Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.3 Bogotá Sept. 2014
A case study of simulated endoscopy: a conceptual approach based on observation of the hands-on workshops of the Colombian Association of Digestive Endoscopy
Camilo Blanco Avellaneda MD. (1), Catalina Cortés Buitrago MD. (2), Alix Yineth Forero Acosta MD. (3), Nadia Sofía Flores MD. (4), Diego Aponte Martín MD. (5), Raúl Cañadas Garrido MD. (6)
(1) Master of Education, Associate Instructor at the Universidad El Bosque in Bogotá, Colombia. MD in Gastrointestinal Surgery and Endoscopy. E-mail: cblanco@etb.net.co
(2) Master in Education, Instructor at the Pontificia Universidad Javeriana, Anesthesiologist. Bogotá, Colombia.
(3) Master of Education, Speech Therapist at the Clínica Fernando Vanegas Cano. Bogotá, Colombia.
(4) Master of Education, Director of Undergraduate Credential Program in Childhood Education in the Faculty of Education at the Fundacion Universitaria del Area Andina, BA in Early Childhood Education. Bogotá, Colombia.
(5) Internist, Gastroenterologist and Endoscopist, Former President of ACED, Graduate Academic Coordinator of the Gastroenterology Program at the Fundación Universitaria Sanitas in Bogotá, Colombia.
(6) Professor of Gastroenterology at Pontificia Universidad Javeriana, Internist, Gastroenterologist and Endoscopist in Bogotá, Colombia.
Received: 22-05-14 Accepted: 21-07-14
Abstract
Introduction: Simulation is an educational tool that consists of artificial replication of phenomena, processes or real situations in order to achieve an established academic goal. The aim of this study is to describe the pedagogical elements and the organizational model used in activities simulating endoscopy at an international convention of digestive endoscopy in order to compare them with the categories currently accepted for Medical Education Based on Simulation.
Methods: This is a qualitative, cross-sectional study. Data were collected during five hours of simulation workshops attended by six instructors and 40 students. Data were collected through observation, notes, checklists, oral and visual records, interviews with instructors and student surveys. The information was analyzed and compared using five categories accepted in previous work and related to Medical Education Based on Simulation.
Results: Five workstations were designed for the acquisition and development of individual technical skills. The allocation of time and the design of the workshops led to overcrowded work stations, unequal opportunities, and a five hour long stretch of work. This was, stressful for both students and instructors. Nevertheless, students perceived the simulation exercises of the convention as positive activities.
Conclusions: This study allows us to propose suggestions for improving activities at future events. First, it is essential that all components of the simulation be planned, designed and implemented according to established learning objectives. Second, all simulations should be accompanied by some kind of feedback. Third, it is recommended that highly structured formats be used during all stages of the simulation when participants do not have sufficient prior experience in education based on simulation.
Keywords
Gastrointestinal endoscopy, learning, simulation, feedback, medical education.
INTRODUCTION
Continuing education programs offered by American and European scientific associations, and in the last year by Colombian Association of Digestive Endoscopy and the Colombian Association of Gastroenterology, have introduced practical activities through workshops. These workshops use concepts, methods and simulation-based learning (SBL) whose main focus is to achieve improvement in endoscopic techniques.
SBL and Simulation-based Medical Education (SBME) require knowledge of the constituent elements. Some of these were used in this study including adult education (the physicians attending these events are specialists), the role of technology (the workshops specifically addressed training in the latest endoscopic techniques) the use of multimedia images and videos of real cases, and the use of INSIMED (Instituto de simulación médica - Institute for Medical Simulation) in Bogotá, a learning environment designed specifically for simulation activities.
Training physicians to perform gastrointestinal endoscopy through SBL and SBME offers several benefits including the opportunities of teaching and practicing in an environment that is safe for the student. There are no risks for real patients (several of the activities in these workshops were performed on ex-vivo models. In accordance with the planning and structure of the sessions, they foster motivating learning rather than punitive scenarios for both students and teachers. This is a space in which students and teachers can share their experience, transmit the systematic nature of their practice and apply educational and evaluative concepts.
The significant human, organizational, technological and financial resources required for organization of these workshops deserve and motivate a broad understanding of the different pedagogical elements that must underlie these types of educational practices.
This study is based on the traditional case study in social science type of qualitative research. Its purpose is to describe the educational characteristics and the organizational model used in simulation-based learning during the X International Course of Digestive Endoscopy held in Bogotá on April 3, 2014 and to compare them with categories currently accepted as constituents of SBL and SBME. It is hoped that this will enrich concepts in a way that allow changes and recommendations for upcoming activities of continuing medical education in gastroenterology and digestive endoscopy.
General Objective
The general objective of this study is to conceptually identify the pedagogical aspects underlying simulation-based Medical Education activities through observation of workshops about endoscopic techniques at an international specialty conference.
Specific Objectives
The studys specific objectives are to explain in detail the methodological and logistic issues involved in the workstations, to characterize the activities of teaching, learning, feedback and monitoring related to practical simulations, and to review the educational concepts applied in simulation of gastrointestinal endoscopy based on evidence including impacts, development and prospective.
MATERIAL AND METHODS
This is a descriptive, cross-sectional, qualitative study of social research. Fieldwork was conducted during the Workshops using ex-vivo models at the X Curso Internacional de Endoscopia Digestiva de la Asociación Colombiana de Endoscopia Digestiva (ACED - X International Course of Digestive Endoscopy of the Colombian Association of Digestive Endoscopy) held in Bogotá on April 3, 2014.
The observations used for this study were made during the second evening of simulation workshops. Six instructors and forty students participated. All students were specialists or senior residents in adult or pediatric gastroenterology, endoscopy and gastrointestinal surgery. Students came from a variety of Colombian public and private institutions and have varying amounts of experience and areas of interest. Two students are directors of Colombian Association of Digestive Endoscopy. Three manufacturers of endoscopic equipment provided four technicians, three other suppliers of endoscopic supplies provided four additional technicians, and two directors of INSIMED participated. Total attendance was 72 people.
The educational research group consisted of four people with Masters Degrees in Education, a research assistant, and the two directors of the Colombian Association of Digestive Endoscopy (DA and RC) from the workshops organizing committee who agreed to participate and be evaluated by this study. The group designed and implemented the study including all data entry and analysis and the writing of this study.
Qualitative data were collected from four sources: non-participant observations by three of the investigators (CB, AF and NF) with the help of a check list previously developed from field research, video and audio tapes of the activities at each of the 5 workstations, unstructured interviews of the 5 instructors, students answers to questions for evaluation of the course on a form prepared by two members of the research team (DA-RC).
This was a social case study which used qualitative analysis. The study was oriented according to five deductive categories accepted for scientific works related to SBL and SBME. The study triangulated theory, data collection and the interpretations of the researchers.
Ethical Issues
Instructors, students, assistants and simulation center managers were all informed of the general purpose of the research and of the confidential handling of information from performances and images observed during the workshops. Verbal consent was obtained for access to each of the stations, for taking notes, for recording audio and video, and for use of satisfaction surveys and interviews of participants considered relevant to the investigation. Fieldwork records are safe and privacy is maintained.
Methodology of Analysis
The content analysis method was used to study qualitative data obtained from notes, audio and visual recordings of workshops, interviews and surveys. Findings were placed within the categories identified on the checklist in the results section. The checklist is based on the pedagogical elements that should be found in simulation workshops according to previous studies that the group consulted.
RESULTS
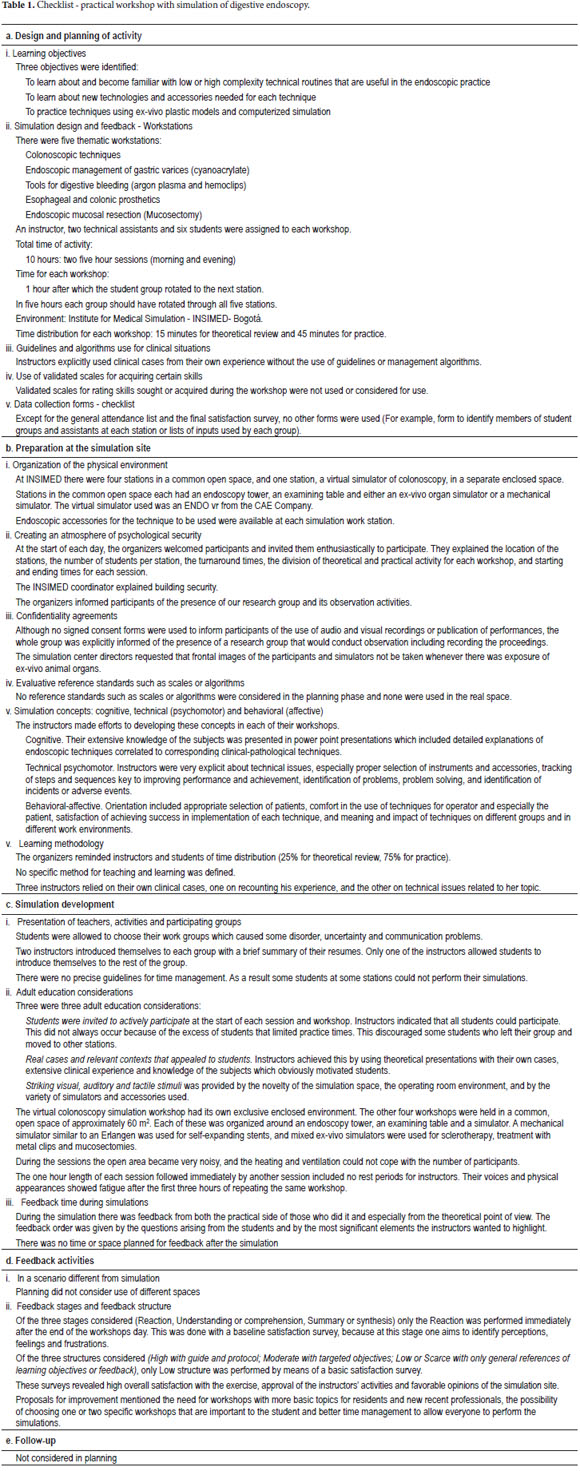
The results shown below are organized by category and presented with their respective components and findings. (Table 1)
DISCUSSION
Simulation is imitation or modeling of a real-life situation to be used in training or instruction (1). It can be understood from a pedagogical point of view and according to its structure as a technique or teaching-learning methodology that allows replacement or amplification of real experiences by means of authentic replication or interactive tools. The usefulness of this method has been confirmed in complex scenarios similar to clinical ones such as aviation and military training (2-4).
The learning method traditionally used for digestive endoscopy focuses on the use of clinical scenarios with real patients. Procedures are performed directly on the patient under the supervision of an instructor.
Accepted advantages of the traditional method include one-on-one training, real problems solved in real time, and immediate feedback and assessment of results. Limitations include dependence on patient availability, patient authorization for student involvement; increased time of procedures, high costs that may be incurred and, most significantly under current conditions, the potential risks and discomfort caused to patients (1).
Clinical simulation has been motivated by four factors (3, 5, 6):
1. The 1964 Helsinki Declaration which protects individuals subject to experimentation.
2. The safety required by patients who are passive subjects in educational processes.
3. New approaches in medical education based on quality criteria, timelessness of processes and demonstration of objective skills.
4. New computing, electronic and virtual reality technologies.
Scientific societies such as the Colombian Association of Digestive Endoscopy, the Colombian Association of Gastroenterology and the American Society for Gastrointestinal Endoscopy (ASGE) make efforts to provide simulation activities to their members. These have drawn a great deal of attention in the past 15 years. Since the development of flexible endoscopes, they have been recognized as potential tools for improving training and gaining endoscopic expertise (7, 8).
Endoscopic simulation currently uses at least four types of simulators:
1. First generation mechanical simulators are usually plastic. The Erlangen mannequin is the icon of these simulators. Th is techniques was first described in 1974 (9).
2. Mixed models that combine mechanical simulators with ex-vivo animal organs (10).
3. Computer virtual reality simulators that combine video technology with interactive graphic computer simulation to allow appreciation of movement of endoscopic accessories in connection with images that appear in real time (11,12).
4. Live animal models are more realistic and closer to the sensitivity of the human tissue. These models usually use young pigs weighing approximately 35 kg (13).
In this case the first three types of simulation models were used because of for practical reasons and the type of facility. Clear variations exist among these types. Mechanical simulators are simple and require minimal preparation for use, but provide less real experiences. Mixed mechanical simulators with ex-vivo organs are also very easy to use but are more demanding in terms of preparation and disposal of tissues. Although their consistency is more rigid than live tissue they allow simulated performances of most procedures. Computerized simulators have the great advantages of long term use and low costs of updating procedures once the initial investment has been made. They also provide a friendly environment once training has been received. Live models are completely realistic but have more ethical issues and require time and effort to prepare animals, have high costs including anesthesia, veterinarians and a much more complex operating room (1).
Support for the use of simulation for training and achieving competence in gastrointestinal endoscopy is based on two types of studies performed with mixed ex-vivo simulators and computer simulators. One type consists of studies constructed to test the validity of both the structure and the use of the simulator in order to identify the presence of either an inexperienced or experienced endoscopist, according to measurement of variables such as duration of procedure, complexity achieved, recognition of pathology and others. The other type consists of clinical studies that aim to determine whether the use of the simulator leads to better performance of endoscopic procedures in the clinical field (1).
Studies show that there are computerized simulators that distinguish between novice and expert endoscopists (14, 15). Clinical studies that compare traditional clinical training with patients and traditional theoretical training with that achieved with computerized simulators and ex-vivo mixed models report that residents trained with computerized simulators can initially show more complete performance skills with less need for help (16, 17). On the other hand, better skills are achieved when ex vivo mixed models are used. This is especially true for hemostasis techniques, therapeutic procedures such as polypectomies (18), and high risk procedures such as ERCPs and double-balloon enteroscopies (19, 20).
Training with colonoscopy simulators is also supported by validity of construct studies that rank performance from novice to expert in the technique tested (21-23). Multiple clinical studies show better performances from those trained with simulators that from those trained with patients and those without previous clinical experience. This is especially true for early stages of training in colonoscopy.
Nevertheless, all students require a similar number of in vivo cases to reach the 90% skill level [160], even though the performance of physicians trained with simulators is superior in the first 80 cases or even in the first 30 cases (24, 25). In other words, progress made with initial simulator training is rapidly tied to clinical practice which is a modest benefit from the medium to long term use of the simulator.
In this context, there are two unresolved problems that limit the use of simulation for training in endoscopy. First, the lack of concrete definition of the skills obtained from simulation prevents identification of expertise attained in one or more specific techniques. One tool for colonoscopy that allows evaluation of minimum standardized skill performance of students has been validated. It defines minimum benchmarks that must be reached (26). These include of depth of the insertion for cecal intubation, full examination conducted independently, and ability to identify reference sites in the colon (27). There are still no precise validated definitions of the skills to be achieved for other colonoscopic procedures through training with simulation.
The second problem is the cost of models that limits their use in institutions that must ration their resources (28). This is especially true for computer and live models. Costs include monetary investments and investments in human resources, although the use of simulators may reduce the number of trainers needed (7). One study warns that students may not improve as much in training through simulation as they do with traditional methods if there is no feedback from a tutor (23). Likewise, there is no clarity on the benefits of the intermittent or continuous use of simulators which could modify costs. Simulation training for hemostasis procedures has improved by having three separate weekend sessions over a period of 7 months (16).
The proposal to transform and develop training with endoscopy simulators makes integrating three learning conditions more importance. These conditions are independent study, training in a structured program with study modules, and work with simulators that reinforces students skills (28).
This proposal seeks to achieve two central goals through the use of simulation: shorten the learning curve by decreasing the number of clinical procedures with real patients needed to achieve expertise or proficiency in a particular technique, and correlate evaluation of skill levels obtained in simulation with proficiency in performance of procedures with real patients which requires identification of what is transferred efficiently from training with simulators (7).
Studies show that students acquire skills through training, but there have been no attempts to distinguish between technical and cognitive skills, so this remains a dark area that requires further investigation since achievement of integrated skills including technical and cognitive abilities is central to significant learning in the long term (7).
Work has already been done to develop next generation endoscopic simulators which will simulate evaluative integrity. These simulators will allow construction of particular standard learning curves for each specific procedure which will be integrated into the simulators program. They will develop at least two elements that allow the objective assessment of the skill: 1) identification of key metrics of a particular procedure; and 2) development of an assessment tool based on this metric. This will enable measurement of the range of expertise of the person in the process, and allow accurate prediction of professional performance in real clinical scenarios (28).
The results of these studies show that the benefit of simulation models is linked to selection of students at the appropriate level to benefit from training with precisely defined learning objectives combined with the use of simulation scenario that provides psychological fidelity (29). This is understood as a set of sensations that trigger real cognitive processes that allow the simulated scenario to be perceived as real thus approximating the simulator performance to the real clinical context (30).
With this future scenario and with the evidence accumulated from more than 15 years of research in the field of simulation, the valuable efforts of our national association, the Colombian Association of Digestive Endoscopy, face the reality found in this scenario of simulation workshops during an international conference. This allowed us, through the use of an observation matrix, to show the need for improvement of activities in future workshops. These improvements can be achieved by conceiving simulation within a formal educational scenario in which planning, implementation, execution, evaluation and monitoring of the learning-teaching process are all precisely defined. This will allow the design of activities that are predictable, consistent, standardized and reproducible (31). Our observation matrix which used a checklist may well be a basic tool that could be useful in the improvement process in the future.
Pedagogical considerations regarding knowledge, learning, educability, new trends, epistemology and knowledge generation should be applied to the educational approach and to training with simulators. This is especially important since medical education in general, and endoscopic training in particular, are progressively being required to include simulation as a mandatory part of postgraduate training as evidenced by the new 2012 guidelines for gastroenterology of the United States Accreditation Council for Graduate Medical Education (32, 33).
CONCLUSIONS
Given all of the above, and in agreement with Sedlak, one of the foremost experts in the world (32), there are several key elements to consider when thinking about incorporating Simulation-based Medical Education:
Simulation should not be intended to replace experience based on real patients. It should be seen as a tool to augment traditional training and should be useful for approximating knowledge of new techniques or devices.
To date, simulation has shown its greatest benefit in training for treatment of less common but more serious conditions such as active gastrointestinal bleeding or perforation of the colon.
Simulation should not be intended to replace education supervised by an instructor. In fact, as already mentioned, training with a simulator is less effective when there is no teacher supervision during its performance.
The economic, organizational, technological, and especially human resources required for simulation workshops are so significant that they perfectly merit that teachers be pedagogically qualified. These qualifications will increase the formative impact on motivated professionals that can subsequently be reflected in better and more competent care for patients.
In our case study there is evidence of urgent improvements that need to be made in upcoming workshop. There should be fewer students per station. Time at each station should be optimized by decreasing the theoretical intervention of instructors and the number of students per rotation. Practical psychomotor activity should be prioritized without omitting cognitive and affective issues. Break times for instructors and for technical assistants should be included. Students should be made aware that they need to respect their own time limits and those of their peers during practice. A wider range of topics in the workshop would allow students to select one or two topics of interest in advance. Workshops should be structured according to the level of complexity of the training needed by the participants invited. Simulations should have clear pedagogical policies regarding planning, didactic consistency of teachers, evaluation, feedback and medium and long term follow-up of the impacts of workshops.
This needed because, despite the efforts, desires and interests of current research, there is a large gap in our knowledge regarding the usefulness and real impact of endoscopic simulation on the practice of professionals such as those who participated in the program studied here. This may be a first step in that investigation.
Acknowledgements
We wish to acknowledge the help of the 2012-2014 Board of Directors of the Colombian Association of Digestive Endoscopy, Mónica Ayelde, all of the administrative and logistical staff, INSIMED and its director, and the teachers who worked as instructors. All of their collaborative, committed, generous and selfless work allow completion of the activity of the practical workshops which were the setting for this research. We want to express our special gratitude to Doctor Diego Aponte and Doctor Raúl Cañadas for having the courage to accept this study, since as organizers of the workshops they were pedagogically evaluated always looking for future improvement and benefit of the entire medical Colombian community related to digestive endoscopy.
REFERENCES
1. ASGE Technology Committee, Desilets D, et al. Endoscopic simulators. Gastrointestinal Endoscopy 2011; 73: 861-867. [ Links ]
2. Gaba D.M. The future of simulation in health care. Quality & Safety in Health Care 2004; 13(Supl.1): i2-10. [ Links ]
3. Cortés C. La retroalimentación en la educación basada en simuladores: un estado del arte. Retroalimentación efectiva en escenarios críticos de reanimación. [Tesis de Grado de Maestría]. Bogotá: Facultad de Educación. Pontificia Universidad Javeriana; 2014. [ Links ]
4. McGaghie WC, Issenberg SB, Petrusa ER, et al. A critical review of simulation-based medical educación 2010; research: 2003-2009. Medical Education 44: 50-63. [ Links ]
5. Corvetto M, Bravo MP, Montaña R, et al. Simulación en educación médica: una sinopsis. Revista Médica de Chile 2013; 141: 70-79. [ Links ]
6. Bini EJ, Firoozi B, Choung RJ, et al. Systematic evaluation of complications related to endoscopy in a training setting: a prospective 30-day outcomes study. Gastrointest Endosc 2003; 57: 8-16. [ Links ]
7. Cohen J, et al. Preservation and Incorporation of Valuable Endoscopic Innovations (PIVI) on the use of endoscopy simulators for training and assessing skill. Gastrointestinal Endoscopy 2012; 3: 471-475. [ Links ]
8. Nelson DB, Bosco JJ, Curtis WD, et al. ASGE technology evaluation report. Endoscopy simulators. May 1999. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc 1999; 50: 935-7. [ Links ]
9. Classen M, Ruppin H. Practical training using a new gastrointestinal phantom. Endoscopy 1974; 6: 127-31. [ Links ]
10. Hochberger J, Neumann M, Maiss J, et al. Erlanger ausbildungssimulator fur die interventionelle endoskopie (EASIE): Eine neue perspective fur die qualitdtsorientierte praktische Ausbildung (German). Endoskopie heute 1998; 4: 23-25. [ Links ]
11. Williams CB, Baillie J, Gillies DF, et al. Teaching gastrointestinal endoscopy by computer simulation: a prototype for colonoscopy and ERCP. Gastrointest Endosc 1990; 36: 49-54. [ Links ]
12. Noar MD. Robotics interactive endoscopy simulation of ERCP/sphincterotomy and EGD. Endoscopy 1992; 24(Suppl. 2): 539-41. [ Links ]
13. Nelson DB, Bosco JJ, Curtis WD, et al. Technology status evaluation report: endoscopy simulators. Gastrointest Endosc 2000; 51: 790-2. [ Links ]
14. Ferlitsch A, Glauninger P, Gupper A, et al. Evaluation of a virtual endoscopy simulator for training in gastrointestinal endoscopy. Endoscopy 2002; 34: 698-702. [ Links ]
15. Moorthy K, Munz Y, Jiwanji M, et al. Validity and reliability of a virtual reality upper gastrointestinal simulator and cross validation using structured assessment of individual performance with video playback. Surg Endosc 2004; 18: 328-33. [ Links ]
16. Hochberger J, Matthes K, Maiss J, et al. Training with the compact EASIE biologic endoscopy simulator significantly improves hemostatic technical skill of gastroenterology fellows: a randomized controlled comparison with clinical endoscopy training alone. Gastrointest Endosc 2005; 61: 204-15. [ Links ]
17. Maiss J, Pratt F, Wiesnet J, et al. The complementary Erlangen Active Simulator for Interventional Endoscopy training is superior to solely clinical education in endoscopic hemostasis - the French training project: a prospective trial. Eur J Gastroenterol Hepatol 2006; 18: 1217-25. [ Links ]
18. Haycock A, Youd P, Bassett P, et al. Simulator training improves practical skills in therapeutic GI endoscopy: results from a randomized, blinded, controlled study. Gastrointest Endosc 2009; 70: 835-45. [ Links ]
19. Bittner J, Mellinger J, Imam T, et al. Face and construct validity of a computer-based vistual reality simulator for ERCP- Gastrointest Endosc 2010; 71: 357-64. [ Links ]
20. May A, Nachbar L, Schneider M, et al. Push-and-pull enteroscopy using the double-balloon technique: method of assessing depth of insertion and training of the enteroscopy technique using the Erlangen Endo Trainer. Endoscopy 2005; 37: 66-70. [ Links ]
21. Sedlack RE, Kolars JC. Validation of a computer-based colonoscopy simulator. Gastrointest Endosc 2003; 57: 214-8. [ Links ]
22. Grantcharov TP, Carstensen L, Schulze S. Objective assessment of gastrointestinal endoscopy skills using a virtual reality simulator. JSLS 2005; 9: 130-3. [ Links ]
23. Eversbusch A, Grantcharov TP. Learning curves and impact of psychomotor training on performance in simulated colonoscopy: a randomized trial using a virtual reality endoscopy trainer. Surg Endosc 2004; 18: 1514-8. [ Links ]
24. Cohen J, Cohen SA, Vora KC, et al. Multicenter randomized controlled trial of the impact of virtual reality simulator training on the acquisition of competency in colonoscopy. Gastrointest Endosc 2006; 64: 361-8. [ Links ]
25. Sedlack RE, Kolars JC, Alexander JA. Computer simulation training enhances patient comfort during endoscopy. Clin Gastroenterol Hepatol 2004; 2: 348-52. [ Links ]
26. Sedlack RE. Training to competency in colonoscopy: assessing and defining competency standards. Gastrointest Endosc 2011; 74: 355-66. [ Links ]
27. Haycock A, Koch A, Familiari P, et al. Training and transfer of colonoscopy skills: a multinational, randomized, blinded, controlled trial of simulator versus bedside training. Gastrointest Endosc 2010; 71: 298-307. [ Links ]
28. Cohen J, Thompson C. The Next Generation of Endoscopic Simulation. The American Journal of Gastroenterology 2013; 108: 1036-1039. [ Links ]
29. Sedlack RE. Simulators in training: defining the optimal role for various simulation models in the training environment. Gastrointest Endosc Clin N Am 2006; 16: 553-63. [ Links ]
30. Beaubien JM, Baker DP. The use of simulation for training teamwork skills in health care: how long can you go? Quality and Safety in Health Care 2004; 13 (Supl.1): i51-56. [ Links ]
31. Corvetto M, Bravo M.O., Montaña R, et al. Simulación en educación médica: una sinopsis. Revista Médica de Chile 2013; 141: 70-79. [ Links ]
32. Sedlack RE. Incorporating simulation into the GI curriculum: the time is now. Gastrointestinal Endoscopy 2012; 76: 622-624. [ Links ]
33. ACGME Program Requirements for Graduate Medical Education in Gastroenterology (Section IV. A. 6.b) Effective July 1, 2012. Disponible en: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ ProgramRequirements/144_gastroenterology_int_med_2016.pdf. Acceso en mayo 14, 2014. [ Links ]











 text in
text in