Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.4 Bogotá Oct./Dec. 2014
Argon Plasma Ablation versus Band Mucosectomy for Endoscopic Management of Barrett's Esophagus with dysplasia or Esophageal Carcinoma
Rodrigo Castaño MD. (1), Óscar Álvarez, MD. (2), Amy Piñeres MD. (3), Mario H Ruiz MD. (4), Andrés Rojas MD. (5), Alejandra Álvarez (6), Luis Miguel Ruiz (6), David Restrepo (7), Víctor Calvo (8)
(1) Gastrointestinal Surgeon and Endoscopist, Chief of the Graduate General Surgery Program at Universidad Pontificia Bolivariana, Member of the Gastrohepatology group at the Universidad de Antioquia and the Instituto de Cancerología Clínica las Américas in Medellín, Colombia. rcastanoll@hotmail.com
(2) Radiologist, Internist and Gastroenterologist, Professor at the San Antonio Campus of the University of Texas, Director of Gastroenterology at the Veterans' Administration Hospital of Texas Valley Coastal Bend in Harlingen, Texas.
(3) General Surgeon at the Clínica Bolivariana in Medellín, Colombia.
(4) General Surgeon at the Hospital Pablo Tobón Uribe in Medellín, Colombia.
(5) General Surgeon at the Instituto de Cancerología-Clínica las Américas in Medellín, Colombia.
(6) Medical Students in the Medical Faculty of the Universidad Pontificia Bolivariana in Medellín, Colombia.
(7) Medical Student in the Medical Faculty of the CES in Medellín, Colombia.
(8) Statistician in Medellín, Colombia.
Received: 31-03-14 Accepted: 05-11-14
Abstract
Introduction: Various endoscopic techniques for ablation of metaplastic esophageal epithelia which maintain the integrity of the submucosa have been described. All maintain patients under aggressive acid suppressive therapy with proton pump inhibitors. To date, few studies have compared the different endoscopic techniques for eradicating Barrett's esophagus (BE) with dysplasia. Similarly the factors that might influence patients' prognoses after these therapies have not been very consistently evaluated.
Objective: This is a pilot study which compares the effectiveness of complete eradication of BE with dysplasia through endoscopic mucosal resection (EMR) with bands and low voltage endoscopic argon plasma coagulation (APC). The three points evaluated are whether complete ablation of BE was achieved, the number of sessions required and whether and what complications occurred.
Methods: APC was performed using a flexible 10 French catheter. The voltage used was 50 W and flow timed varied between 1 minute and 2 l/min. In one group BE mucosa was treated with multi-band ligation. Up to six bands were placed per session. The mucosa with BE was removed with a polypectomy loop and a mixed stream of water. Patients were followed up endoscopically and biopsies were obtained from the four quadrants in both treated and untreated areas at three, six and twelve months after treatment ended. All patients received high doses of proton pump inhibitors.
Results: This prospective study describes our results in a group of 62 patients with Barrett's Esophagus and dysplasia. Thirty-three patients (22 men, 67%) were treated with APC and 29 were treated with EMR (19 men, 66%). Complete ablation of BE was achieved in 86.2% of patients treated with EMR and in 79% of those treated with APC. The number of sessions required to achieve complete ablation was 1 ± 1 for EMR and 2 ± 1 for APC. No major complications such as gastrointestinal bleeding requiring transfusion or perforations occurred. The only complications were two cases of esophageal stenosis, one in each group. These were successfully treated with single sessions of dilation. After a mean of 68.7 ± 18.9 months of follow-up in the APC group and 50.2 ± 19.3 months in the EMR group no cases of carcinoma of the esophagus and no deaths due to disease or therapy had occurred.
Conclusions: In patients with BE with high or low grade dysplasia, APC and EMR achieve comparably high eradication rates of neoplasia and intestinal metaplasia (79% versus 86%). Both procedures have comparable levels of effectiveness and safety and have low rates of complications. Nevertheless, APC is associated with a greater number of sessions.
Keywords
Barrett's esophagus, gastroesophageal reflux, argon plasma, dysplasia in the esophagus.
INTRODUCTION
Barrett's esophagus (BE) is an acquired precancerous lesion in which the squamous epithelium of the distal esophagus is replaced by columnar cells which have characteristics of intestinal metaplasia (1). The risk of developing carcinoma increases when the degree of dysplasia increases (2). The prognosis of esophageal adenocarcinoma is poor despite treatment. Its recognized incidence has increased everywhere in the world more than any other malignancy (3, 4). Although chronic gastro-esophageal reflux has been recognized as a trigger of intestinal metaplasia, efforts to control reflux through medical therapy and surgery have not had favorable impacts on reversing intestinal metaplasia (5, 6). At present, there are no known genetic markers that indicate a change from BE to dysplasia or cancer (7). For these reason, it has been proposed that endoscopic follow-up be used for early detection of dysplastic changes (8, 9).
Esophagectomies have traditionally been recommended for patients with high-grade dysplasia (HGD) and/or esophageal cancer, but they are not exempt from high risks of morbidity and mortality especially in elderly patients and patients with comorbidities (10). Therefore, endoscopic therapy is a suitable alternative for these patients (11). Two methods of endoscopic management which are easily accessible in our environment are argon plasma ablation and endoscopic mucosal resection using band ligation (12). These treatments in cases of BE with HGD and intramucosal carcinoma are justified in the absence of local regional lymph node involvement.
Local ablation limited to the area of dysplasia have relapse rates of 30% in monitored cases (13-15). Consequently, the goal of treatment for BE should be complete eradication of the metaplastic epithelium and replacement by neosquamous epithelium which does not have potential for malignancy of specialized intestinal metaplasia, with a low rate of complications (16-19). There is no evidence that supports necessary eradication of BE when dysplasia is not present. Recently, use of the APC technique was described in our environment. A prospective follow-up study demonstrated that APC for dysplastic BE eradicates 69% of the epithelium. Average study follow-up time was close to four years (20). A major limitation of ablation is the absence of a histological specimen which might indicate the success or failure of the therapy.
Histological samples can be obtained with EMR alone or in combination with ablation and are particularly important in case of BE with nodules. In the case of intramucosal carcinoma, it provides information regarding differentiation, the presence or absence of lymphovascular invasion, the depth of the invasion and whether or not resection margins are compromised (21). We do not consider the endoscopic technique of ligation without mucosal resection to be good medical practice (22).
EMR techniques include resection with a polypectomy snare, lifting and cutting with submucosal injection, cap-assisted resections, and resections with ligation (11). Ligation followed by resection is simple and easy to implement which was extrapolated from experience with ligation of esophageal varices (23, 24). Band mucosectomy can be performed with or without prior injection of solution. The tissue is sucked into a cap to then the band is released creating pseudo-polyp which is then resected with the polypectomy snare and retrieved for histological study. Assisted cap resection has been compared with band ligation and found to be equally safe and effective (25).
This study compares the effectiveness of APCs and EMRs at achieving complete eradication of BE with dysplasia or carcinoma in situ. The procedures were performed several tertiary medical centers in Medellin, Colombia.
MATERIALS AND METHODS
Patients included in the study were referred to two tertiary hospitals in Medellin, Colombia for treatment of BE and low to high grade dysplasia of high from June 2004 to November 2011.
Two months prior to every procedure, each patient underwent endoscopy during which biopsy samples were taken every 2 cm in all four quadrants. Patients whose biopsies indicated cancer invasion beyond the mucosa (T1 sm or deeper) were referred for surgical resection. None of the patients underwent endoscopic ultrasound.
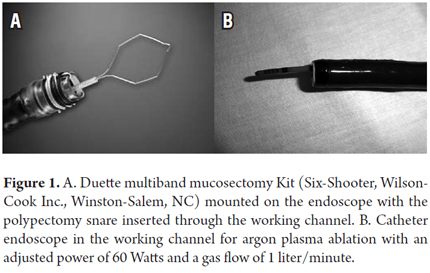
From 2004 to 2009, patients were treated with APC, but in January 2006 band mucosectomies were introduced. The Duette multiband mucosectomy Kit was used for six cases, but for most patients ligations were performed with the varicose vein band kit followed by resection of tissue with a 10mm or 20 mm polypectomy snare (Figure 1).
Patients were excluded when they had other malignancies, esophageal resections, and advanced esophageal cancer and when they were pregnant, older than 80 years of age or were terminally ill.
The ethics committee of the University of Antioquia approved the protocol and the study. This committee is the entity that evaluates the research protocols of residents.
Evaluation prior to procedure
Informed consent was obtained from all patients. The length of BE was defined as the distance between the margin of the proximal gastric folds and the squamous-columnar junction. Endoscopic mapping of the BE was done by taking samples with standard biopsy forceps every two centimeters in the four quadrants. Alternately, biopsy samples were taken directly from lesions when they were visible (change in color, nodules, ulcers, etc.).
Techniques of endoscopic therapy
Band Mucosectomy
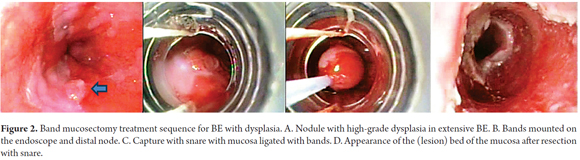
Patients were sedated with a combination of intravenous midazolam and meperidine. Propofol was not used in any of the patients. No adverse effects attributable to sedation occurred. The Duette multiband mucosectomy Kit (Wilson Cook Medical-Bloomington, IN) includes a multiband linker and a 1.5 by 2.5 cm hexagonal polypectomy snare made of braided wire (Figure 1A). The original Saeed Multiband ligator (Wilson-Cook Medical, Winston-Salem, NC) was used for most of the patients. Once the ligator is mounted on the tip of the endoscope, the endoscope is advanced into the esophagus, aspiration creates a pseudo-polyp and mucosal ligation is performed with 6 bands when the Duette kit is used and with up to 10 bands when the Saeed kit is used (Figure 2).
A 30 Watt alternating current was used to make cuts. Submucosal injections were not used before suction and ligation. The next application was in the mucosa immediately adjacent to the resection margin. The number of treatments, length of treated dysplastic BE and adverse reactions (immediate and delayed) were all registered. The extent of ligation was determined individually according to the length and configuration of BE and/or macroscopic lesions and whether or not there was a single focus of dysplasia or multiple foci. The product of resection was brought to the stomach and from there was collected with a Dormia basket or Roth Net. Polyps were fixed in 10% formol for histopathology. Patients were discharged the same day after they had recovered from sedation. They were given a double dose of proton pump inhibitor for 10 days, four daily doses of 15 ml of sucralfate for 10 days, and 500 mg of acetaminophen with 8 mg codeine for a week. A liquid diet was prescribed for three days followed by a normal diet.
Argon plasma ablation
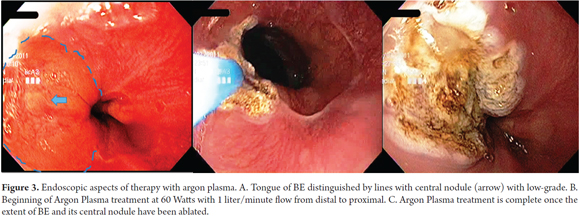
It was originally designed for open surgery. It is a contactless electrocoagulation procedure for endoscopic use. Argon gas is provided through a Teflon catheter inserted through the working channel of the endoscope. The argon is ionized with an electrosurgical unit with a high frequency current (Figure 1B). It generates temperatures up to 130°C which desiccates the tissue to a maximum depth of 3-4 mm. It is ideal for ablation of the metaplastic epithelium in BE. With the patient sedated with midazolam and meperidine, the argon gas is administered through the work channel of the endoscopy in a straight line through the catheter or radially until the conductive tissue is found. In our procedures APC was used with 60 Watts of power and a flow of 1 liter/minute. The APC starting point was the gastroesophageal junction from which point it moved in the proximal direction. According to the principles of physics, argon gas tends to travel from coagulated areas which have high impedance to inadequately coagulated areas which have low impedance (Figure 3).
The main advantages of APC are its easy mobility, low cost, and the absence of the biological hazards of lasers and absence of any licensing requirements. The number of sessions needed depends on the extension of the BE and patient tolerance to treatment.
Patients were discharged the same day after recovering from the procedure. Following discharge they were treated with a double dose of proton pump inhibitor for 10 days, four daily doses of 15 ml of sucralfate for 10 days, and 500 mg of acetaminophen with 8 mg codeine for a week. A liquid diet was prescribed for three days followed by a normal diet. Patients were contacted by telephone five to seven days after the procedure to check for any adverse effects due to treatment.
Pathology
Histological evaluation includes a description of the suitability of the specimen for histologic interpretation, presence of specialized epithelium and degree of dysplasia. Dysplasia was defined as neoplastic epithelium confined to the basement membrane in the absence of inflammation and staged according to the Vienna classification as negative for dysplasia, indefinite for dysplasia, LGD, HGD and carcinoma (26, 27). When cancer was found, the following factors were determined: depth of invasion, degree of differentiation (well or poorly differentiated), location of invasion (lymphatic, vascular or neural), whether the resected area was compromised, depth of compromise, and lateral extension of compromise. The side margins cannot be properly evaluated when the sample is resected in fragments. T1A mucosal cancer was defined as a lesion whose depth of invasion reached no further than the muscularis mucosa. T1B mucosal cancer was defined as a lesion which extended into the submucosa without compromising the muscularis propria.
Biopsies taken during endoscopic follow-ups of the new squamous epithelium were used to assess the presence of intestinal metaplasia in the epithelium or below it (sub-squamous intestinal metaplasia or hidden or submerged Barrett's esophagus).
Monitoring
Whether or not eradication of intestinal metaplasia was complete was determined through histology and endoscopy. During follow up endoscopy, standard biopsy forceps were used to take samples at intervals of one centimeter from all four quadrants from the distal esophagus to the gastro-esophageal junction. If no intestinal metaplasia was found after two consecutive endoscopies, we considered the metaplasia to have been eradicated. Recurrence was defined as any histological finding of intestinal metaplasia with or without dysplasia after the complete eradication of dysplastic BE.
During the follow-up period patients received 40 mg of a proton pump inhibitor (omeprazole or esomeprazole). Patients were treated endoscopically every 6-12 weeks until BE had been eradicated. Endoscopic follow-up examinations were done 6, 12, 18 and 24 months after treatment, and then every year thereafter. Follow-ups include four quadrant biopsies of the neosquamous epithelium in the treated area.
Statistical Analysis
Absolute distributions, relative distributions and summary indicators such as arithmetic mean, standard deviation, median and interquartile range were used for descriptive analysis. Whenever necessary, the Chi square test, Fisher's exact test and the likelihood ratio, were used to estimate relations of personal and clinical issues depending on the type of technique used. The Shapiro-Wilk test was used to test normality of distribution. Based on this, either Student's t-test or the Mann-Whitney U test was used to compare independent measurements. The Kaplan - Meier estimator was used for survival analysis. The curves obtained with this methodology were compared using the Log Rank test (Mantel-Cox). A p value of less than 0.05 was considered statistically significant. Data entry, processing and analysis were done with IBM SPSS Statistics 21.
RESULTS
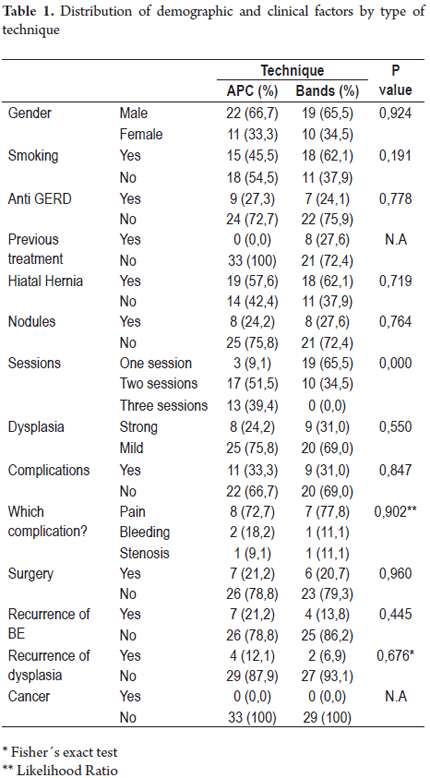
Over a period of seven years, sixty-two patients (41 male, 66%) were treated for Barrett's esophagus with argon plasma ablation coagulation or resection. Thirty-three patients were treated with APC and 29 patients underwent endoscopic band mucosectomies. Patients' ages ranged from 48 to 72 years (average age: 63 ± 4.8 years).
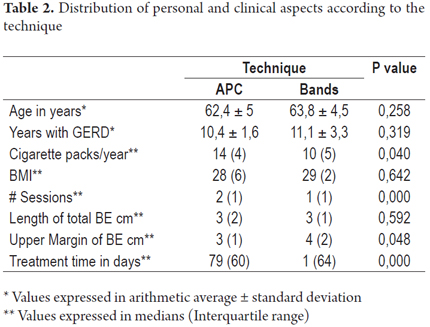
Data recorded for all patients in both groups included how many years each patient had suffered gastro-esophageal reflux, any history of anti-reflux surgery, any history of smoking, presence of hiatal hernia, body mass index, and whether or not nodules associated with BE were found (Table 1).
Other factors that were evaluated included the degree of dysplasia, the presence or absence of nodules in BE, the average length of the esophagus in which the entire circumference of the esophagus was compromised by BE, and the highest margin of BE within the esophagus, the number of sessions, complications, and average time of treatment. In the band mucosectomy group, eight patients been treated with APC with the intention of removing dysplasia prior to resection (Table 2).
Some patients in both groups experienced pain after interventions: APC (24%) and bands (24%). One patient in each group needed dilation because of stenosis. Only one patient in the APC group required hospitalization for 48 hours due to chest pain, sore throat and fever. The patient recovered completely after treatment with analgesics and intravenous fluids. There were no perforations and only two cases of bleeding during therapy with APC and one case in the band mucosectomy group. No transfusions were needed in either group.
The results of the histopathological examination after endoscopic band mucosectomy showed changes in 11 patients. The grade of dysplasia increased in eight patients: six from low grade to high grade, and two from HGD to carcinoma, one in situ and one with invasion of the submucosa. The grade of dysplasia decreased in three patients from HGD to LGD and did not change in the remaining 18 patients.
During the follow-up period there were no relapses into BE in the form of submucosal islets, the appearance of dysplasia related to the circumferential extent or length of the proximal margin of BE.
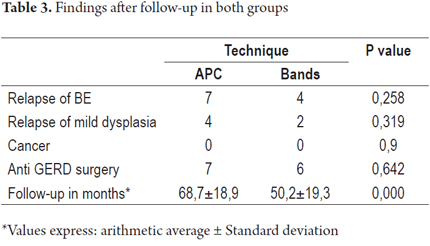
The two groups were compared based on the follow-up protocol at 3, 6, 12 and 18 months. During monitoring relapses were documented in seven patients in the APC group (21%) and in four patients in band mucosectomy group (13.8%). The earliest relapse of BE occurred after 8 months. Dysplasia was again apparent in four patients treated with APC and in two treated with mucosectomy including two of those who had had relapses of BE. There were no cases of cancer found during follow-up (Table 3)
Treatment was considered to have failed when any patient presented BE following either treatment. Three patients had one report each of BE in the follow-up biopsies, but this was not repeated in any of the other biopsies. Two patients had been treated with APC (one with submerged BE and the other one with epithelial BE). The third had been treated with band EMR (epithelial BE). Treatment of these patients was not considered to have failed.
DISCUSSION
Esophagectomy has been the standard treatment for the management of patients with high-grade dysplasia or intramucosal carcinoma. Although patients have been cured, the rates of morbidity and mortality are very high especially in medical centers with low volumes of this kind of surgery (28).
The goal of endoscopic ablation in cases of Barrett's esophagus with dysplasia is to achieve complete eradication of intestinal metaplasia and dysplasia and maintain eradication for the long term and with minimal risk of complications.
This study compares APC and endoscopic band mucosectomy for treatment of BE with dysplasia. With better follow-up and endoscopic biopsy protocols for BE, it is expected that more cases of dysplasia will be detected. Endoscopic treatment is suitable for both dysplasia and intramucosal cancer of the esophagus. Early endoscopic treatment combined with ablative techniques such as APC, photodynamic treatment, radiofrequency and mucosal resection lead to better prognoses for patients. The intention of these treatments is to provide similar survival rates and times to those obtained by surgery but with lower morbidity and mortality rates and with a better cost-benefit ratio. The ideal ablation technique or combination of techniquese has not been identified yet. The purpose of this study was to compare two ablation techniques, APC and endoscopic band mucosectomy, through follow-up of patients who had been treated for BE with dysplasia.
In 1998 Mork (29) and Byrne (30) published the first studies of the use of APC to treat BE. Their initially favorable results have not been replicated in more recent studies, including in our environment (20). There is no consensus regarding the Wattage that should be used for APC. The best results like those of Manner who eradicated 77% of BE without dysplasia were achieved with 90 Watts of power but with high rates of morbidity (31). There is still no evidence that ablation of Barrett's esophagus without dysplasia is of any utility. The current study used an intermediate power of 60 Watts, although treatment with only 30 Watts of power have also been described (32).
Inoue initially described endoscopic mucosal resection assisted by a cap on the tip of the endoscope (33). This technique was modified by Fleischer who applied a band to the esophageal tissue after creating a pseudo-polyp by aspiration (with or without injection of the submucosa) which was the resectioned with a polypectomy snare (23).
APC has been randomly compared with photodynamic treatment by Hage (34), Raghunath (35) and Kelty (36) with similar results for both BE treatments for patients with or without dysplasia but with short monitoring periods of 12 months. The cost-benefit ratio favors APC.
Penetration of the thickness of the esophageal wall is a key determinant of the success of treatment. Ackroyd has evaluated the thickness of the esophageal epithelium with or without intestinal metaplasia in paraffin blocks (37). He suggests a probable BE thickness of 0.6 mm (slightly higher than the squamous epithelium). Ablation with APC and ablation with photodynamic treatment are more than sufficient to eradicate metaplastic and dysplastic tissue from the esophageal mucosa.
The occurrence of metaplastic epithelium below the squamous epithelium (hidden BE) was initially described by Barr (38). This has been found in all types of treatment. The development of cancer in this layer of the epithelium had previously been reported (35, 39-42).
The rates of adverse effects for both treatments were similar, and there were no major complications such as perforations in any of the patients in either group. One patient in each group required dilation to solve problems with stenoses.
Recently, combined modalities involving mucosal resection together with ablative treatments have shown better results. However, a study with 120 patients with BE and dysplasia divided into two groups would be need to achieve conclusions. This suggestion combined with sufficient monitoring time could help detect significant differences.
Endoscopic ultrasound was not considered for evaluation prior to procedures in this study because published studies indicate it can overestimate the depth of compromise (43) even in cases of nodular Barrett's esophagus in which the recommendation is removal of the nodule (44).
The use of APC for BE ablation has been reported in various studies (29, 45-51). These studies report reversal of Barrett's esophagus in between 42% and 98% of cases after one to six treatments. In this study the complete ablation of BE with dysplasia was achieved with APC in 67% of the patients, while it was achieved in 79% of those treated with endoscopic band mucosectomy. While these results are not encouraging, they can be explained by the strict definition of Barrett's esophagus, persistently applied in this study. It was considered that any specialized columnar epithelium constituted persistent Barrett's esophagus. During monitoring this meant any appearance of subepithelial islets which had carcinogenic potential.
It has been suggested that the results of APC can be improved by increasing the power to more than 65 Watts and by increasing the depth of treatment for more complete ablation (46, 47). In our study we replicated the previous finding showing that recurrence is more common when BE is more than 3 cm deep and when acid reflux persists. Various studies of PPI treatment are based on findings of pH-impedance, but because we did not monitor pH in this study, we cannot exclude the possibility that the reappearance of BE was related to increased exposure to pHs of less than 4 in patients with subepithelial BE.
Until recently, the goal of the treatment was to control dysplasia. However, recent studies have shown that genetic abnormalities may persist after treatment (52, 53). Van Hillegersberg described two patients who had BE with cancer whose treatments only incompletely eradicated the cancer (54). This underlines the conclusion that the goal of treatment should be the complete abolition of the metaplastic epithelium. The presence of BE after the first treatment with APC indicates the need for further treatment until complete BE eradication. However, neither treatment achieved complete eradication of BE in all patients.
Resected specimen quality should be sufficiently satisfactory to determine the depth of tumors. Our study showed changes in histological diagnoses in two patients with HGD. They were treated by mucosectomy and were found to have intramucosal cancer in their follow-ups. Another patient was found to have submucosal invasion which was handled with an esophagectomy. No residual lesion was found.
Endoscopic mucosal band mucosectomy is a safe and effective procedure. It can be part of the evaluation, staging and endoscopic eradication HGD or intramucosal carcinoma. It can be applied without the need for prior submucosal injections. It can be used on an outpatient basis with sedation and analgesia without interrupting the patient's oral intake. Large areas of the mucosa can be quickly resected with great histological accuracy for precise diagnosis and staging of the lesion. Secondary stenosis after mucosectomies can occur with mucosal resections when the compromise involves more than 50% of the esophageal circumference. In general, patients respond easily to dilation. Bleeding is uncommon, and, if happens, it occurs in the early hours after the intervention. It can be avoided if the cut is performed with pure coagulation (21).
Recently, a combination therapy for BE with dysplasia based on endoscopic band mucosectomy has been suggested. The remnant BE is treated with APC. This method had lower recurrence rates for dysplasia during a two-year follow-up period (55). This therapeutic combination was corroborated in a published study (56).
In our study, the initial treatment to eradicate of BE with dysplasia was successful for every patient. However, in the long-term monitoring, it became apparent that the possibility of relapse is common despite initial ablation. This has also been suggested in recent studies (57).
There are few publications that support the cost effectiveness of ablation for patients with BE with dysplasia. When comparing the costs of APC with those of photodynamic treatment, the numbers favor treatment with APC (35). It has been recognized that ablation to treat BE is cost-effective if the treatment is definitive and if it does not require tracking in the future, but at this moment this cannot be offered with any of these treatments.
CONCLUSIONS
Endoscopic ablation methods including APC and band mucosectomy have been gaining space as treatments for patients with BE and dysplasia. They can control this with lower rates of patient morbidity and mortality than invasive surgical procedures. This study, as in the medical literature generally, does not identify which one endoscopic treatment is the best, but it does make clear treatment should be early and that only a few retreatments should be needed for complete eradication.
Because of the low costs of these procedures in our environment, they can be cost-effective even with long-term endoscopic monitoring.
We need more studies with more patients and longer follow-up times to establish whether ablation or resection is the best method treatment, whether a combination of treatments might be best, and whether these treatments really are as efficacious as esophagectomies in terms of disease-free survival and quality of life.
Conflicts of interest
The authors have no conflicts of interest.
This study was conducted with the support of the Sustainability Project of the Office of the Vice Rector of Research at the University of Antioquia.
REFERENCES
1. Leeuwenburgh I, Scholten P, Calje TJ, et al. Barretts esophagus and esophageal adenocarcinoma are common after treatment for achalasia. Dig Dis Sci 2013; 58: 244-52. [ Links ]
2. Hur C, Miller M, Kong CY, et al. Trends in esophageal adenocarcinoma incidence and mortality. Cancer 2013; 119: 1149-58. [ Links ]











 text in
text in