Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.2 Bogotá abr./jun. 2014
Primary Malignant Melanoma of the Esophagus: A Case Report and Literature review
Elkin Yasmany Cabrera Riascos, MD. (1), Ricardo Oliveros, MD. (2), Jairo Ospina, MD. (2), Jorge Mesa, MD. (3), Ricardo Villarreal, MD. (4), Haylmanrth Contreras, MD. (4)
(1) General Surgery Resident at the Universidad de la Sabana in Chia, Colombia. elkincabreramd@hotmail.com
(2) Department of Gastrointestinal Surgery and Endoscopy at the Instituto Nacional de Cancerología (National Cancer Institute) in Bogotá, Colombia.
(3) Department of Oncological Pathology at the Instituto Nacional de Cancerología in Bogotá, Colombia.
(4) Specialist in Training Gastrointestinal Surgeons and Endoscopists at the Universidad Militar Nueva Granada in Bogota, Colombia.
Received: 30-07-13 Accepted: 08-05-14
Abstract
Primary malignant melanoma of the esophagus is an extremely rare disease: among esophageal tumors its incidence is only 0.1% to 0.2%. The prognosis is generally poor due to the high potential for metastasis. Differential diagnosis of metastatic malignant melanoma can be a challenge for the group treating it. Moreover, managing it requires a multidisciplinary team which includes a gastroenterologist, a pathologist, an oncologist, a medical oncologist, and a dermatologist.
We report an in situ case of primary malignant melanoma of the esophagus in a 45 -year-old patient which was managed with three esophagectomies at the National Cancer Institute of Colombia. In addition, we review the literature.
Keywords
Esophageal neoplasms, melanoma, esophagoscopy, surgery.
INTRODUCCION
Primary malignant melanoma of the esophagus (PMME) is an extremely rare condition with an incidence of 0.0036 cases per one million people every year (1). Approximately 340 cases have been reported in the world literature, accounting for between 0.1% and 0.2% of all esophageal neoplasms (2, 3).
The first case was reported by Baur in 1906, although he considered it to be a metastasis from elsewhere rather than a primary melanoma of the esophagus (4).
The prognoses of these cases are poor because of the great potential for dissemination, especially to the blood and lymph systems. The incidence of metastasis at diagnosis is between 40% and 80% (5).
Clinical manifestations of the disease vary according to the carcinoma in the esophagus. The vast majority of patients are asymptomatic or have nonspecific symptoms such as heartburn and epigastric pain. Dysphagia is uncommon because these are soft tumors. Symptoms such as hematemesis and melena are rare because ulceration is rare. The duration of symptoms prior to diagnosis is approximately 3 months (6).
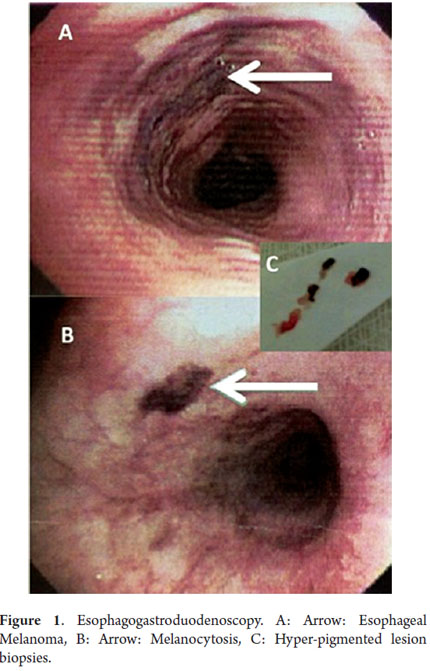
Endoscopically, PMME appears as to be a circumscribed, pigmented polypoid lesion (Except for amelanotic melanoma) which is covered by normal esophageal mucosa (6). A careful check of the entire esophagus is necessary in order to look for melanocytosis and satellite foci of intramural metastasis of the primary lesion.
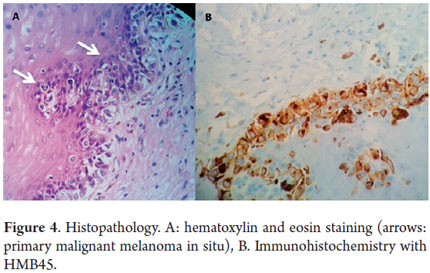
Biopsy sensitivity is only 80% because 20% of these cases are mistaken for poorly differentiated esophageal carcinomas, especially cases of amelanotic melanoma (6). Immunohistochemistry is therefore useful, especially in cases of PMME S100, HMB45 and Melan-A mark positive (7).
The largest study (n = 175) found in the literature was done by Maekawa et al (8). It identified the distribution of tumor locations as follows: 7.1% were in the upper thoracic esophagus, 3.3% were in the upper middle esophagus, 36.3% were in the middle esophagus, 16.5% were in the lower middle esophagus, 26.9% were in the lower esophagus, and 2.7% were at the gastroesophageal junction.
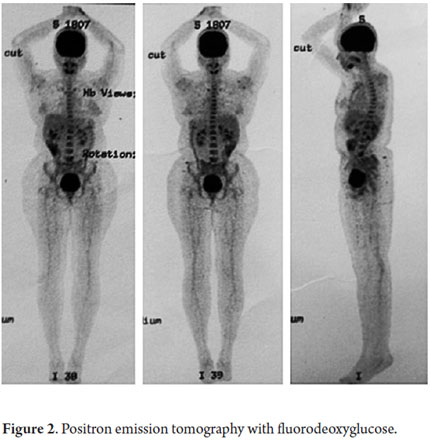
Most PMME metastases occur in regional lymph nodes, supraclavicular lymph nodes, the liver, the lungs and in the bones (6). The disease has great potential for spreading. The incidence of metastases at the time of diagnosis is between 40% and 80% (5). Positron emission tomography using fluorodeoxyglucose as the tracer (FDG-PET) is currently accepted as the technique of choice for detecting metastases originating from solid tumors although its performance in gastrointestinal tract melanoma remains unclear (9).
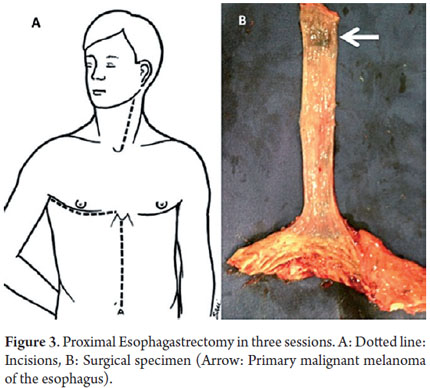
Treatment and prognosis of the disease also remain unclear. Surgery has been used in 60% to 80% of the cases reported in the literature, with proximal esophagogastrectomies used for locally resectable disease. Due to limited amount of information available, there is no consensus regarding the adjuvant treatment of PMME (10).
The average prognosis for patient survival reported by Sabanathan et al. (6) in their series was 10 months, although a study by Volpin (3) reports that the five-year survival rate was 37%. Nevertheless, survival time following treatment depends on the clinical stage at time of diagnosis, and we lack studies that inquire into this factor (10).
CASE REPORT
A 45 year-old black woman who had suffered epigastric pain and heartburn for 10 years came to the outpatient clinic of the Colombian National Cancer Institute. She had no other relevant medical history. Her physical examination was completely normal. In particular, there were no suspicious skin, ocular, anal and cervical lesions. She had already had an esophageal duodenoscopy (EGD) which reported Grade A extra-peptic esophagitis (Los Angeles Classification), acute erosive gastritis, active diffuse antral chronic gastritis, acute erosive duodenitis, duodeno-gastric bile reflux.
Proton pump inhibitors were prescribed, but her systems persisted. Three years later another EGD was performed. It showed two hyper-pigmented zones. One was 2 cm in diameter and was located on the posterior wall of the esophagus 21 cm from the dental arch. The other was 6 mm in diameter and was located on the posterior wall at 31 cm from the dental arch. Biopsies were taken from both (Figure 1). The pathology report showed basal atypical melanoma in-situ with melanocytic proliferation. The lamina propria had lymphocytic infiltration and melanocytic pigmentation.
An FDG-PET was taken. It did not identify any lesions suggesting hypermetabolic tumor or metastatic involvement (Figure 2). Chest and abdominal contrast tomography were normal.
With these studies, the patient was referred to the surgical board of gastrointestinal surgery which decided to perform an esophagogastrectomy with curative intent in three sessions: left cervicotomy, right thoracotomy and midline supraumbilical laparotomy. The process was carried out at the National Cancer Institute in June 2013. Figure 3 shows the surgical specimen.
On the seventh day following surgery, a low output fistula occurred in the esophagogastric anastomosis. A Penrose drain was inserted, and it spontaneously resolved 20 days after surgery.
The final pathology report confirmed the initial diagnosis. The following histopathology was described: primary malignant melanoma in situ (proximal lesion) in radial growth phase (Immunohistochemistry HMB45 and Melan A positive) without stromal invasion. Atypical melanocytosis (distal lesion) without lymphovascular or neural invasion. Tumor-free edges of proximal radial and distal sections. 10 metastasis-free lymph nodes (0/10) (Melan A, HMB45 and CD 68 positive) (Figure 4).
Today, after two months of clinical follow-up as an outpatient, the patient is asymptomatic and has no complications.
DISCUSSION
PMME is a rare condition with an incidence of 0.1% to 0.2% reported in the literature (2, 3). Diagnosis was uncertain until De La Pava et al. (11) demonstrated the presence of benign melanocytes in esophageal mucosa in 4 of 100 autopsies. Subsequently, Ohashi et al. (12) reaffirmed this observation demonstrating the presence of melanocytes in esophageal mucosa in 8% of the population.
Risk factors for the disease have not been identified, and alcohol and tobacco consumption do not appear to be associated. Melanocytosis, a benign condition characterized by an increased number of melanin granules in the melanocyte cytoplasm in the basal stratum of the esophageal mucosa, has been associated with PMME (12). Esophageal melanocytosis occurs in 25% to 30% of patients with PMME (13).
In our patient, the pigmented lesion in the esophagus was documented three years after the first endoscopy. At first, biopsies were inconclusive and immunohistochemical tests were needed to better characterize the histopathological findings. However, she also had a synchronous lesion, distal to the melanoma in situ, which was consistent with melanocytosis.
Although FDG-PET showed no hypermetabolic lesions in this case, it is still a useful tool for staging this disease, especially for evaluation of distant metastases which are diagnosed in 40% to 80% of the patients who are diagnosed with PMME (5, 9). A series by Chalkiadakis et al. reported that 31% had liver metastases, 29% had metastases to the mediastinum, 18% had metastases to the lungs and 13% had metastases to the brain at the time of diagnosis (14).
The diagnostic criteria of Allen and Spitz define cutaneous malignant melanoma as having the typical histological pattern of melanoma with melanin granules within tumor cells and as originating in the squamous epithelium at the junction of the epithelium with nests of atypical melanocytes adjacent to the tumor mass (15).
As reported in the literature, when PMME was locally resectable, it was managed surgically in 60% to 80% of cases (10). For this reason and because of the clinical characteristics of the patient, we performed an esophagectomy in three sessions in order to achieve adequate local and regional lymph node dissection, despite the morbidity that a thoracic approach can entail.
A low output fistula at the esophagogastric anastomosis developed, but it resolved spontaneously. The frequency of this complication varies widely in literature, but it can occur in 10% to 25% of patients undergoing esophagectomies (16).
Yamaguchi et al. (10) analyzed 72 patients who had been surgically treated for PMME from 1993 to 2003 in Japan. They defined several predictive factors including age of patient over 60 years, presence of T2 invasion, presence of local/regional lymph node metastases and distant metastases.
Some adjuvant management options include chemotherapy, chemotherapy combined with radiation therapy, endocrine therapy and immunotherapy. Individually, none of these has shown improvement in the prognosis of the disease, and there is a lack of studies to define response after surgical management. It is difficult to argue if such treatments have some value in PMME management due to the low incidence of the disease.
REFERENCES
1. Westwood DA, Macemon JB, Coulter GN, Chalmers-Watson TA, Roberts RH. Primary oesophageal malignant melanoma. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2011;15(7):1286-8. [ Links ]
2. Wang S, Tachimori Y, Hokamura N, Igaki H, Kishino T, Kushima R. Diagnosis and surgical outcomes for primary malignant melanoma of the esophagus: a single-center experience. Ann Thorac Surg. 2013;96(3):1002-6. [ Links ]
3. Volpin E, Sauvanet A, Couvelard A, Belghiti J. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagus Off J Int Soc Dis Esophagus ISDE. 2002;15(3):244-9. [ Links ]
4. Baur EH. Ein Fall von Primaerem Melanoma de Oesophagus. Arb Geb Pathol Anat Inst Tuebingen. 1906;5:343-54. [ Links ]
5. Li B, Lei W, Shao K, Zhang C, Chen Z, Shi S, et al. Characteristics and prognosis of primary malignant melanoma of the esophagus. Melanoma Res. 2007;17(4):239-42. [ Links ]
6. Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol. 1989;84(12):1475-81. [ Links ]
7. Joob AW, Haines GK 3rd, Kies MS, Shields TW. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1995;60(1):217-22. [ Links ]
8. Maekawa T, Satoh K, Maekawa H, Wada R, Matsumoto M. A case of primary malignant melanoma arising in the esophagus. Nippon Gekakei Rengo Gakkai Zasshi. 2005;30:154-9. [ Links ]
9. Schwimmer J, Essner R, Patel A, Jahan SA, Shepherd JE, Park K, et al. A review of the literature for whole-body FDG PET in the management of patients with melanoma. Q J Nucl Med Off Publ Ital Assoc Nucl Med AIMN Int Assoc Radiopharmacol IAR. 2000;44(2):153-67. [ Links ]
10. Iwanuma Y, Tomita N, Amano T, Isayama F, Tsurumaru M, Hayashi T, et al. Current status of primary malignant melanoma of the esophagus: clinical features, pathology, management and prognosis. J Gastroenterol. 2012;47(1):21-8. [ Links ]
11. De La Pava S, Nigogosyan G, Pickren JW, Cabrera A. Melanosis of the esophagus. Cancer. 1963;16:48-50. [ Links ]
12. Ohashi K, Kato Y, Kanno J, Kasuga T. Melanocytes and melanosis of the oesophagus in Japanese subjects--analysis of factors effecting their increase. Virchows Arch A Pathol Anat Histopathol. 1990;417(2):137-43. [ Links ]
13. Lohmann CM, Hwu WJ, Iversen K, Jungbluth AA, Busam KJ. Primary malignant melanoma of the oesophagus: a clinical and pathological study with emphasis on the immunophenotype of the tumours for melanocyte differentiation markers and cancer/testis antigens. Melanoma Res. 2003;13(6):595-601. [ Links ]
14. Chalkiadakis G, Wihlm JM, Morand G, Weill-Bousson M, Witz JP. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1985;39(5):472-5. [ Links ]
15. Allen AC, Spitz S. Malignant melanoma; a clinicopathological analysis of the criteria for diagnosis and prognosis. Cancer 1953; 6(1):1-45. [ Links ]
16. Schuchert MJ, Abbas G, Nason KS, Pennathur A, Awais O, Santana M, et al. Impact of anastomotic leak on outcomes after transhiatal esophagectomy. Surgery. 2010;148(4):831-838; discussion 838-840. [ Links ]











 texto em
texto em