Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.2 Bogotá abr./jun. 2014
Warning Signs for Eosinophilic Proctocolitis: Two Case Reports
Wilson Daza C., MD. (1), Silvana Dadán, MD. (2), Ana María Rojas V. MD. (3), Edgardo Yaspe, MD. (4)
(1) Pediatric Gastroenterologist, MSc in Clinical Nutrition, Gastronutriped, Director of Graduate Pediatric Gastroenterology University Forest Officer. Bogotá, Colombia. wilson.daza@gastronutriped.com
(2) Clinical Nutritionist, MSc in Clinical Nutrition, Graduate Assistant Professor of Pediatrics and Pediatric Gastroenterology. Universidad El Bosque in Bogotá, Colombia.
(3) Pediatrician, Fellow of Pediatric Gastroenterology at the Universidad El Bosque in Bogota, Colombia.
(4) Medical Pathologist at Labopat in Bogota, Colombia.
Received: 25-10-13 Accepted: 08-05-14
Abstract
We present the cases of two patients diagnosed with eosinophilic proctocolitis without persistence of rectal bleeding which is the most typical manifestation but with perseverance of the eosinophilic inflammation. One purpose of presenting these cases is to emphasize the importance of assessing less relevant demonstrations as part of the strict monitoring of patients in order to decide whether they need colonoscopy and biopsies and to allow redirection of medical nutrition management.
Keywords
Eosinophilic proctocolitis, clinical presentation, food allergy.
INTRODUCTION
Food allergies have a wide spectrum of clinical expressions which are based on three immune triggering mechanisms:
1. Mediation by Immunoglobulin E (IgE). This type of food allergy has acute onset which can involve more than one organ including the skin (urticaria and angioedema), respiratory system (rhinoconjunctivitis and asthma) and gastrointestinal tract (nausea, vomiting and diarrhea).
2. Cell mediated (non IgE). This type may have either acute or chronic development as in the cases of enterocolitis and proctocolitis.
3. Mediation by mixed mechanisms with or without involvement of IgE. This type has late onset and can manifest as atopic dermatitis, eosinophilic esophagitis and eosinophilic gastroenteritis (1, 2).
In the early years of life, the cow's milk protein (CMP) is the most common allergen. Gastrointestinal manifestations of CMP allergy are nonspecific and secondary to inflammation or gastrointestinal dysmotility (2).
CMP allergy has a peak of expression during the first year of life. Its prevalence subsequently decreases to 1% in children older than 6 years old. At preschool ages, its prevalence varies from 1% to 17.5%, between 5 and 16 years it varies from 1% to 13.5%, and in adults its range is from 1% to 4% (1, 2).
Eosinophilic proctocolitis is one of the most likely causes of rectal bleeding in breastfed infants between the first and the sixth month of postnatal life (3). In the eighties it was considered to be a rare disease, but its incidence has been increasing (4). 60% of cases occur during the first 6 months of life in infants fed with breast milk. Resolution occurs around 2 years of age (5).
Diagnosis of food allergies, including eosinophilic proctocolitis, is based on a detailed medical history with emphasis on family and personal histories and on clinical features. A colonoscopy is not a routine procedure for all patients with suspected proctocolitis because diagnosis is primarily clinical. When a colonoscopy is relevant, erythematous lesions, ulcerations, ecchymosis or erosions are observed. Histologically, eosinophilia and acute inflammation are evident (5). The pathology usually shows superficial erosions, eosinophilic infiltration into the lamina propria, crypt abscesses and nodular lymphoid hyperplasia (1, 3).
Treatment involves the restriction of allergens for both the nursing mother and the infant (3, 5). If the probable diagnosis is allergic proctocolitis, 72% to 96% of affected children improve when cows milk is removed from the diet (6). It has been reported that up to 7% of patients require extensively hydrolyzed formula and 5% need a formula based on L-amino acids. These are severe cases including childhood allergies to several or many foods (2).
CASE REPORTS
Case 1
A 25 day old boy was brought to Gastronutriped (GNP - Gastroenterology, Hepatology and Nutrition Unit) in Bogota by his family because he presented rectal bleeding.
From birth the child had consistently suffered from recurrent regurgitation and emetic episodes which were associated with dysphagia and choking crises but without any alteration of appetite or general conditions. Prior to consultation breast-feeding had been supplemented with formula. Three different Stage 1 brands of infant formula had been used without any improvement of symptoms. Three days before the consultation the child presented a single episode of Bristol 5 type stool associated with rectal streaks of blood. On her own initiative, the day before coming to GNP the mother decided to being using a partially hydrolyzed formula and to continue breast feeding. She restricted protein from cow's milk, eggs, nuts and seafood. A stool test's results were normal.
Due to cephalopelvic disproportion, the patient had been delivered by cesarean section after a 38 week pregnancy. Both adequate weight and length were adequate at birth. The child did not present neonatal jaundice and defecated his meconium in the first 24 hours.
The child's father suffers from allergic rhino-conjunctivitis, and a paternal aunt suffers from food allergies to tomatoes, papayas, chicken, avocados and mushrooms.
Physical examination showed normal growth indicators according to World Health Organization standards. Although weight for age was "at risk" (-1.06 Standard Deviation) and length for age ratio showed weak impairment (-1.89 Standard Deviation), they were "normal-compensated" relative to weight for length (0.85 SD) and head circumference for age (0.55 SD).
Upon admission to GNP eosinophilic proctocolitis was suspected due to the history of rectal bleeding combined with the family history of allergies. On the other hand, symptoms such as dysphagia, choking crisis and spitting led us to suspect GERD with esophagitis or eosinophilic esophagitis.
Management with extensively hydrolyzed formula and continued breastfeeding began. Elimination of allergens that had already been started by the mother was continued under strict guidance of a clinical nutritionist.
The patient was evaluated again at a month and 14 days of age, 20 days after the first visit. There had been no new episodes of rectal bleeding, and vomiting and suffocation crises had lessened, but episodes of dysphagia associated with dyschezia persisted. Mixed breastfeeding with a restrictive diet and extensively hydrolyzed formula continued, Administration of 6 mg/kg/day of an anti H2 antagonist and domperidone was begun (administered by the mother). Upon physical examination, dermatitis was evident on the ears. On the other hand, good weight-height evolution, with obvious progress in the both weight and length growth rates was observed (W/H (-0.75 SD) and W/L (-1.17 DE)). Parameters for the weight-length ratio (0.56 SD) and head circumference-age (0.90 SD) continued to be within the normal range.
Notwithstanding the foregoing, due to the dermatitis and persistent vomiting, the improvement was considered to be partial. It was decided to observe the patient's evolution to determine whether it warranted switching to a formula based on L-amino acids and also to decide on whether or not to perform an endoscopic study.
During the third check-up at 2 months and 15 days, the patient's stools still contained mucus but were without blood. There were no signs of perianal erythema. After the parents told of increased regurgitation, the anti H2 antagonist was replaced by a proton pump inhibitor (PPI) which was administered by the attending pediatrician through house calls. This was done despite the mother's comment that it was not advisable to administer proton pump inhibitors to children under 1 year of age.
The mother decided to suspend breast feeding, and the patient continued to be fed with extensively hydrolyzed formula. The anthropometric assessment showed continued improvement in weight (WH: - (0.66 SD) LH: (-1.18 SD), WL: (0.52) SD, PC: (0.97) SD). Given the patient's adequate anthropometric evolution, adequate rate of growth associated, and the absence of other symptoms, and considering that gastroesophageal reflux was the only physiological symptom, the PPI was suspended while domperidone was continued for management of vomiting.
The baby had another check-up at 4 months and 21 days. The parents explained that the child had very dry skin, erythematous plaque on the scalp and recurrent vomiting. For these reasons, the attending physician had changed the extensively hydrolyzed formula to a formula based on L-amino acids two weeks before the check-up at GNP. The check-up showed an altered sleep pattern, Bristol 6 like stools with persistence of mucus but no blood, excessive flatulence and perianal erythema. As a consequence of the worsening symptoms, especially increased episodes of vomiting, the mother restarted the PPIs.
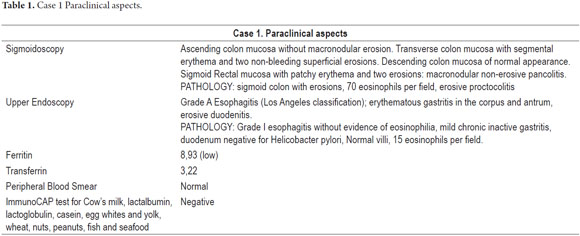
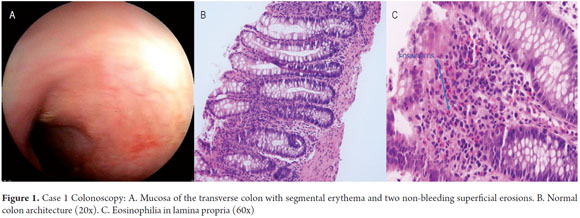
Considering the child's clinical course, it was decided to perform an upper endoscopy and a colonoscopy, and to order various laboratory tests including a complete blood count, ferritin, transferrin, ImmunoCAP testing for food allergies. Management, was continued with L-amino acids based formula, PBI and domperidone (Table 1 and Figure 1).
Eosinophilic proctocolitis with evidence of erosive proctocolitis was documented through colonoscopy and a blood test which showed an eosinophil count of 70 per field at high power. For this reason management with L-amino acid based formula continued. However, as inflammation persisted after the formula had already been used for some time, it was decided to begin administering 0.5 mg of prednisolone per day for 4 weeks. The upper endoscopy showed esophagitis, erythematous antral gastritis and duodenitis. Administration of the PPIs continued.
After beginning of treatment with steroids, the patient's skin lesions improved, and his stools changed from Bristol 6 to Bristol 4 without blood and notably without mucus. His perianal erythema improved as well. Steroids were slowly reduced until they were completely suspended at the end of the four week period. At 6 months of age, complementary feeding free of major food allergens began.
Good progress was evident at the next check-up when the child was 9 months and 9 days old. Anthropometric parameters were within the normal range (W/H: -1.07 SD; L/H: -0.85 SD, W/L: -0, 8, and PC/H: +1.87 SD) and the child was tolerating his progression to complementary feeding.
The patient's favorable progress continued into his first year of life. Management with L-amino acid based formula and progression of complementary feeding continued.
According to global allergy management protocols, a challenge to cow's milk was performed, and the child tolerated the challenge adequately. The family did not return for additional check-ups.
Case 2
An infant boy, 2 months and 18 days old, was brought to GNP by his family because of diarrhea.
At 5 days old, the child presented a clinical picture consisting of type 7 liquid stools about 12 to 13 times per day. They suspended breast feeding and initiated management with partially hydrolyzed low-lactose infant formula. At one month and 10 days, rectal bleeding began. A stool examination showed yellow color, blood +, mucus + +, pH 7, negative reducing sugars, and 2 to 4 erythrocytes per field. They decided to repeat the exam; the new exam showed: yellow color, mucus + +, pH 6, fecal fat + + +, leukocytes: 1 to 2 per field, and 0 to 2 erythrocytes per field. Suspecting an allergy to cows milk protein, they replaced the partially hydrolyzed formula with an extensively hydrolyzed formula and treatment with ampicillin began. Since the child rejected the formula, the family began to prepare a formula with water, roasted rice and guava. According to the family, this enhanced acceptance but led to rectal bleeding and increased stool frequency. Later, it was restarted, and the patient began to have watery stools with mucus. A new stool culture was negative. Pharmacological treatment with zinc sulfate and probiotics was added to the child's treatment.
It is worth noting that this child is the product of a first pregnancy and a cesarean delivery at 39 weeks. His weight and length were adequate at birth, he defecated his meconium within his first 24 hours of life, and three is a family history of allergic rhinitis in both parents and the maternal grandmother.
During the first consultation at GNP, the physical examination was normal, and the child exhibited good general anthropometric parameters (W/H: -0.01 SD, L/H: -0.98 SD, W/L +1.14 SD); PC/H: 0.09 SD).
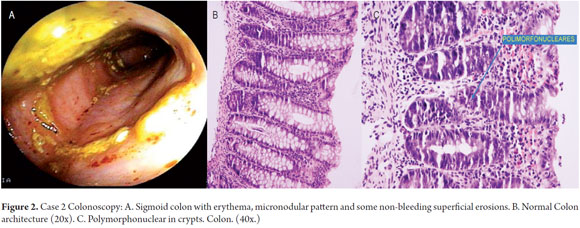
According to the clinical course of the patient, proctocolitis was suspected, and it was decided to perform colonoscopy. In the process, rectosigmoid mucosa with erythema, a nodular pattern and some superficial non-bleeding erosions were observed. After the colonoscopy, due to the finding of inflammation it was decided to start L-amino acid based formula even though the patient was already receiving extensively hydrolyzed formula.
At a check-up 6 days after the initial assessment, when the child was 2 months and 24 days old, the family reported that stool frequency had decreased to once daily which confirmed the suspected diagnosis of allergic proctocolitis. The report histopathology report also showed, «moderate acute erosive proctocolitis», 5 eosinophils per field, exocytosis and polymorphonuclear leukocyte infiltration (See Figure 2). Although eosinophilic infiltration was not confirmed with the eosinophil high power field count, the L-amino acid based formula was continued because of the improvement in the number and appearance of stools (Bristol 7 without mucus).
At the next check-up when the child was 5 months and 24 days old, the child's evolution was observed to be favorable with normal stools. It was decided to start complementary allergen-free feeding under the guidance of a clinical dietitian.
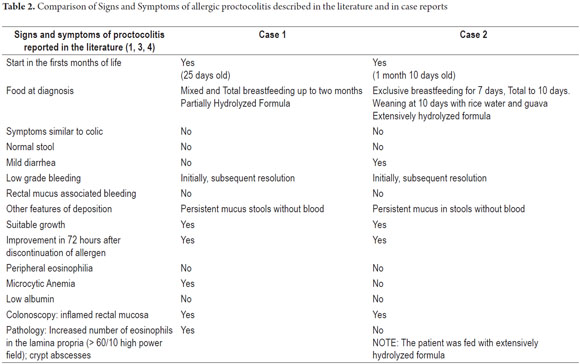
At 13 months of age, the child was brought back for another check-up. Again, favorable evolution was observed with dietary transgressions with cow's milk protein. On physical examination, good growth development was observed (WH: 0.35 SD, LH: -0.19, WL: 0.56, PCH: -0.30 SD). Therefore, it was considered appropriate to try a cow's milk protein challenge which was successfully performed with good tolerance to the protein in cow's milk. (See Table 2).
DISCUSSION
Eosinophilic proctocolitis is a gastrointestinal manifestation of food allergies not mediated by IgE. It was first described several years ago, but continues to generate concerns. It is described as "inflammatory changes in the rectum and colon as a result of ingesting protein antigens such as cow's and soy milk and is associated with rectal bleeding. It improves with elimination within the first 72 hours." Furthermore, it is self-limiting and most patients will have adequate weight-height development and will not be not anemic (7, 8, 9, 18).
Nevertheless, a small group of patients with mild, usually transient, rectal bleeding, which is not the main symptom have also been described. The two cases reported above are consistent with this. They had persistent stools with mucus or watery stools accompanied by mucus with no bleeding as the primary symptom (7, 10).
The incidence of eosinophilic proctocolitis has been increasing. It is due in part to the decline of breastfeeding and the more frequent use of infant formula (6). Nevertheless the two cases described were both exclusively breastfed when the disease appeared which may indicate sensitization to food allergens ingested by the mothers and transferred through breast milk. This kind of sensitization may worsen if milk and/or soy protein based formulas are initiated.
At the Unit of Gastroenterology Hepatology and Nutrition - Gastronutriped - there were 50 patients with confirmed eosinophilic proctocolitis among children diagnosed with food allergies between 2010 and 2013. 57% of these patients were male. Only the two cases detailed in this article had persistent atypical intestinal disorders with stools with mucus as the predominant symptom.
In both cases, extensively hydrolyzed formulas were tried and then replaced with L-amino acid based formulas which resulted in progressive improvement. Dupont suggests that up to 10% of children with allergies to cows milk protein do not thrive on protein hydrolysates, but do thrive on elemental formula which is evidenced by absence of gastrointestinal or extra-intestinal symptoms secondary to allergy and by increased weight (11).
In both cases described, torpid progress with diets restricted to breast feeding and extensively hydrolyzed formulas was observed. This indicated colonoscopies for differential diagnoses. Pathology reports documented eosinophilia in the lamina propria (More than 60 eosinophils per field) associated with crypt abscesses and intraepithelial lymphocytes (predominantly CD8 +). Nevertheless, the significance of the eosinophil counts remains inconclusive because there is no consensus yet on the normal value of eosinophil counts. Some reviews suggest that 5 to 35 per field is normal (12). In Case One, the count of eosinophils per high power field was greater than sixty, confirming the disease. In Case 2, a lower count was observed but with high levels of polymorphonuclear infiltrates which is likely to have been secondary to the use of extensively hydrolyzed formula prior to the procedure. The good response to the L-amino acids formula supports the conclusion that the excessive mucus in their stools was due to persistent proctocolitis.
Close monitoring of patients was the basis for determining whether or not there were subtle changes with improvement or deterioration of clinical presentation.
Some GNP patients who have severe proctocolitis have not responded to restriction of allergens and required have oral administration of low-dose systemic corticosteroids. Outcomes have been favorable outcome, as in the first case reported above. Among the 50 patients diagnosed with eosinophilic proctocolitis, three patients needed corticosteroids. They were given between 0.5 mg/day and 1 mg/kg/day which achieved complete resolution of symptoms in all three patients. The use of steroids for eosinophilic proctocolitis is not clearly indicated in the current literature which discusses steroid treatment for colitis and proctocolitis resulting from etiologies other than allergies. Lucendo proposes the use of budesonide because it acts on the small intestine and colon when dietary restrictions are insufficient to achieve improvement (13). The scarcity of related research indicates a need for controlled studies of this issue (14).
Although there is no reported experience in their use for managing proctocolitis, other medications that have been mentioned as potential treatments are are cromoglycate, montelukast and histamine receptor antagonists (15). For those patients who do not improve, it is essential to consider differential diagnoses of such pathologies as bacterial gastroenteritis, anal fissures, intestinal intussusception, juvenile polyps and other non-allergic forms of colitis such as granulomatous disease or inflammatory bowel disease. While they do not occur frequently, they should be taken into account (3).
At GNP it has been observed that some children with allergic proctocolitis have difficulty progressing to tolerance of new complementary foods when they are introduced. This occurs even with foods that are only very slightly allergenic (unpublished data). In some cases, newly introduced foods are withdrawn and the patient is given more time to reach the tolerance reported in the literature (15). Jacob reports the case of a four year old boy who had suffered from proctocolitis at 2 months of age. It was managed with dietary restriction of cows milk protein, but when the allergen was reintroduced two years later, gastrointestinal symptoms, especially bleeding, recurred.
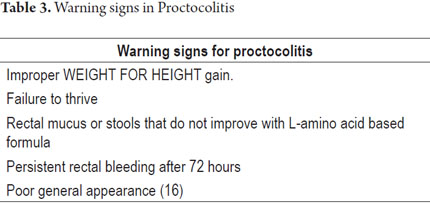
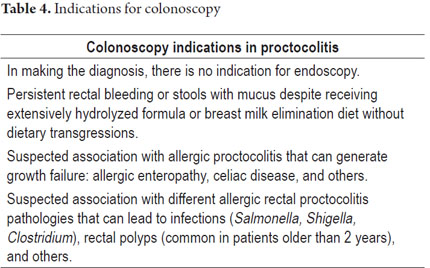
Taking all of the above into consideration, we want to underline the need for multidisciplinary teams including a pediatrician, a gastroenterologist, a nutritionist, an allergist, a speech and hearing specialist, a psychologist and a social worker, and the need for diligent monitoring of the patient´s symptoms and growth. (See Table 3 and Table 4).
CONCLUSION
Eosinophilic or allergic proctocolitis, is one of the earliest manifestations of food allergies. It has been described as a benign disease whose main clinical manifestations are rectal bleeding and mucus in the stool. However, it is worth noting that in addition to bleeding and mucus in the stool other equally transcendent and evocative symptoms exist such increased frequency and stool consistency. These manifestations may be obviated by the absence or persistence of enterorrhagia which can result in a delay in the necessary change of the approach. Such delays can make it very difficult difficulty to resolve the inflammatory process which can increase the amount of time required to reach tolerance of the triggering allergen and which can also promote sensitization to other allergens during the introduction of complementary feeding.
REFERENCES
1. Fiocchi A, Schünemann HJ, Brozek J, Restani P, Beyer K, Troncone R, et al. Diagnosis and Rationale for Action Against Cow's Milk Allergy (DRACMA): a summary report. J Allergy Clin Immunol. 2010;126(6):1119-1128.e12. [ Links ]
2. Koletzko S, Niggemann B, Arato A, Dias JA, Heuschkel R, Husby S, et al. Diagnostic approach and management of cow's-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr. 2012;55(2):221-9. [ Links ]
3. Heine RG. Pathophysiology, diagnosis and treatment of food protein-induced gastrointestinal diseases. Curr Opin Allergy Clin Immunol. 2004;4(3):221-9. [ Links ]
4. Yu M-C, Tsai C-L, Yang Y-J, Yang S-S, Wang L-H, Lee C-T, et al. Allergic colitis in infants related to cow's milk: clinical characteristics, pathologic changes, and immunologic findings. Pediatr Neonatol. 2013;54(1):49-55. [ Links ]
5. Wolfe JL, Aceves SS. Gastrointestinal manifestations of food allergies. Pediatr Clin North Am. 2011;58(2):389-405, x. [ Links ]
6. Atkins D, Furuta GT. Chapter 10 - Eosinophilic Gastroenteropathies (Eosinophilic Esophagitis, Eosinophilic Gastroenteritis and Eosinophilic Colitis). En: James JM, Burks W, Eigenmann P, editores. Food Allergy [Internet]. Edinburgh: W.B. Saunders. 2012; 129-41. [ Links ]
7. Odze RD, Wershil BK, Leichtner AM, Antonioli DA. Allergic colitis in infants. J Pediatr. 1995;126(2):163-70. [ Links ]
8. Simon D, Wardlaw A, Rothenberg ME. Organ-specific eosinophilic disorders of the skin, lung, and gastrointestinal tract. J Allergy Clin Immunol. julio de 2010;126(1):3-13; quiz 14-15. [ Links ]
9. Academy of Breastfeeding Medicine. ABM Clinical Protocol #24: Allergic Proctocolitis in the Exclusively Breastfed Infant. Breastfeed Med Off J Acad Breastfeed Med. 2011;6(6):435-40. [ Links ]
10. Troncone R, Discepolo V. Colon in food allergy. J Pediatr Gastroenterol Nutr. 2009;48 Suppl 2:S89-91. [ Links ]
11. Dupont C, de Boissieu D. [Treatment of severe cow's milk protein allergy using Neocate]. Allerg Immunol (Leipz). 2002;34(3):85-90. [ Links ]
12. Lowichik A, Weinberg AG. A quantitative evaluation of mucosal eosinophils in the pediatric gastrointestinal tract. Mod Pathol Off J U S Can Acad Pathol Inc. 1996;9(2):110-4. [ Links ]
13. Lucendo AJ. Eosinophilic diseases of the gastrointestinal tract. Scand J Gastroenterol. 2010;45(9):1013-21. [ Links ]
14. Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004;113(1):11-28; quiz 29. [ Links ]
15. Jacob CMA, Pitarello DLA, Pastorino AC, Trevisan MMF, Koda YL, Vidolin E, et al. Allergic Proctocolitis Associated With Cow's Milk With An Unusual Evolution. J Allergy Clin Immunol. 2007;119(1):S123-S123. [ Links ]











 texto em
texto em