Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.4 Bogotá Oct./Dec. 2014
Characterization of Patients with Non-Alcoholic fatty Liver Disease in a Highly Complex Colombian Hospital in 2013
Claudia Marcela Vanegas R. MD. (1), Camilo Restrepo R. MD. (1), Natalia Vargas G. MD. (1), Andrés Eduardo Marín C. MD. (1) , Lina María Martínez S. MD. (1), Carlos Enrique Yepes D. MD. (2, 3), Juan Carlos Restrepo G. MD. (1, 2, 3)
(1) Medical Faculty of the School of Health Sciences at the Universidad Pontificia Bolivariana in Medellín, Colombia.
(2) Liver Transplant Group and Gastrohepatology Group at the Hospital Pablo Tobón Uribe and the Universidad de Antioquia in Medellín, Colombia.
(3) Medical Faculty of the School of Health Sciences at the Universidad Pontificia Bolivariana and Gastrohepatology Group at the Hospital Pablo Tobón Uribe and the Universidad de Antioquia in Medellín, Colombia. E-mail: jcrestrepo@une.net.co; jcrestrepo@hptu.org.co
Received: 25-03-14 Accepted: 05-11-14
Abstract
Non-alcoholic fatty liver disease (NAFLD) affects 2% to 8% of the general population. It is associated with obesity, type 2 diabetes, metabolic syndrome and insulin resistance.
Objective: The objective of this study was to characterize patients with NAFLD who were treated in the Hepatology Department of a 4th level hospital between 2006 and 2011.
Methods: This was a descriptive, observational and retrospective study of a population consisting of all patients treated in the hepatology department of a 4th level hospital who had been diagnosed with NAFLD. Patients with other liver diseases were excluded. Data was collected from medical records on a form designed by the researchers. Data were then tabulated and analyzed in SPSS ® version 17.0. Measures of central tendency, position and dispersion were calculated for quantitative variables, and absolute and relative frequencies were calculated for qualitative variables. The Mann-Whitney U test and the and chi-square test were used as appropriate.
Results: 58.5% of the sample were female patients. We found that 52.3% of the sample were overweight according to BMI, and 72.1% were diagnosed with fatty liver by ultrasound.
Conclusion: We found that most patients with NASH have elevated body mass indices similar to reports published elsewhere.
Keywords
Fatty liver, insulin resistance, obesity.
INTRODUCTION
Non-alcoholic fatty liver disease is defined as the accumulation of fat in the hepatocytes that accounts for more than 5% of the liver's weight (1). NAFLD is an entity that has a wide clinical and pathological spectrum that includes simple steatosis and non-alcoholic steatohepatitis (NASH). As time passes, NASH is gaining recognition as an important cause of morbidity and mortality (2).
Global prevalence is highly variable with figures ranging from 2.8% to 88% depending on the population studied. These data have been increasing proportionally as rates of obesity, sedentary lifestyles and high calorie diets have increased (1). It has been found that patients in the fourth to sixth decades of life have higher predispositions to NAFLD and NASH (3).
Besides obesity, non-alcoholic fatty liver disease is also associated with metabolic syndrome whose risk factors include insulin resistance, diabetes, increased waist circumference and dyslipidemia (4).
Clinical and initial laboratory findings are often nonspecific, but traditionally the diagnosis occurs incidentally, mainly by ultrasound (5).
The best method for identification and classification of fatty liver disease is histology which can differentiate between early and late forms. However, for proper diagnosis it is necessary to exclude other disorders, especially viral hepatitis, significant intake of alcohol, and exposure to potentially hepatotoxic drugs (1, 6).
Since initial changes resulting from non-alcoholic steatohepatitis, including increased aminotransferase, can predict future development of cirrhosis, early identification might allow prevention of cirrhosis (7). Ten year follow-ups have shown that 25% of patients with NASH progress to cirrhosis and that fatal liver failures occur in 12% of these patients. Many patients diagnosed with cryptogenic cirrhosis (up to 80%) eventually develop NASH. Frequently, the transplanted liver of these patients may develop alterations that are identical to NASH (8).
Changes in lifestyle that decrease body weight can change aminotransferase levels, thus and have an overall effect on liver histology and on the natural course of the disease (2, 9, 10).
According to Idrovo and Guevara, the estimated prevalence of NASH is 2% to 3%, but the estimated prevalence of NAFLD is 20% which makes it the primary reason patients are referred to hepatologists (11). The prevalence of NAFLD in patients with chronically increased levels of aminotransferase ranges from 21% to 63%, but increases to 95% when these patients are also obese. The prevalence of NASH in obese patients is 25%, but for patients with type II diabetics it is 63%.
This explains the need for this study which attempts to characterize patients with non-alcoholic fatty liver disease referred to the Hepatology Unit of a high complexity hospital between 2006 and 2011.
METHODOLOGY
This is a retrospective, descriptive and observational study of the population of patients who had non-alcoholic fatty liver disease and who were treated in the hepatology unit at a high complexity hospital in Medellin during the study period. Exclusion criteria were histories of alcoholism (consistent consumption of more than 40grams of alcohol per day), diagnoses of viral or autoimmune hepatitis, metabolic disorders, hereditary factors, and/or drugs or toxins. The data collection plan consisted of gathering information from medical histories of patients and from clinical, laboratory, and treatment data related to the clinical course of the disease. A data collection form was used. Later, the data were tabulated and analyzed in SPSS version 17.0. Central tendency, position and dispersion measures were calculated for quantitative variables, and absolute frequencies were calculated for qualitative variables. Prevalence of the disease was calculated. Associations between fatty liver disease and body mass index (BMI) were analyzed using the required statistical tests according to the data distribution. The Ethics Committee of the institution approved this research. Confidentiality was maintained for data contained in clinical files.
RESULTS
The study included 294 patients, of whom 58.5% were female. The average age was 48 years old (SD 13.7). More than 50% of patients were 50 years old or under. Average BMI was 28.7 (SD 5.0), and 52.3% of patients were classified as obese according to BMI: 18.1% of patients had obesity grade I, 8.3% had obesity grade II, and 3.2% were morbidly obese. Only 18.1% had normal BMIs. Needless to say, these data refer to the 73.5% of patients who had information available.
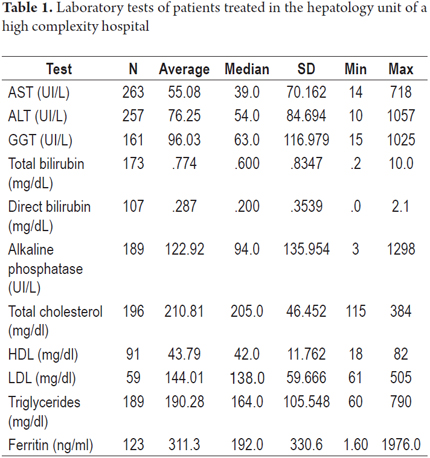
Fifty percent of the patients had aspartate aminotransferase (AST) levels less than or equal to 39 54 IU/L, alanine aminotransferase (ALT) levels less than or equal to 54 IU/L, and Alkaline Phosphatase (AP) levels less than or equal to 94 IU/L. Up to 50% of patients had total cholesterol and triglycerides of less than or equal to 205 mg/dl and 164 mg/dl respectively. The median for ferritin was 192 ng/ml with an average of 311.3 (SD 330.6) (see Table 1).
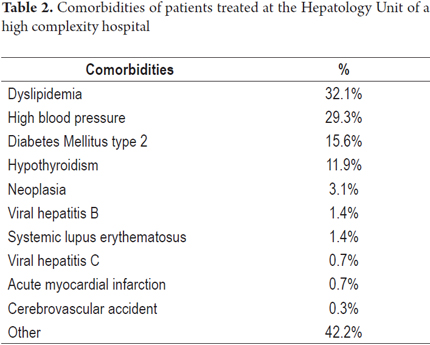
The most frequent comorbidities were dyslipidemia (32.1%), arterial hypertension (29.3%) and diabetes mellitus type 2 (15.6%). Other comorbidities occurred less frequently (see Table 2).
One third of the patients did not consume alcohol, and 26.9% drank occasionally but less than 40g/day. It is necessary to clarify that no information was obtained from 39.8% of the medical records.
According to ultrasound reports, 72.1% had fatty liver disease, 0.7% had hepatomegaly and 5.4% did not have fatty livers. It must be clarified that 21.8% of the reports were not found in the medical records. Only 19% of patients had liver biopsy reports results, and 17.1% of these confirmed fatty livers. The remainder (81%) did not.
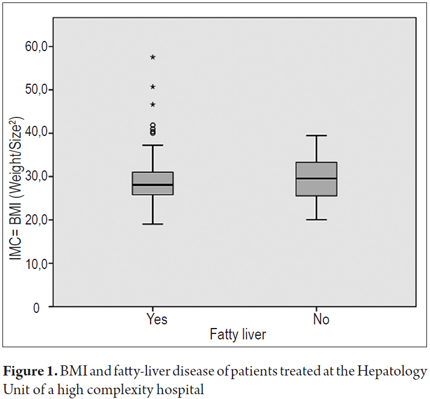
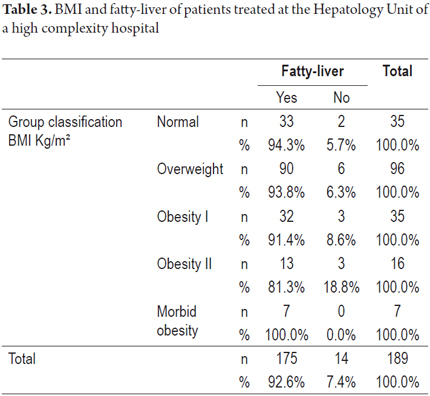
Figure 1 shows that up to 50% of patients with fatty livers had BMIs that were less than or equal to 27 Kg/m² with a more accurate interquartile range. Table 3 shows that the diagnosis of fatty livers was higher in all cases of patients classified with altered BMIs regardless of classifications. It was 100% for patients with morbid obesity (see Table 3).
DISCUSSION
NAFLD and NASH are currently recognized as major public health problems because of their relevant association with obesity and diabetes. They are also considered to be the main causes of chronic liver disease which may develop into cirrhosis, decompensated cirrhosis and hepatocellular carcinoma and which has great impacts on morbidity and mortality of individuals and large costs for the health care system (12). Women are not free from this entity which underlines the importance of learning how to recognize it and treat it in a timely and appropriate manner. A study by Leite et al. found results that were similar to those of our study including a frequency of female patients of 68.1% (7). NAFLD and NASH have high prevalences and a primary relationship with insulin resistance syndrome which is a liver manifestation. This disease must be recognized early in patients with risk factors so that healthy and durable lifestyle changes can be made in a timely way that allows the patient to recover from the disease and that prevents progression to cirrhosis.
In recent years progress has been made in understanding the natural history of NAFLD/NASH. However, most studies have limitations because of the slow progression to liver disease, the limitation of follow up times to the short and medium term, and the possible referral and selection biases. Hepatic steatosis is strongly related to all clinical phenomena of insulin resistance including obesity, metabolic syndrome and diabetes (13). When studies are conducted in obese patient populations (BMI> 30 kg/m²), 50% to 90% present NAFLD/NASH. One study found that up to 50% of patients with fatty livers who were classified as being overweight had body mass indices less than or equal to 27 and 27.5% were classified as being (7). It is believed that up to 50% of diabetic patients have NASH. This is a very important relationship that is also considered to be an important prognostic factor. Despite not being included in the diagnostic criteria, hepatic steatosis is considered to be the manifestation in the liver of metabolic syndrome. It has also been shown that the greater the number of criteria present in a person, the greater the risk of NAFLD.
A large percentage of the patients who are tested in cardiovascular risk programs are found to have high transaminase levels due to their underlying conditions (14). The level of the enzyme is usually mildly increased, less than 3 times the reference values, with an AST/ALT ratio of less than one, unlike these levels in patients with Alcoholic Hepatopathy (15). Higher values were observed in our study than those found in other studies such as that by Ortiz-Lopez et al. which had average results of 41 ± 2 IU/L for AST and 59 ± 3 for ALT (16). Patients with steatosis but normal liver enzymes or with an established diagnosis of cirrhosis do not require liver biopsies due to the low value that the procedure offers and the risks that inherent in this invasive study (17). Although only 19% of the patients participating in our study had liver biopsies performed, 91% of these had findings of fatty livers confirmed. This can be compared to the study by Bhat et al. in which 53% of the study population had biopsies and 100% of these patients had histopathological changes (2). One limitation of this study was the difficulty of getting complete data from all of the study patients because of incomplete some medical records. Another limitation is the lack of standardization for diagnosis of the disease. Further studies related to the pathogenesis of NAFLD are needed to complement the findings of this study. In conclusion, it was found that most patients with non-alcoholic fatty liver disease have high body mass indices which is similar to those reported in the data of other studies.
REFERENCES
1. Souza MR, Diniz M de F, Medeiros-Filho JE, Araújo MS. Metabolic syndrome and risk factors for non-alcoholic fatty liver disease. Arq Gastroenterol 2012; 49(1): 89-96. [ Links ]
2. Bhat G, Baba CS, Pandey A, Kumari N, Choudhuri G. Life style modification improves insulin resistance and liver histology in patients with non-alcoholic fatty liver disease. World J Hepatol 2012; 4(7): 209-17. [ Links ]
3. Bellentani S, Marino M. Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD). Ann Hepatol 2009; 8(Suppl. 1): S4-8. [ Links ]
4. Santos LF, Hernández G, Varón A, Beltrán O, Botero RC, Mejía G. Enfermedad hepática por infiltración grasa no alcohólica: La nueva pandemia del milenio. Rev Col Gastroenterol 2010; 25(4): 380-398. [ Links ]
5. Roldan-Valadez E, Favila R, Martínez-López M, Uribe M, Méndez-Sánchez N. Imaging techniques for assessing hepatic fat content in nonalcoholic fatty liver disease. Ann Hepatol 2008; 7(3): 212-20. [ Links ]
6. Farrell GC, van Rooyen D, Gan L, Chitturi S. NASH is an Inflammatory Disorder: Pathogenic, Prognostic and Therapeutic Implications. Gut Liver 2012; 149-71. [ Links ]
7. Leite AB, Mattos AA, Mattos AZ, Coral GP, Evaldt S. Risk factors for nonalcoholicsteatohepatitis in cryptogenic cirrhosis. Arq Gastroenterol 2012; 49(4): 245-9. [ Links ]
8. Cubides VI, Guevara LG. Enfermedad hepática grasa no alcohólica: NAFLD. Rev Col de Gastroenterol 2004; 19(1): 44-49. [ Links ]
9. Jun DW. [The role of diet in non-alcoholic fatty liver disease]. Korean J Gastroenterol 2013; 61(5): 243-51. [ Links ]
10. Centis E, Moscatiello S, Bugianesi E, Bellentani S, Fracanzani AL, Calugi S. Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver disease. J Hepatol 2013; 58(4): 771-7. [ Links ]
11. Idrovo V, Guevara G. Enfermedad hepática grasa no alcohólica: NAFLD. Rev Colomb Gastroenterol 2004; 19 (1): 44-9. [ Links ]
12. Lam B, Younossi ZM. Treatment options for nonalcoholic fatty liver disease. Therap Adv Gastroenterol 2010; 3(2): 121-137. [ Links ]
13. Farell GC, George J, Hall P, McCullough AJ. Fatty Liver Disease: NASH and Related Disorders. NEJM 2005; 353(20): 2200-2201. [ Links ]
14. Suzuki A, Angulo P, Lymp J, St Sauver J, Muto A, Okada T, Lindor K. Chronological development of elevated aminotransferases in a nonalcoholic population. Hepatology 2005; 41(1): 64-71. [ Links ]
15. Angulo P. Nonalcoholic Fatty Liver Disease. N Engl J Med 2002; 346(16): 1221-31. [ Links ]
16. Ortiz-Lopez C, Lomonaco R, Orsak B, Finch J, Chang Z, Kochunov VG, Hardies J, Cusi K. Prevalence of prediabetes and diabetes and metabolic profile of patients with nonalcoholic fatty liver disease (NAFLD). Diabetes Care 2012; 35(4): 873-8. [ Links ]
17. Hashimoto E, Taniai M, Tokushige K. Characteristics and diagnosis of NAFLD/NASH. J Gastroenterol Hepatol 2013; 28 (Suppl. 4): 64-70. [ Links ]











 text in
text in