Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.2 Bogotá Apr./June 2014
Perforations Occurring during ERCP: A Complication to Take into Account
Martín Alonso Gómez Zuleta, MD. (1), David Andrés Viveros Carreño, MD. (2)
(1) Gastroenterology Unit at the Universidad Nacional de Colombia and Gastroenterologist at Hospital El Tunal in Bogotá, Colombia.
(2) Hospital El Tunal in Bogotá, Colombia.
Received: 16-11-13 Accepted: 08-05-14
Abstract
When it was introduced 40 years ago, endoscopic retrograde cholangiopancreatography (ERCP) was used to diagnose biliopancreatic diseases. Nevertheless, because of its risks, it has been used only for therapeutic procedures for more than 10 years. It is very useful for handling various biliopancreatic pathologies, but like most endoscopic procedures, ERCP is not without potential risks, and the rate of complications is around 5% to 7 %. Perforations are one of the most feared complications because early diagnosis is very difficult and because they can result in death. We present clinical cases of this type of diagnosis that have been managed in our hospital together with a review of the literature.
Keywords
Perforation, endoscopic retrograde cholangiopancreatography, ERCP.
INTRODUCTION
Since the introduction of endoscopic retrograde cholangiopancreatography (ERCP) in 1968 (1), it has become an indispensable endoscopic procedure in the practice of gastroenterology. Its therapeutic usefulness for treating a wide range of pathologies is especially important; it can be used to treat choledocholithiasis and biliopancreatic neoplasia as well as complications following surgery (2).
Like most ERCP procedures it is not without potential complications. Complication rates reported in the literature vary widely due to differences in study design, study populations and definitions for complications. In larger studies complication rates are around 5-7% (3-5). Even though the frequency of its performance has declined, and the indications for its realization have improved (6), complications still remains a common problem.
Complications can be classified into those that can occur in any endoscopic procedure and those that are specific tor ERCP. Among the latter, pancreatitis is the most common followed by hemorrhaging, perforations, biliary tract infections and systemic complications (mainly cardiopulmonary complications) (2, 7).
The following are clinical cases in our institution which presented complications, their diagnosis and treatment.
CLINICAL CASE 1
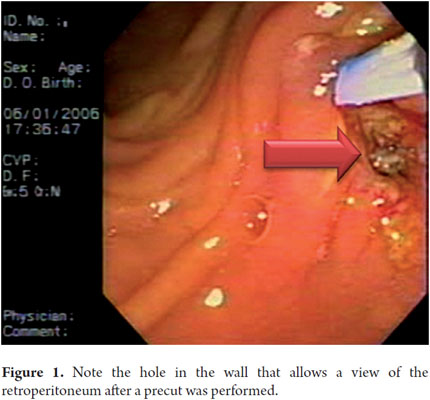
A 67 year old woman underwent ERCP because of suspected choledocholithiasis. Cannulation was not possible, therefore a pre-cut was done. A retroperitoneal perforation was found. We tried to cannulate the bile duct with the papillotome, but only a distal hole which extended to the retroperitoneum could be glimpsed (Figure 1). Due to a high suspicion of perforation, the procedure was suspended. Two hemoclips were used to close the perforation and medical treatment with antibiotics and intravenous fluids was begun through a nasogastric catheter. The clinical outcome was good.
CLINICAL CASE 2
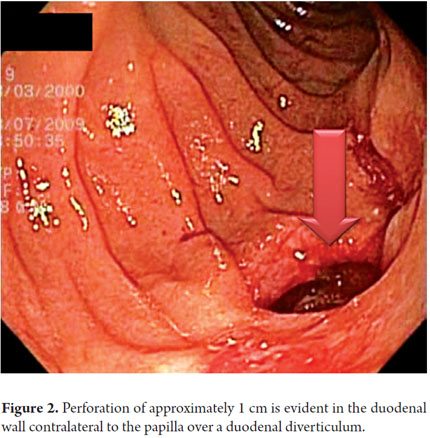
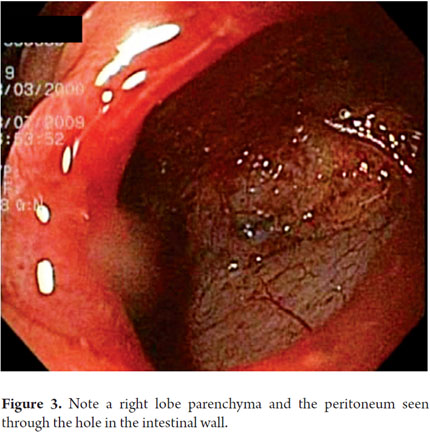
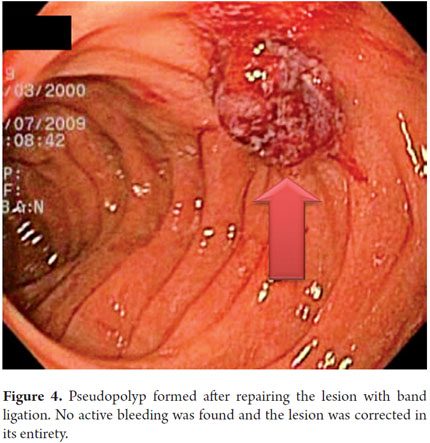
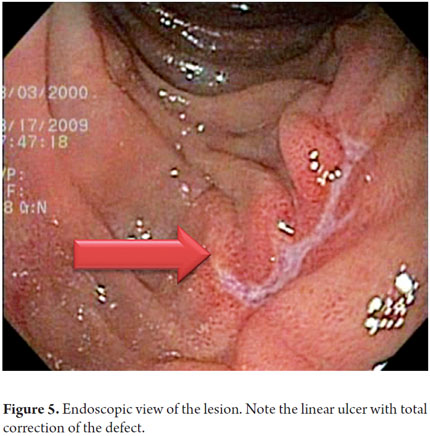
A 64 year old woman with residual choledocholithiasis developed jaundice 15 days after a cholecystectomy. An ERCP was performed. While rectifying the equipment, a diverticulum located diagonal to the papilla was perforated. A papillotomy and stone extraction was rapidly performed. The frontal endoscope showed a 1 cm perforation of a duodenal diverticulum that was on the wall contralateral to the papilla (Figure 2). The proximal part showed the laceration produced by the duodenoscope before the perforation. Images show the peritoneum lining the intestine and the right lobe of the liver (Figure 3). Since the perforation was rapidly detected, it only measured one inch, and its edges were regular. It was decided to close it with a ligation band. After ligation, a pseudo-polyp formed and complete closure of the perforation was achieved (Figure 4). Radiological studies performed after the procedure showed a large area of subcutaneous emphysema, but the patient had a favorable clinical outcome. Ten days later an endoscopic follow-up showed full closure of the perforation with only a linear ulcer left (Figure 5). This is the first case ever reported in literature anywhere in the world of successful closure with a band.
CLINICAL CASE 3
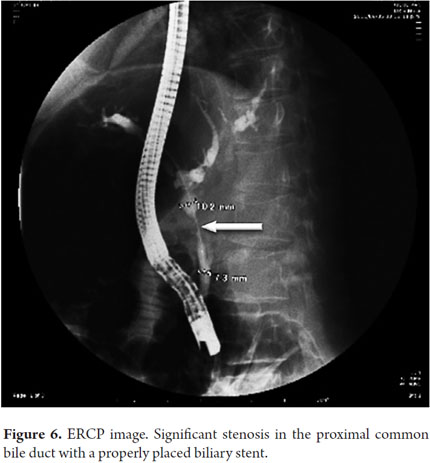
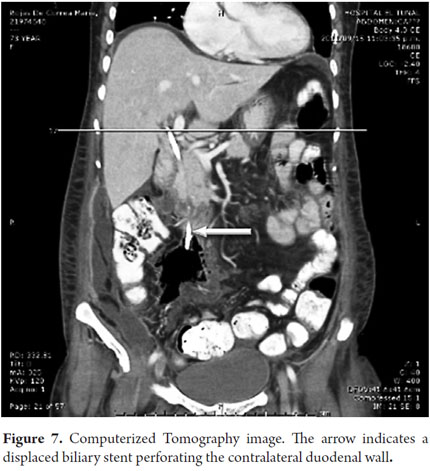
A 72 year old patient with obstructive jaundice and evident weight loss underwent ERCP. Because the procedure revealed an image suggestive of cholangiocarcinoma, a 10 F Stent (12 cm) was used for drainage with excellent results included decreased jaundice. ERCP scans showed a stenosis in the proximal bile duct, so a stent that was placed there (Figure 6). The patient had an excellent outcome until seven days later when she experienced severe abdominal pain and increased jaundice. An abdominal CT scan showed distal stent migration resulting in contralateral perforation of the duodenal wall. Intra-abdominal gas (Figure 7) was also observed. The patient underwent emergency surgery after which she was admitted to the ICU but her evolution was torpid, and she died.
CLINICAL CASE 4
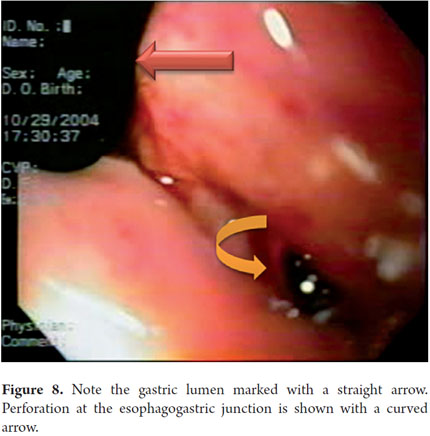
A 70 year old patient with suspected choledocholithiasis began to undergo ERCP, but when the duodenoscope was introduced and positioned in front of the papilla, severe oxygen desaturation occurred. At this point the procedure was suspended. A chest x-ray showed a right pneumothorax. Since the patient remained unstable from a cardiovascular point of view, she was sent to surgery.
Prior to surgery, it is decided to perform an endoscopy to rule causes of spontaneous pneumothorax other than a bulla rupture which was suspected. An esophageal perforation was found at the angle of His in the gastroesophageal junction (Figure 8).
Perforations occur during ERCP at rates ranging from 0.1% to 0.6% according to various studies (3, 4, 8, 9). Perforations can be defined as the presence of air or contrast in the retroperitoneal space or a clinical picture compatible with any normal intestinal perforation (4). Despite being a rare complication of this procedure, the importance of perforations lie in the morbidity and mortality rates. Mortality rates can be as high as 20%, especially for patients in which the perforation is diagnosed late, for whom surgery is required and who have long hospital stays (8).
Perforations usually occur in elderly patients. In some studies they are more common in women and in procedures that are difficult to perform (9, 10). The first characteristic may be associated with the increased frequency of the procedure in this population.
There are several classifications of perforation that are used, but they can be divided into three types (Figure 9) (11).
Type 1
Perforations caused by guide wire or basket. These are produced by the inadvertent passage of the guide wire or another instrument outside the biliary or pancreatic duct. This perforation is usually small and does not have great consequences. Most of the time we do not even realize that it has happened, and it heals spontaneously (8).
Type 2
Periampullar and retroperitoneal perforations are the most common. They occur because the papillotomy extends beyond the mural portion of the papilla or because a pre-cut is too deep (8). There are two major risk factors for this complication: Billroth II reconstruction and dysfunction of the sphincter of Oddi. It is also more common when performing a papillotomy with precut, as in the case report presented above, than with conventional papillotomies (7, 8). This can be diagnosed when there is extravasation of contrast to the retroperitoneum or the presence of free air. Treatment is to leave suspend oral feeding, feed the patient by through a nasogastric tube, and administer a broad-spectrum antibiotic. This leads to satisfactory results in the majority of patients (8).
Type 3
Perforations distal from the periampullary region tend to occur in patients with anatomic abnormalities such as the duodenal diverticula in our case presented above (9). Treatment is always surgical (8, 10), although there are endoscopic treatment option depending on the characteristics of each case. Diagnosis during the procedure is difficult because these perforations occur in the lateral wall of the duodenum where the viewing angle of the duodenoscope does not usually any view of the area (8).
Finding perforations and administering proper treatment can result in clinical resolution even without the need for surgical treatment in most patients. Unfortunately, diagnosis during the procedure is not common (8). The result is the subsequent use of radiological tools for diagnosis. The main clinical manifestations are the presence of abdominal pain, sometimes associated with abdominal distention. Leukocytosis and fever may be found when the perforation is diagnosed late (8).
A simple abdominal x-ray is the first step when there is clinical suspicion of perforation. Absence of intra-peritoneal air and the presence of retroperitoneal air are the only indicators of a controlled or sealed perforation. In these cases medical intervention with bowel rest, nasogastric tube decompression and broad-spectrum antibiotics is recommended (8, 10). In patients with no positive findings and clinical suspicion, CT scans and contrast images are useful because they can detect small volumes of gas (8, 9).
Treatment of a perforation depends on many factors including the site and location of the lesion, the clinical status of the patient, and diagnostic images (8-10). Treatment usually requires joint management by the surgical team. Patients who benefit from surgery require drainage of retroperitoneal or intra-abdominal collections, removal of calculi and the repair of the perforation with or without an intestinal bypass (8).
CONCLUSIONS
ERCP is a very useful procedure. Complications may be unavoidable, but we must try to reduce them as much as possible and recognize them early to improve outcomes. Endoscopic treatment of some lesions is possible and can reduce the morbidity and hospital stays of patients.
REFERENCES
1. McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167(5):752-6. [ Links ]
2. Complications of ERCP - 076fbf43-9959-4859-8286-bc62fec2b5dc.pdf [Internet]. [citado 4 de junio de 2014]. Recuperado a partir de: http://www.asge.org/assets/0/71542/71544/076fbf43-9959-4859-8286-bc62fec2b5dc.pdf [ Links ]
3. Wang P, Li Z-S, Liu F, Ren X, Lu N-H, Fan Z-N, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104(1):31-40. [ Links ]
4. Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96(2):417-23. [ Links ]
5. Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102(8):1781-8. [ Links ]
6. Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 26 de septiembre de 1996;335(13):909-18. [ Links ]
7. Barkay O, Khashab M, Al-Haddad M, Fogel EL. Minimizing complications in pancreaticobiliary endoscopy. Curr Gastroenterol Rep. 2009;11(2):134-41. [ Links ]
8. Avgerinos DV, Llaguna OH, Lo AY, Voli J, Leitman IM. Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc. 2009;23(4):833-8. [ Links ]
9. Kim J, Lee SH, Paik WH, Song BJ, Hwang JH, Ryu JK, et al. Clinical outcomes of patients who experienced perforation associated with endoscopic retrograde cholangiopancreatography. Surg Endosc. 2012;26(11):3293-300. [ Links ]
10. Miller R, Zbar A, Klein Y, Buyeviz V, Melzer E, Mosenkis BN, et al. Perforations following endoscopic retrograde cholangiopancreatography: a single institution experience and surgical recommendations. Am J Surg. 2013;206(2):180-6. [ Links ]
11. Howard TJ, Tan T, Lehman GA, Sherman S, Madura JA, Fogel E, et al. Classification and management of perforations complicating endoscopic sphincterotomy. Surgery. 1999;126(4):658-663; discussion 664-665. [ Links ]
12. Lee TH, Han J-H, Park S-H. Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations. Clin Endosc. 2013;46(5):522-8. [ Links ]











 text in
text in