int HBPD INT. 2013;12(2):125-35. [ Links ]
49. Ekstedt M, Franzén LE, Mathiesen UL, Holmqvist M, Bodemar G, Kechagias S. Statins in non-alcoholic fatty liver disease and chronically elevated liver enzymes: a histopathological follow-up study. J Hepatol. 2007;47(1):135-41. [ Links ]
50. Kelishadi R, Farajian S, Mirlohi M. Probiotics as a novel treatment for non-alcoholic Fatty liver disease; a systematic review on the current evidences. Hepat Mon. 2013;13(4):e7233. [ Links ]
51. Vargas V, Allende H, Lecube A, Salcedo MT, Baena-Fustegueras JA, Fort JM, et al. Surgically induced weight loss by gastric bypass improves non alcoholic fatty liver disease in morbid obese patients. World J Hepatol. 2012;4(12):382-8. [ Links ]











 text in
text in