Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.2 Bogotá Apr./June 2014
Does the Spyglass Cholangioscope Exist in our Midst? And is it Useful?
John Ospina Nieto, MD. (1), Issac Raijman, MD. (2), Benedicto Velasco, MD. (3)
(1) Gastrointestinal surgeon and digestive endoscopist. Scientific Director of the Digestive Studies Unit (UNESDI), Gastroenterologist at Clínica Colombia of Organización Sanitas Internacional, Gastroenterologist at the Centro de Enfermedades Digestivas in Bogotá, Colombia.
(2) President, Digestive Associates of Houston, PA in Houston, Texas. Former Director of Therapeutic Endoscopy Division of Gastroenterology and Digestive Diseases at the University of Texas Health Science Center in Houston, Texas. Bogotá, Colombia.
(3) Medical Internist and Gastroenterologist of the Universidad Nacional de Colombia, Gastroenterologist at Reina Sofia Clinic of Organización Sanitas Internacional, Gastroenterologist at Gastromedicall in Bogota, Colombia.
Received: 29-07-13 Accepted: 08-05-14
Cholangioscopy is to the biliary and pancreatic ducts what colonoscopy is for the colon ... in their absence all we would have would be cholangiographic x-ray images or images from barium enemas.
Abstract
Despite today's high quality duodenoscopes, fluoroscopy equipment and x-ray equipment, a direct endoscopic view of the biliary tree and the pancreas is often required for the best diagnosis and treatment of a patient's pathology. Initial experience with peroral cholangioscopy was very promising, but the enthusiasm for this technique quickly declined due to the extreme fragility and high cost of cholangioscopes and also because of the advent of new imaging techniques.
As the result of recent technological advances in endoscopic equipment, cholangioscopy has undergone a number of changes that include development of ber instruments that are smaller in diameter and which cost less than earlier versions. Consequently, despite the fact that his is still considered to be an emerging technique, peroral cholangioscopy is increasingly being used as a very useful tool for diagnosis and treatment of various pancreatic and biliary diseases including cholangiocarcinoma, giant calculi, stenoses and small polyps.
This article briefly reviews the topic, introduces new equipment and the advantages thereof, and focuses on highlighting the usefulness of this method for certain groups of patients as it is actually being implemented in Colombia over the last year ago with success.
Keywords
Spyglass cholangioscopy, pancreatoscopy.
INTRODUCTION
The history of biliary exploration dates back to 1895 when Dr. Hans Kehr placed a rubber tube inside the common bile duct through the cystic duct stump to bypass the common bile duct (1). Yet it was not until 1968 when endoscopic exploration of the biliary tree was introduced with the development of endoscopic retrograde cholangiopancreatography (ERCP) by Doctors McCuney and Schorbe (2). This was, undoubtedly, a process that changed the diagnosis and treatment of biliary-pancreatic diseases (3). In spite of this, and of currenly having duodenoscopes and high quality fluoroscopy and radiology equipments, it is often that a direct endoscopic visualization of the biliary and pancreatic tree is required to refine the diagnosis and treatment of the underlying pathology.
Initial experiences with transpapillary and peroral cholangioscopy (PC) by Nakajima and Kawai in 1976 and multiple other studies from Japan and Europe were very promising, but the enthusiasm quickly declined due to the advent of new imaging techniques such as Computed Axial Tomography, Endosonography and MRIs, but mostly due the extreme fragility and high cost of cholangioscopes (3).
In recent decades different types of cholangioscopes have been developed. For direct visual examination of the bile and pancreatic ducts we now have intraoperative, percutaneous and peroral exploration equipment. The great technological advances in endoscopic equipment coupled with the interest of manufacturers seeking to popularize and improve the use of these procedures has led to modifications of these systems over time. Percutaneous and, especially peroral, techniques are now positioned as very useful tools for diagnosis and treatment of various pancreatic and biliary diseases such as cholangiocarcinomas, giant calculi, stenoses and small polyps (4, 5).
Although cholangioscopy was first developed several years ago, its use did not become popular until recently. Consequently, it is considered to be an emerging technique. In recent years it has undergone a number of changes including the development of ber smaller diameter instruments. These changes have allowed it to be used with increasing frequency. In this article we provide a brief review, present new types of equipment and their advantages, and especially highlight the usefulness of the procedure for certain patient groups.
PERORAL CHOLANGIOSCOPY AND EXPERIENCE WITH IT IN COLOMBIA
Experience with ERCPs in the past three decades has shown that conventional cholangiography is the most appropriate therapeutic option or diagnostic study for certain diseases. While cholangioscopy was developed around 1950, its technical and scientific limitations led it to fall into disuse. Intraoperative cholangioscopy was finally implemented successfully only in the 1960's (19). Peroral cholangioscopy was developed around 1970 by Dr. Urakami who published the first successful performance of the technique. Then in the 1980s, the concept of mother-child endoscopes began to win adherents and cholangioscopies began to be performed with relative success. Nevertheless, its procedure time of close to 3 hours was too long, and the need for two expert endoscopists combined with the cost and brittleness of the equipment made the technique unpopular (19, 20).
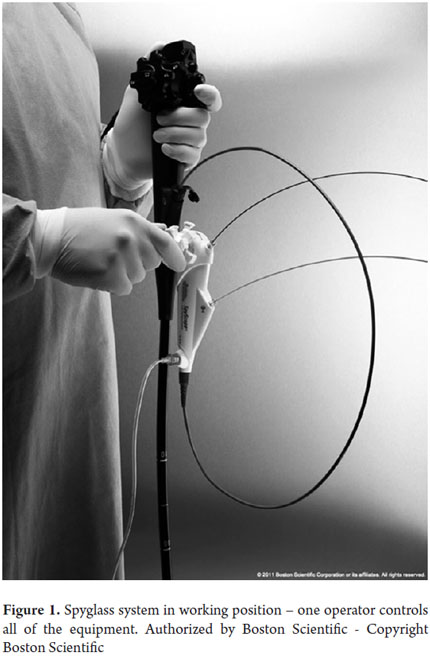
In recent years, very significant technological advances in mini-endoscopes have allowed for the development of new equipment and optical systems. One of these systems is the Spyglass® cholangiopancreatoscopy (Boston ScientificCorp, Natick, Mass) seen in Figure 1. This is a fiber-optic system that is inserted through the working channel of the duodenoscope. It uses either an external 10 French catheter or a disposable Spyscope which has a 1.2 mm working channel. This allows passage of biopsy forceps or lithotripsy equipment (laser or electrohydraulic probes). It also has a 0.6mm irrigation canal for washing the ducts. This system possesses great advantages over its ancestors, and, while more work still needs to be done on the quality of the image, it offers the possibility of working with one operator plus a reusable fiber-optic tool and an easy-to-handle system. The Spyglass® (Boston ScientificCorp, Natick, Mass), which is available in Colombia, has the right combination of features for performance of peroral cholangioscopies as a real and useful technique complementary to ERCPs. Spyglass allows good access, direct visualization, performance of biopsies and instrumentation of bile and pancreatic ducts for diagnosis and treatment of diseases in these pathways (6).
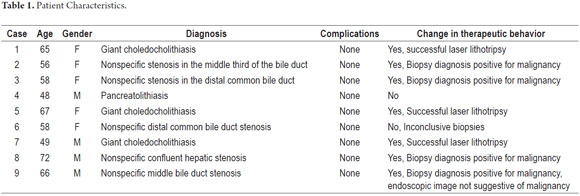
As in many other countries, this technique is still emerging. Nevertheless, serious progress is being made in several clinical institutions including Clinica Colombia and Reina Sofia of the Sanitas Organization. These hospitals have used this technique since March 2012 when the first theoretical and practical Spyglass workshop was given in our country under the guidance of Dr. Raijman. It included lectures, cases of laser lithotripsy to treat giant stones, and reviews of biliary strictures of unknown origin. The workshop was attended by renowned specialists from this country. Afterwards, the training continued in Houston in Dr.Raijman's unit. Finally, in September 2012, Doctors Ospina and Velazco started the program with the first pancreatoscopy performed in Colombia followed by 9 cases of biliary cholangioscopy to date (Table 1). In all cases the diagnoses were correct, outcomes were good, and there were and no complications. Recently, a group led by Dr Ivan Unigarro from Clinica Imbanaco in Cali also began the exciting experience of Spyglass cholangioscopy with a couple of successful diagnoses.
DESCRIPTION OF THE TECHNIQUE
Although performing a peroral cholangioscopy requires experience for proper management, it also has a number of advantages over other techniques such as ERCPs. Notable among the advantages are the facts that it does not usually require additional analysis, images are obtained directly and in three dimensions (not in two dimensions or in black and white), and the instrument is more manageable and resilient than that used for percutaneous cholangioscopy. In addition, the procedure has lower rates of morbidity and less risk of neoplastic spread in cases where malignancy is suspected (1, 5, 19).
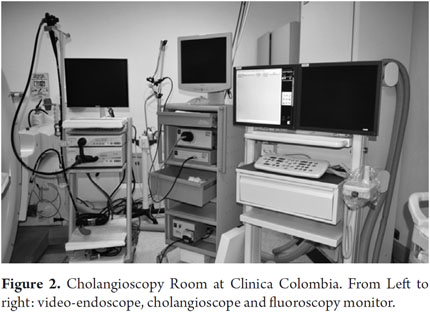
To conduct a peroral cholangioscopy it is necessary to have a trained staff, appropriate rooms and the necessary equipment and accessories for study and treatment of biliopancreatic pathologies. The room must have a fluoroscope or an image intensifier that provides high quality images to allow proper interpretation and radiological guidance. It must also have a video-endoscopy tower to which the duodenoscope can be connected, an additional cholangioscope tower (Figure 2). Also, all suction, resuscitation, monitoring, and anesthesia equipment required in complex therapeutic procedures must be at hand. In cases in which giant stones are suspected, a laser is also a necessity (7, 11).
Before discussing technical issues, it should be noted the biliary specialist must acquire new skills and knowledge in order to perform cholangioscopy. This includes new anatomical, radiological and endoscopic signs and symptoms, learning new maneuvers, and especially learning how to coordinate the simultaneous use of two endoscopes and continuous observation of three monitors.
The first step of the procedure is the introduction of the duodenoscope in a conventional manner into the second portion of the duodenum, and then through the papillary orifice to access the bile duct or the pancreas. Then conventional ERCP is performed to assess the radiological image and to map the workspace (8). Once the area of interest has been identified, the Spyscope or Cholangioscopic catheter is inserted through the work channel. Then the spyglass fiber-optic cable is introduced. To properly conduct the study, intermittent saline solution irrigation is needed throughout the entire study to remove waste, bile detritus, mucus and fluids.
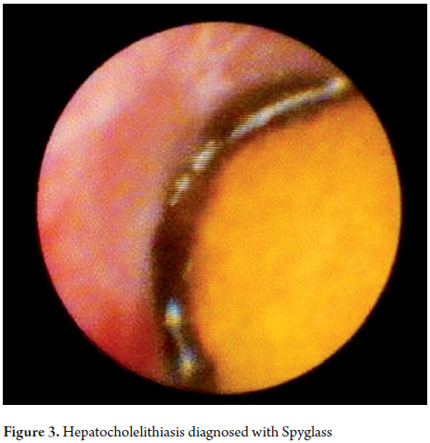
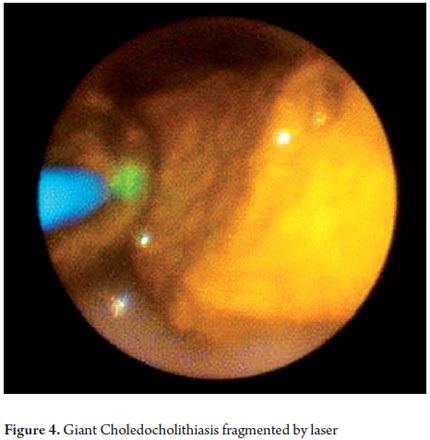
Once the area of the study has been identified, the biopsy or lithotripsy procedure is performed according to the case (Figures 3, 4, 5 and annex 1). It should be noted that this is an invasive therapeutic examination which requires sedation or general anesthesia and antibiotic prophylaxis (8, 9, 10).
INDICATIONS
Although this technology is still emerging, various works and publications have shown that it has ample diagnostic and therapeutic uses in cases in which conventional cholangiography has left the diagnosis in doubt or in which it has therapeutic limitations (see Table 2) (11).
The technique has three areas of diagnostic usefulness:
1. Filling defects which may correspond to benign or malignant intraductal tumors, extrinsic lesions or calculi.
2. Stenoses whose etiologies cannot be discerned using conventional imaging methods and endoscopy, and in which seemingly benign strictures can be malignant.
3. Post liver transplant lesions including infected strictures, ulceration due to cytomegalovirus, and less hemobilia of unknown origin.
It is well known that there must always be clinical suspicion of malignancy in adults who have biliary strictures other than immediate postsurgical and traumatic strictures. It is also well known that diagnostic tools such as cytology and cytology combined with blind transpapillary biopsies make successful diagnoses in only these 30% to 60% of these cases (27).
Cholangioscopy has significantly changed treatment of these patients. Figures are close to 30% after performance of cholangioscopy (11, 12). It can even differentiate between a false stenosis and calculi (11, 15).
The first spyglass studies published by Doctors Chen and Plesko reported that the procedure was successful in 91% of their cases and had the ability to obtain material suitable for histology in 19 of the 20 cases evaluated. Subsequently, several papers have appeared that supported the diagnostic capacity of this technique.
In a series of 102 cholangioscopies, biopsies performed under direct vision with SpyGlass showed 70% sensitivity and 100% specificity for confirming malignancies. Its positive predictive value (PPV) was 100% while its negative predictive value (NPV) was 75% (12). Similarly, a series of 97 patients with in bile duct strictures published by Tsuyuguchi et al. demonstrated 100% diagnostic sensitivity, 86% specificity and 93% accuracy. According to their results, the diagnostic accuracy for filling defects was 100% as direct visualization of the lesion allowed determination of whether the lesion was caused by calculi, a benign stricture or a tumor (18).
Cholangioscopy increases the possibility of differentiating and diagnosing lesions more precisely than either ERCP or magnetic resonance-cholangio-pancreaticography (MRCP). This is true in the aforementioned cases as well as in patients with primary sclerosing cholangitis where its utility for evaluating dominant strictures is as important as well as its role in the evaluation of pancreatic intraductal lesions, chronic pancreatitis, pancretolithiasis and intraductal papillary mucinous neoplasms (IPMN) (19, 21, 22).
Recently this technique has also been used for evaluating choledochal cysts, studying hemobilia of unknown origin, and fungal and viral diseases. It is especially useful in cases of bile duct cytomegalovirus and for post-transplant liver patients (19, 23, 24, 25, 26).
Cholangiopancreatoscopy not only offers more accurate diagnoses than ERCP, it also offers the possibility of performing therapeutic procedures such as the removal of giant gallstones that cannot be removed by conventional means due to their size, location, or adherence to the epithelium. The method also provides the possibility of using fragmentation techniques such as electrohydraulic or laser lithotripsy which are useful for giant stones and in patients with Mirizzi syndrome type II. Successful results have been reported in up to 89% of cases eliminating the need for repeated ERCP + prosthesis or surgical treatment for these patients (19).
SAFETY
Studies confirm that the number of complications with peroral cholangioscopy does not exceed 6% of cases, although two studies report complication rates close to 11% (16, 17). The most common complications are cholangitis, pancreatitis (reported in up 3.8% of cases) (19), perforations and septicemia (9, 11, 15, 16, 17). Although there have been no reports of mortality due to cholangioscopy, there have been serious complications. A comparison of the morbidity of the different techniques shows that peroral cholangioscopy has lower morbidity than does percutaneous cholangioscopy (7).
CONTRAINDICATIONS
In general terms a cholangioscopy can be performed in any patient with indications for ERCP. Likewise, it is contraindicated in any patient in which ERCP is prohibited: this means that it is considered contraindicated in cases of coagulation disorders, and when indications for the procedure are absent. Cholangitis is considered to be a contraindication for cholangioscopy due to the high risk of bacteremia resulting from bacterial translocation during the procedure.
Before ending, it is noteworthy to mention that this technique has already proven beyond a doubt that it is a very useful tool for diagnosis and treatment of complex biliopancreatic pathologies even though there are no studies of its cost-effectiveness because it is still an emerging technique. We expect that it will become an increasingly important technique as it becomes better and better understood and as experience in its use is gained.
Finally, it should be noted that although equipment required to handle is not complex, there are some minimum requirements:
- Training: Performance of peroral cholangioscopy requires a team with extensive experience in endoscopic retrograde cholangiopancreatography (ERCP) and requires additional theoretical and practical training.
- Facilities: As previously mentioned, it is necessary to have a peroral cholangioscopy system that includes everything needed for an ERCP as well as:
- Video display equipment including processor and light source.
- Fiber optic catheters.
- Biopsy clamps suitable for the channel system.
- Laser or electrohydraulic lithotripter.
Organization: Performance of cholangioscopy requires modifying the routine activities of the gastroenterology and endoscopy services in terms of patient scheduling and use of medical and paramedical human resources.
For these reasons the implementation of these procedures has been recommended in 3rd and 4th level institutions that have large numbers of patients, economic, scientific, and technological resources, and which have the appropriate personnel.
We want to finish by highlighting the main idea of the article, which is the current importance and usefulness of this technique in our environment as well as its safety and superior diagnostic and therapeutic performance.
ANNEX 1
Laser lithotripsy procedure with Spyglass by Dr. Antonio Sedici
REFERENCES
1. Nieto DJO. Cirugia Endoscopica al dia: Feliz cumpleaños CPRE [Internet]. Cirugia Endoscopica al dia. 2008 [citado 5 de junio de 2014]. Recuperado a partir de: http://cirugiaendoscopicaaldia.blogspot.com/2008/04/feliz-cumpleaos-cpre.html [ Links ]
2. McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167(5):752-6. [ Links ]
3. Nakajima M, Akasaka Y, Fukumoto K, Mitsuyoshi Y, Kawai K. Peroral cholangiopancreatosocopy (PCPS) under duodenoscopic guidance. Am J Gastroenterol. 1976;66(3):241-7. [ Links ]
4. Judah JR, Draganov PV. Intraductal biliary and pancreatic endoscopy: an expanding scope of possibility. World J Gastroenterol WJG. 28 de mayo de 2008;14(20):3129-36. [ Links ]
5. Nimura Y. Staging cholangiocarcinoma by cholangioscopy. HPB. 2008;10(2):113-5. [ Links ]
6. Reavis KM, Melvin WS. Advanced endoscopic technologies. Surg Endosc. 2008;22(6):1533-46. [ Links ]
7. ASGE Technology Committee, Shah RJ, Adler DG, Conway JD, Diehl DL, Farraye FA, et al. Cholangiopancreatoscopy. Gastrointest Endosc. 2008;68(3):411-21. [ Links ]
8. Shah RJ, Langer DA, Antillon MR, Chen YK. Cholangioscopy and cholangioscopic forceps biopsy in patients with indeterminate pancreaticobiliary pathology. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2006;4(2):219-25. [ Links ]
9. Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video). Gastrointest Endosc. 2007;65(6):832-41. [ Links ]
10. Okugawa T, Tsuyuguchi T, K C S, Ando T, Ishihara T, Yamaguchi T, et al. Peroral cholangioscopic treatment of hepatolithiasis: Long-term results. Gastrointest Endosc. 2002;56(3):366-71. [ Links ]
11. Beltrán P. Cambios en el manejo de las enfermedades biliares con Spyglass. Reunión ACAD. 2009;32(3):125-26. [ Links ]
12. Kurland J, Ozden N, Lee S-H, Pawa R, Sawhney M, Chuttani R, et al. Assessment of SPYGLASS Direct Visualization System for Cholangioscopy and Pancreatoscopy in 102 Consecutive Patients. Gastrointest Endosc. 2009;69(5):AB273. [ Links ]
13. Wright H, Sharma S, Gurakar A, Sebastian A, Kohli V, Jabbour N. Management of biliary stricture guided by the Spyglass Direct Visualization System in a liver transplant recipient: an innovative approach. Gastrointest Endosc. 2008;67(7):1201-3. [ Links ]
14. Bhat YM, Kochman ML. Novel management of complex hilar biliary strictures with the Spyglass Direct Visualization System (with video). Gastrointest Endosc. 2009;69(6):1182-4. [ Links ]
15. Chen YK, Parsi MA, Binmoeller KF, Hawes R, Pleskow DK, Slivka A, et al. Peroral Cholangioscopy (POC) Using a Disposable Steerable Single Operator Catheter for Biliary Stone Therapy and Assessment of Indeterminate Strictures - A Multi-Center Experience Using SPYGLASS. Gastrointest Endosc. 2009;69(5):AB264-AB265. [ Links ]
16. Yamao K, Ohashi K, Nakamura T, Suzuki T, Sawaki A, Hara K, et al. Efficacy of peroral pancreatoscopy in the diagnosis of pancreatic diseases. Gastrointest Endosc. 2003;57(2):205-9. [ Links ]
17. Wang HP, Chen JH, Wu MS, Wang HH, Chou AL, Chang YS, et al. Application of peroral cholangioscopy in an endemic area with high prevalence of hepatocellular carcinoma and choledocholithiasis. Hepatogastroenterology. 2000;47(36):1555-9. [ Links ]
18. Tsuyuguchi T, Fukuda Y, Tsuchiya S, Sakai Y, Saisho H. The Role of Peroral Cholangioscopy For Bile Duct Lesions: Peroral Cholangioscopy For Bile Duct Lesions. Dig Endosc. 2005;17:S53-S56. [ Links ]
19. Judah JR, Draganov PV. Intraductal biliary and pancreatic endoscopy: an expanding scope of possibility. World J Gastroenterol WJG. 2008;14(20):3129-36. [ Links ]
20. Urakami Y, Seifert E, Butke H. Peroral direct cholangioscopy (PDCS) using routine straight-view endoscope: first report. Endoscopy. 1977;9(1):27-30. [ Links ]
21. Tajiri H, Kobayashi M, Ohtsu A, Ryu M, Yoshida S. Peroral pancreatoscopy for the diagnosis of pancreatic diseases. Pancreas. 1998;16(3):408-12. [ Links ]
22. Uehara H, Nakaizumi A, Tatsuta M, Iishi H, Kitamura T, Ohigashi H, et al. Diagnosis of carcinoma in situ of the pancreas by peroral pancreatoscopy and pancreatoscopic cytology. Cancer. 1997;79(3):454-61. [ Links ]
23. Kolodziejski TR, Safadi BY, Nakanuma Y, Milkes DE, Soetikno RM. Bile duct cysts in a patient with autosomal dominant polycystic kidney disease. Gastrointest Endosc. 2004;59(1):140-2. [ Links ]
24. Scotiniotis IA, Kochman ML. Intramural cyst of the bile duct demonstrated by cholangioscopy and intraductal US. Gastrointest Endosc. 2001;54(2):260-2. [ Links ]
25. Huang SP, Wang HP, Chen JH, Wu MS, Shun CT, Lin JT. Clinical application of EUS and peroral cholangioscopy in a choledochocele with choledocholithiasis. Gastrointest Endosc. 1999;50(4):568-71. [ Links ]
26. Kubota H, Kageoka M, Iwasaki H, Sugimoto K, Higuchi R, Honda S, et al. A patient with undifferentiated carcinoma of gallbladder presenting with hemobilia. J Gastroenterol. 2000;35(1):63-8. [ Links ]
27. Draganov PV, Chauhan S, Wagh MS, Gupte AR, Lin T, Hou W, et al. Diagnostic accuracy of conventional and cholangioscopy-guided sampling of indeterminate biliary lesions at the time of ERCP: a prospective, long-term follow-up study. Gastrointest Endosc. 2012;75(2):347-53. [ Links ]











 text in
text in