Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.2 Bogotá Apr./June 2014
A Case Report of Pulmonary and Lingual Tuberculosis
Rafael Pila Pérez, MD. (1), Víctor Adolfo Holguín Prieto, MD. (1), Rafael Pila Peláez, MD. (1), Pedro Rosales Torres, MD. (1), Danay Caballero Hernández (1)
(1) Department of Internal Medicine at the Hospital Universitario "Manuel Ascunce Domenech" in Camagüey, Cuba.
Received: 19-02-14 Accepted: 08-05-14
Abstract
Objective: The objective of this study is to present a rare case of secondary lingual tuberculosis (TB). This was the first reported occurrence of this disease in the hospital and in the province in 50 years.
Case report: A 69 year old male patient who had been hospitalized twice because of bacterial pneumonia acquired in the community was admitted to the hospital. For three weeks prior to admission the patient had suffered fever, dry irritating coughing, constitutional symptoms, 0.5 to 1.0 cm nodular lesions on the dorsum of the tongue, and canker sores at the base of the tongue. As a result the patient had been unable to eat. Two acid fast bacilli (AFB) smears both showed a rating of 9. Tuberculosis testing, x-rays and histology confirmed the diagnosis. Tuberculosis treatment was begun. After two months the nodules disappeared. The patient remained asymptomatic and continues to be monitored on an outpatient basis.
Conclusions: TB of the tongue is a rare finding that should be included in the differential diagnosis of diseases of the oral cavity. This case demonstrates the importance of continued vigilance of this entity in medical and dental practice.
Keywords
Pulmonary tuberculosis, diseases of the tongue, granulomatous diseases.
INTRODUCTION
Today tuberculosis (TB) is a curable disease. Its prevalence decreased significantly after the introduction of streptomycin and polychemotherapy, but the problem has not been completely solved problem, and it has reappeared in a spectacular manner forcing doctors to keep it in mind not only when faced with lung diseases but also when diagnosing and treating symptoms located in various other organs.
This entity is a chronic, systemic bacterial infection that most often affects the lungs. Nevertheless, it can compromise, in order of frequency, the kidney, lymph nodes, liver, nervous system, and bones. The decline in TB has not been followed by a decrease in the number of extrapulmonary sites, but has been shown accompanied by decreased morbidity and mortality (1).
Oral manifestations of TB are extremely rare. With an incidence of 14%, the tongue is the least common location in this area, but it has a variety of presentations (2). Lingual TB is a diagnostic dilemma particularly because of its rarity, especially its presentation in immunocompetent patients (2, 3).
The aim of this paper is to present the case of a patient with pulmonary and lingual TB. This was the first case diagnosed in Camagüey in the last 50 years.
CASE REPORT
A 69 year old male patient had come to the hospital twice with a diagnosis of community-acquired bacterial pneumonia. The patient was a smoker without family history of interest. Three weeks before admission to the hospital, he developed a fever accompanied by night sweats, a dry irritating cough, asthenia, anorexia and weight loss (10 kg in 2 months). In the three days prior to admission he noticed pain in his tongue radiating to the right ear. The pain was accentuated by chewing and made eating difficult.
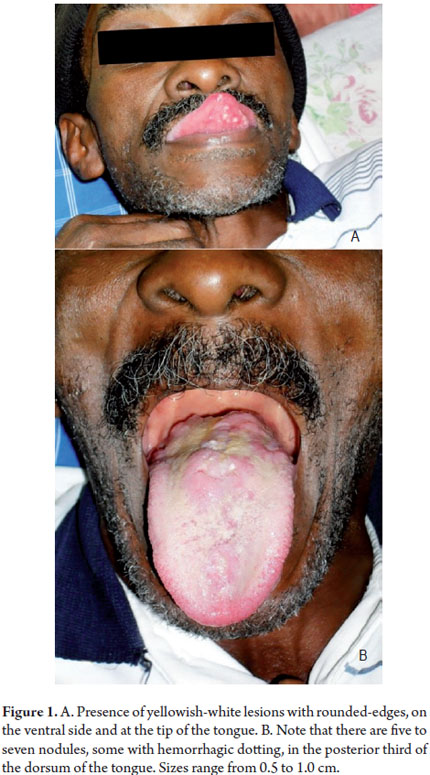
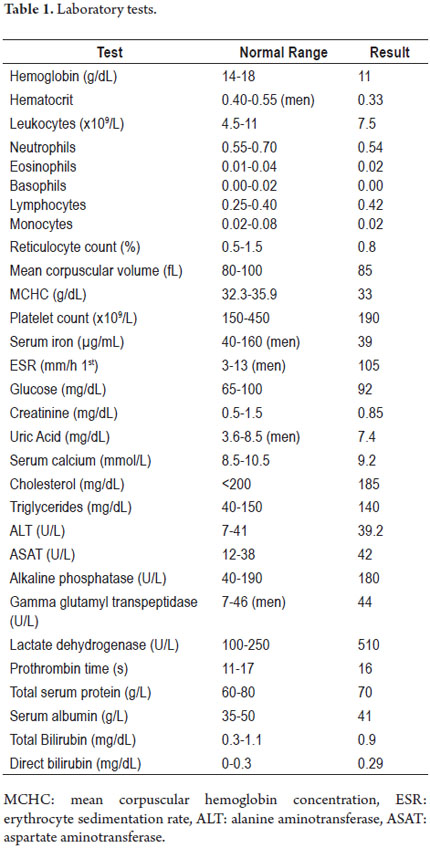
Physical examination: The patient's vital signs were as follows: respiratory rate - 28/min, central heart rate - 100 beats/ minute, blood pressure - 110/70 mmHg. His general condition had deteriorated. He was feverish and had a temperature of 39 ° C. There were no alterations in his skin nor palpable lymphadenopathy in any lymph node chain. Cardiopulmonary examination revealed a globally decreased vesicular wheeze with scattered crackles in both lungs especially in the upper 2/3 of the left lung. The patient had tachycardia and rhythmic heart murmurs. In the oral cavity (Figure 1) five to seven nodular lesions were found in the posterior third of the dorsum of the tongue. The lesions were soft and painful and measured between 0.5cm and 1 cm. They were infiltrated and had some bleeding dots at the base of the tongue. Six to seven aphthous ulcers were observed at the tip of the tongue. They were yellowish-white with rounded-edges and measured 0.3mm to 0.6 mm. No abnormalities were found in other organ systems.
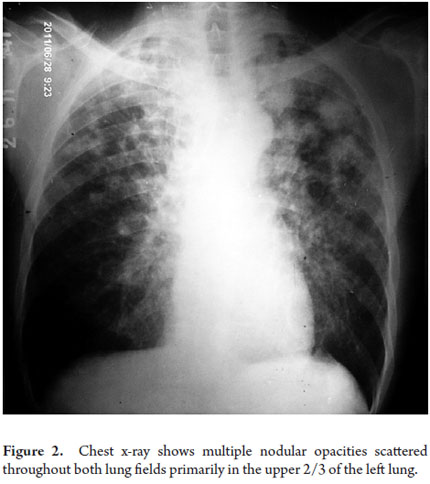
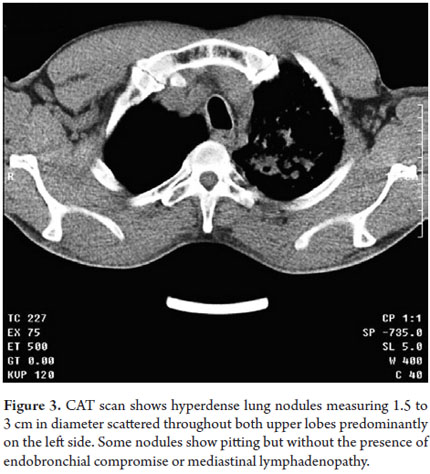
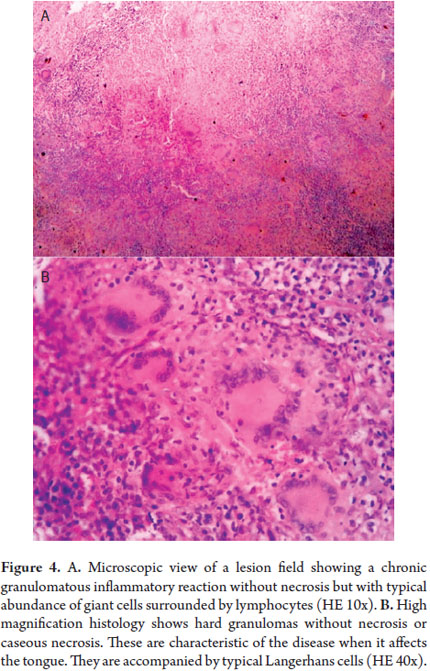
Clinical Studies: Analytical studies are presented in Table 1. Serological studies for VDRL, HIV, HVB antigens and HVC antigens were negative. Blood cultures were negative. A chest x-ray showed multiple nodular opacities scattered throughout both lung fields especially in the upper 2/3 of the left lung (Figure 2). A CAT scan of the lungs showed hyperdense nodular lesions measuring 1.5cm to 3 cm in diameter scattered in both upper lobes but predominantly in the left lobe. Some of these nodes showed a tendency to cavitation (Figure 3). Faced with the possibility of lung tuberculosis, the patient was tested with the Mantoux method and an AFB smear (TB). An induration of 16 mm was shown by the Mantoux method, and the AFB smear coded 9 in to 2 chances. A tongue biopsy (Figure 4) showed a granulomatous inflammatory process consistent with lingual TB. Sputum culture and histological samples tested with Lowenstein-Jensen confirmed the growth of Mycobacterium tuberculosis (Mycobacterium tuberculosis).
The patient was diagnosed as having pulmonary TB with secondary lingual compromise. Management began with polychemotherapy according to the National Program for TB management. At eight weeks the disappearance of oral lesions was observed, and there was marked improvement of the patient's radiological and clinical picture. The patient has continued regular checkups as agreed for this disease.
DISCUSSION
Oral manifestations of TB are rare (4) because saliva continuously acts on the bacilli and prevents it from depositing on oral tissue (5). When bacilli achieve penetration of the mucosa, they are phagocytized and incorporated into the circulation without causing oral lesions (4). The mucosa is not environmentally suitable for development of mycobacterium tuberculosis (6). The clinical characteristics of TB in the mouth can be primary (rare) or secondary (much more common) infections (4, 6, 7). The gums are most frequently affected by primary infections, followed by the oropharynx (6, 7). Nevertheless, the parotid can also be affected (8, 9). Secondary forms are mainly located on the tongue (5).
Children and young adults are most likely to be affected especially because of immunosuppression and the association shown by some studies with HIV/AIDS (3). A study in India of 212 children with HIV found that 132 of them (62.26%) presented oral lesions, and TB was reported as a systemic disease in 49.1% (3). Thirty- three patients (26%) did not show immunosuppression, 74 (58%) had moderate immunosuppression, and 20 (15%) had severe immunosuppression. In all cases it was shown that oral lesions correlated with lesions elsewhere in the body (3, 8, 9).
In contrast, the case reported here is a 69 year old patient with no history of any primary or secondary immunosuppression.
In primary oral TB, lesions occur most commonly in the form of ulcers which appear pitted and are surrounded by edematous areas (2, 8, 9, 11). The edges of these ulcers bleed but heal spontaneously after 10 to 20 days (5, 10). Their sizes vary, but they average 2 to 3cm in diameter. They are whitish with a regular background and are usually located at the front and on the ventral surface of the tongue (13). When TB occurs in the nodular form, the clinical course is more persistent and painful. In these cases there is painless cervical lymphadenopathy which subsequently can form abscesses and open to the skin. They discharge a necrotic material (4). Lymphadenopathy may suggest malignancy (12).
Oral TB and lesions in other organs or other areas of the eye, nose and throat region are more common in secondary infections although they usually originate in the lungs (4). In these cases, the lesions occur by direct infection of the mycobacteria from the sputum when a previous mucosal lesions allows infection or by transmission through the blood or lymph (5, 14). The most frequent site for tubercular ulcers and nodules is on the back of the tongue. Ulcers are resectable, non-adherent, soft, and usually painful. Pain is exacerbated during chewing and typically radiates to the ear. Lesions are rounded so that when cleaned they show yellowed corpuscles and bleeding points. These corpuscles are called yellow beans or Trélat signs (5, 10, 13). They are usually accompanied by cervical lymphadenopathy.
The patient reported on here had a form of secondary tuberculosis with lingual compromise without ulcers, but with quite a few painful nodules on the dorsal surface of the tongue. He also presented thrush on the ventral side. This is a truly unusual finding not found in the literature reviewed. Adenopathy was never evident in any of the explored node chains.
The patient's oral condition and clinical, radiological and endoscopic signs are nonspecific (6-8). Usually the diagnosis is made by histopathology that differentiates among granulomatous and neoplastic diseases (9). A biopsy of the lingual region shows chronic granulomatous inflammatory reaction suggestive of TB, as was seen in the study of one of the lingual nodules of this patient. When there is lymphadenopathy of the cervix or elsewhere, it can provide support for a diagnosis (12). However, it should be taken into account that sometimes the histopathology of the initial biopsy reveals only nonspecific inflammation (15). Excised tissue biopsy is essential for differential diagnosis. Other possible diagnoses which must be discarded include squamous tongue cancer, smoking, histoplasmosis in endemic areas (10), syphilis, traumatic lesions, aphthous ulcers (14), lymphomas and various bacterial infections (16). Polymerase chain reactions are also useful because of their high specificity in detecting genomic material of mycobacterium tuberculosis (8-10).
Although the diagnosis of lingual TB is a real clinical challenge, early identification is essential. Lesions can be completely healed with specific antimicrobial treatment for between two and eight months (9, 17). Some authors indicate six months despite lingual TB's association with other locations in the oral cavity, larynx and lung (18).
CONCLUSIONS
Because the lingual TB is so unusual, and since doctors rarely ever think of it as a possible cause of this clinical presentation, priority is given to other entities according to local epidemiology. This significantly delays diagnosis. In secondary forms, which are the most frequent, the lingual condition usually results from pulmonary and/or laryngeal TB. Smear-positive forms are remarkably important in the epidemiology of this reemerging disease.
REFERENCES
1. Pila Pérez R, Amador Betancourt J, Pernas Alvariño J, Alvarez Suárez G. Tuberculosis extrapulmonar: estudio de 97 casos. Rev Cuba Med. 1987;26(3):256-66. [ Links ]
2. Kumar S, Sen R, Rawal A, Dahiya RS, Dalal N, Kaushik S. Primary lingual tuberculosis in immunocompetent patient: a case report. Head Neck Pathol. 2010;4(2):178-80. [ Links ]
3. Ranganathan K, Geethalakshmi E, Krishna Mohan Rao U, Vidya KM, Kumarasamy N, Solomon S. Orofacial and systemic manifestations in 212 paediatric HIV patients from Chennai, South India. Int J Paediatr Dent Br Paedodontic Soc Int Assoc Dent Child. 2010;20(4):276-82. [ Links ]
4. Gharebaghi N, Monsouri SA, Darazam IA, Mansouri D, Sajadi MM, Mansouri N. A 40-year-old man with tongue lesions. Lingual and pulmonary tuberculosis (TB). Clin Infect Dis Off Publ Infect Dis Soc Am. 2011;52(10):1231, 1276-7. [ Links ]
5. Morán López E, Lazo Amador Y. Tuberculosis. Rev Cuba Estomatol. 2001;38(1):33-51. [ Links ]
6. Sharma AB, Laishram DK, Sarma B. Primary tuberculosis of tongue. Indian J Pathol Microbiol. 2008;51(1):65-6. [ Links ]
7. Hussaini J, Mutusamy S, Omar R, Rajagopalan R, Narayanan P. Base of tongue tuberculosis: a case report. Acta Med Iran. 2012;50(2):151-2. [ Links ]
8. El Ayoubi A, Benhammou A, El Ayoubi F, El Fahssi A, Nitassi S, Kohen A, et al. [Primary extranodal ENT tuberculosis]. Ann Oto-Laryngol Chir Cervico Faciale Bull Société Oto-Laryngol Hôp Paris. septiembre de 2009;126(4):208-15. [ Links ]
9. Furugen M, Nakamura H, Tamaki Y, Haranaga S, Yara S, Higa F, et al. [Tuberculosis of the tongue initially suspected of tongue cancer: a case report--including the search for recent 16 cases in Japan]. Kekkaku. 2009;84(8):605-10. [ Links ]
10. Hofman V, Selva E, Musso S, Odin J-C, Dellamonica P, Hofman P. [Tuberculosis: a rare and misleading etiology of tongue's ulcer]. Ann Pathol. 2003;23(3):261-5. [ Links ]
11. Garg RK, Singhal P. Primary tuberculosis of the tongue: a case report. J Contemp Dent Pract. 2007;8(4):74-80. [ Links ]
12. Sareen D, Sethi A, Agarwal AK. Primary tuberculosis of the tongue: a rare nodular presentation. Br Dent J. 2006;200(6):321-2. [ Links ]
13. Yiğit O, Cinar U, Uslu Coşkun B, Başak T. Tuberculous ulcer of the tongue: a case report. Kulak Burun Boğaz Ihtis Derg KBB J Ear Nose Throat. 2004;13(3-4):98-101. [ Links ]
14. Vidal M, Delevaux I, André M, Marroun I, Gavet F, Voinchet H, et al. [Lingual tuberculosis revealing disseminated tuberculosis]. Rev Médecine Interne Fondée Par Société Natl Francaise Médecine Interne. 2007;28(2):124-6. [ Links ]
15. Memon GA, Khushk IA. Primary tuberculosis of tongue. J Coll Physicians Surg--Pak JCPSP. 2003;13(10):604-5. [ Links ]
16. Feller L, Anagnostopoulos C, Bouckaert M, Raubenheimer EJ. HIV/TB co-infection: literature review and report of multiple tuberculosis oral ulcers. SADJ J South Afr Dent Assoc Tydskr Van Suid-Afr Tandheelkd Ver. 2005;60(8):330-2, 343. [ Links ]
17. Michalak A, Wojtas G, Kidawa I, Tylzanowska-Nitek K. [Tuberculosis of the tongue in a patient with disseminated pulmonary tuberculosis]. Pneumonol Alergol Pol. 2004;72(1-2):28-31. [ Links ]
18. Díaz Manzano JA, Castillo Romero JL, Padilla Romero MJ, Sánchez Laínez JJ, Castillo Aguilar C, Cegarra Navarro MF. [Simultaneous pulmonar, laryngeal and lingual affectation by Mycobacterium tuberculosis]. An Otorrinolaringológicos Ibero-Am. 2007;34(3):237-41. [ Links ]











 text in
text in