Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.4 Bogotá Oct./Dec. 2014
Preliminary Experience with Radiofrequency Ablation of Barrett's Esophagus with in situ Dysplasia or Carcinoma
Rodrigo Castaño MD. (1), Óscar Alvarez MD. (2), Amy Piñeres MD. (3), Mario H Ruiz MD. (4), Andrés Rojas MD. (5), Alejandra Álvarez (6), Luis Miguel Ruiz (6), David Restrepo (7), Víctor Calvo (8)
(1) Gastrointestinal Surgeon and Endoscopist, Chief of the Graduate General Surgery Program at Universidad Pontificia Bolivariana, Member of the Gastrohepatology group at the Universidad de Antioquia and the Instituto de Cancerología Clínica las Américas in Medellín, Colombia. rcastanoll@hotmail.com
(2) Radiologist, Internist and Gastroenterologist, Professor at the San Antonio Campus of the University of Texas, Director of Gastroenterology at the Veterans' Administration Hospital of Texas Valley Coastal Bend in Harlingen, Texas.
(3) General Surgeon at the Clínica Bolivariana in Medellín, Colombia.
(4) General Surgeon at the Hospital Pablo Tobón Uribe in Medellín, Colombia.
(5) General Surgeon at the Instituto de Cancerología-Clínica las Américas in Medellín, Colombia.
(6) Medical Students in the Medical Faculty of the Universidad Pontificia Bolivariana in Medellín, Colombia.
(7) Medical Student in the Medical Faculty of the CES in Medellín, Colombia.
(8) Statistician in Medellín, Colombia.
Received: 31-03-14 Accepted: 05-11-14
Abstract
Introduction: Barrett's esophagus (BE) is the result of chronic damage to the esophageal epithelium caused by the acid of gastrointestinal reflux diseases (GERD). It is defined as replacement of the by stratified squamous epithelium that normally lines the esophagus with metaplastic columnar epithelium. BE represents a risk factor for esophageal adenocarcinoma. The aim of radiofrequency ablation (RFA) is to destroy the metaplastic epithelium with the electric current of a radiofrequency to stimulate the reappearance of stratified squamous epithelium in the distal esophagus.
Objective: The objective of this study was to evaluate the efficiency and safety of RFA which has recently been introduced in the city of Medellin, Colombia for management of BE with in situ dysplasia or carcinoma.
Materials and Methods: Ten patients were treated with RFA. BE patients with in situ dysplasia or carcinoma and histological diagnoses were chosen for treatment. RFA procedures were done with BARRX equipment, the circular HALO360 system or the HALO90 system. Macroscopic and microscopic effects of RFA, patient tolerance to treatment and complications were evaluated.
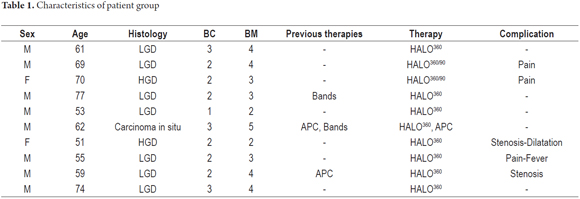
Results: A group of 10 patients received treatment with RFA. All ten finished treatment and follow-up. Seven patients had low-grade dysplasia, two had high-grade dysplasia, and one patient had in situ carcinoma. Two patients had undergone endoscopic resections of nodules and treatments of mucosa with bands prior to therapy with RFA. A total of 13 procedures were performed: 10 RFAs with the HALO360, 2 RFAs with the HALO90 and one argon plasma treatment for residual BE in one patient. Eradication of metaplastic and dysplastic esophageal epithelium was achieved in all patients and confirmed by endoscopic and histologic evaluation. No significant complications related to RFA were found, but in two patients esophageal stenoses were found. One required endoscopic dilatation three weeks after therapy.
Conclusions: Based on these preliminary results we believe that this is a promising method that is well-tolerated by patients and which has no major complications. Metaplastic and dysplastic epithelium of the distal esophagus were successfully eradicated in most patients.
Keywords
Barrett's esophagus, esophageal cancer, esophageal dysplasia, metaplasia, in situ carcinoma, radiofrequency ablation.
INTRODUCTION
Barrett's esophagus (BE) is the result of chronic damage to the esophageal mucosa due to reflux of gastric acid or gastro esophageal reflux disease (GERD). BE is defined as replacement of the stratified squamous epithelium that normally lines the esophagus by columnar intestinal metaplasia. BE is a risk condition for the appearance of esophageal adenocarcinoma (EAC). Globally, statistical measures of the incidence of BE in the general population vary from 0.9% to 6.0% while the global incidence of EAC in BE patients is estimated to be less than 0.5% (1, 2). Nevertheless, BE patients with high grade dysplasia progress to EAC at a rate of 6% per year (3). The incidence of EAC is increasing faster than any other neoplasia according to forensic reports (4). In light of endoscopy's inadequate recognition of BE and the stable growth of EAC cases, these patients have recently become a focus of attention in all latitudes.
During the last two decades, various endoscopic methods have been used to eradicate BE. Argon plasma therapy (5), endoscopic resection of the mucosa (6), submucosal dissection (7), cryotherapy (8), photodynamic therapy (9), and more recently radiofrequency ablation (RFA) have been used the most frequently (10). Colombian publications about these techniques include those by our own Doctors Rey and Pinilla (11).
RFA uses alternating electrical current to induce an electromagnetic field charged with rapidly oscillating ions that collide with one another and create molecular friction. This results in the liberation of exothermic energy that, when applied to esophageal tissue, leads to a thermic lesion (controlled with water vapor), protein coagulation and cellular necrosis which destroys the metaplastic or dysplastic epithelium and thus stimulates the process of epithelial regeneration (12). In order to effectively eradicate the mucosa, there should be no change in contact between the esophagus and the ablation interface. Hence, RFA is not generally applied with a healing intention to nodular tissue.
The first study of eradication of BE with dysplasia was a multi-center random controlled simulation trial by Shaheen with a group treated with RFA and a control group. In that study the RFA treat group had a 77% BE eradication rate while the control group had only a versus 2.3% rate. Similarly the RFA group had an 81% eradication rate for high grade dysplasia versus and 90% rate for eradication of all types of dysplasia compared to 19% and 23% in the control group. The rate of progression to cancer was reversed with the RFA group's rate of only 2.4% while the control group's rate was 19% with 6% of patients developing stenoses in 12 months of follow up (13). Recently, these researchers have updated their study with data from three years of follow up which shows dysplasia and intestinal metaplasia eradication rates of 98% and 91% respectively for long segments of BE (5cm average) (14).
The evidence from other well-designed randomized controlled blinded studies also suggest that RFA is highly effective for removing BE with favorable margins of safety as demonstrated endoscopically and histologically (15, 16). Even though long term monitoring has been limited, the eradication of BE persists in more than 90% of patients after 5 years of follow-up (17). In addition, studies of the properties of the neosquamous epithelia that regenerates after RFA show the absence of pre-existing oncogenic anomalies, suggesting a transition to low risk epithelia (18).
The purpose of this study is to evaluate the efficacy and safety of radiofrequency ablation for managing BE with any grade of dysplasia or esophageal carcinoma described as in situ in a group of patients treated in Medellín, Colombia.
MATERIALS AND METHODS
Using a Halo® 360 catheter, RFA was performed on 10 patients (9 men) between the ages of 52 and 74 years (average age was 66 years) over a period of 18 months (January 2012 to July 2013). All patients had had symptoms of GERD for over 10 years and had had hiatal hernias. The study's inclusion criterion was presence of BE with any degree of dysplasia or in situ carcinoma histologically confirmed by two pathologists. Two patients, one with a high degree dysplasia and the other with in situ carcinoma, had previously undergone endoscopic band mucosectomies. None of the patients were evaluated with endoscopic ultrasound.
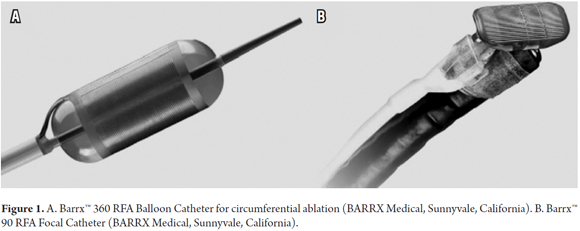
Before treatment all patients were evaluated endoscopically with biopsies taken from spots 1 centimeters apart in each of the four quadrants of the esophagus for the entire length affected by BE. BE was classified according to the Prague classification (19). Procedures were planned every two months for each patient as necessary. They were performed under general anesthesia using HALO equipment produced by BARRX Medical (Sunnyvale, California USA). The initial treatment used the HALO360 probe in all patients to determine whether circumferential BE was present. The HALO90 device was used as complementary therapy (Figure 1).
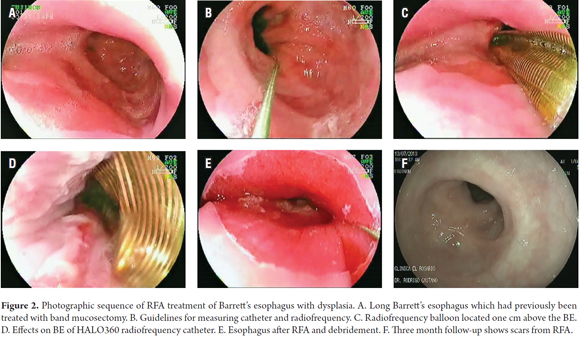
Before treatment, a 4 cm long measuring catheter was used to determine the diameter of the esophagus and to facilitate the choice of HALO 360 balloon catheter size to be used in therapy. The HALO ablation catheter has a 3 cm balloon on its distal extreme with a bipolar electrode on its external surface. This electrode is available in balloon diameters of 22 mm, 25 mm, 28mm, 31mm and 34 mm. Dosimetry studies show that circumferential ablation is more effective with the application of 10 a 12 j/cm2 and 40 W/cm2 to achieve the eradication of the entire thickness of the mucosa (Figure 2) (20, 21).
The radiofrequency was administered to dysplastic tissue with a bipolar electrode at 12 Joules/cm2. The depth of ablation must include the mucosa and the superficial portion of the submucosa. Two of the patients received HALO90 therapy. One of the patients who did not authorize complementary therapy with the HALO90 catheter ended up receiving argon plasma treatment.
For both the 360 degree and the 90 degree ablation catheters the energy generator automatically applies the radiofrequency to the electrode after being activated with the pedal. Due to the equipment's pre-established combination of high power and energy, the depth of tissue penetration by the ablation is uniformly 1000 um. Since this is not dependent on the operator, RFA results in controlled deconstruction of the columnar epithelial layer, the lamina propria and part of the mucosa's muscular layer while the submucosa remains unscathed (22).
After treatment, patients took a proton pump inhibitor at a standard dose of twice a day and an oral acid blocker before each meal and before going to bed. The patient also continued on a liquid diet for 3 days followed by a soft diet for one week.
The treatment's endoscopic and microscopic effects including patient tolerance to the procedure and possible complications were evaluated.
Endoscopic follow-ups were scheduled for three, six and twelve months after procedures were performed. Biopsy samples were taken from the four quadrants of the area treated by RFA. With the help of digital chromoendoscopy (FICE or NBI), special emphasis was placed on endoscopic and histological follow up for any evidence of the reappearance of BE or of buried Barrett's metaplasia.
RESULTS
Of the 10 patients, seven presented low grade dysplasia, two presented high grade dysplasia, and one had a background of in situ carcinoma. All of the patients were treated with the HALO 360 probe in their initial session. Abnormal metaplastic epithelia with dysplastic changes and in situ carcinoma were eradicated from all patients. Two patients required an additional session with the HALO90 catheter while another patient required removal of a residual islet with argon plasma due to administrative problems.
Three patients had previously undergone other types of treatment: one had had argon plasma ablation and band mucosectomy, one had had undergone band mucosectomy, and the third had undergone argon plasma therapy. In none of these cases did the previous treatments interfere with the success of RFA therapy. Only one patient did not have a hiatal hernia, and hernias in the other nine patients were not impediments to safe therapy.
No immediate complications arose that could be attributed to therapy. Two weeks after the intervention, patients mentioned spontaneous thoracic pain that became exacerbated with ingestion and improved with the initially ordered medication. Only one patient presented fever and vomiting the night after treatment. Three patients required a change to another type of intervention because of pain as soon as the therapy began (parenteral analgesics and/ or ICU management).
Two patients presented symptomatic stenoses. One of them required dilatation therapy with Savary-Guilliard plugs of up to 17mm after three weeks. The stenosis was alleviated with only one dilatation session.
The average follow-up time was less than a year, yet none of the patients presented metaplastic or dysplastic epithelia or carcinoma.
Table 1 summarizes patient characteristics.
DISCUSSION
To date, there is no single consistent and unequivocal indication for BE with dysplasia or in situ carcinoma in the esophagus (23). Despite the growing interest in managing this condition, most guidelines only recommend monitoring patients with BE for early detection of cancer. The frequency of endoscopic monitoring depends on the type of lesions associated with BE according histological findings (24). For isolated metaplasia, endoscopies with biopsies are recommended every 2 to 3 years, for low grade dysplasia they are recommended once a year, and for high grade dysplasia every 3 to 6 months (25). However, some authors suggest surgical removal in cases of low grade or high grade dysplasia although refinement and development of endoscopic treatment techniques have favorably impacted this issue (26-28).
RFA is one of the most recently developed methods for managing BE. Data from two large clinical trials suggest a success rate of 92% over 5 five years, including in patients who have only metaplasia without dysplasia (25-29). An efficacy rate of 81% has been shown for patients with low grade dysplasia, and an efficacy rate of 90% rate has been shown for cases with high grade dysplasia (30-31). RFA therapy is as effective as endoscopic resection of the mucosa but has a lower rate of complications (13).
Complications related to RFA that have been described include nausea, thoracic pain, transitory dysphagia and odynophagia, stenoses, mediastinitis and esophageal perforations. Perforations are treated with self-expanding stents (32-34). It has been estimated that stenoses, the most common complications in our patients, occur in 8% of all RFA treatments, but this is much less than the 88% described after endoscopic mucosal resection (35).
No significant complications were found in the group we treated. This was due in good measure to the strict criteria that RFA would be deferred in patients with ulcerated esophagitis because it could lead to perforations or significant stenosis (36). However, the concomitant use of endoscopic mucosal resection followed by RFA has been described in a study of 24 patients who did not have a higher complication rate (37).
When the cost-effectiveness RFA was evaluated in a study using the Markov model with a hypothetical patient cohort of 50 years with non-dysplastic BE, three scenarios were considered: 1- natural history, 2- only follow-up, 3- RFA. Considering an RFA eradication rate of 50% for non-dysplastic BE, which was intentionally lower than those reported in studies, it was concluded that RFA is the most cost-effective method for non-dysplastic BE depending on patient age and taking into consideration both the cost of RFA and the RFA eradication rate (38).
A second economic model was designed to simulate the natural history of a cohort with BE, with patient ages between 50 years and 80 years or death. Cost-effectiveness was compared for three strategies: 1- monitoring, 2- esophagectomy and 3- RFA. Endoscopic RFA of BE with high grade dysplasia increased life expectancy by three years at a cost that was USD 6,000 lower than the cost of no intervention. RFA is the most cost-effective strategy for patients with low grade dysplasia and patients without dysplasia if the ablation permanently eradicates the low grade dysplasia in more than 28% of cases or BE without dysplasia in more than 40% of cases. For RFA to be cost-effective, follow-up must be suspended after therapy (39).
A third model used a cohort of patients of 50 years of age with BE and without dysplasia, who were monitored until 80 years of age or death. Cost-effectiveness was evaluated in three scenarios: 1- endoscopic monitoring with surgery if cancer was detected, 2- endoscopic management with RFA if dysplasia was detected or 3- initial RFA followed by endoscopic controls. The study found that among patients with high grade dysplasia, an initial RFA followed by endoscopic monitoring was more cost-effective than the other options (40).
The use of RFA with HALO360 for treating BE was approved by the FDA in 2005, and the use of the HALO90 for treating BE received FDA approval in 2006. The scientific evidence was considered to be of sufficient quality to conclude that these treatments have health benefit in the eradication of high risk epithelia. In a comparison of this technology with endoscopic monitoring for cases of low grade dysplasia, RFA demonstrated the best prognoses and cost-effectiveness (13). In addition, the net benefit of complete eradication of BE may be achieved outside of the limits of formal research studies. Faced with this, the American Gastroenterology Association (AGA) and the British guidelines recommend the procedure and consider RFA to be necessary for treatment of dysplastic BE (29, 41).
A recent retrospective study of 417 patients has shown that more experience with the procedure was related to achievement of better results but was not clear about how much experience is required for achievement of good results (42).
One of the main concerns about treating BE with RFA is durability over time. A meta-analysis has evaluated that durability. It looked at 18 very heterogeneous studies with 3,802 total patients that evaluated the efficiency of RFA and at six very heterogeneous studies with 540 patients that evaluated durability. The meta-analysis demonstrated that complete eradication of BE with dysplasia was achieved in 91% of the cases and that BE progressed to cancer in only 0.7% of cases. Stenoses were the most frequently found complication at 5% (17).
When comparing proactive RFA treatment of BE with mild dysplasia, Phoa found that ablation decreases progression to HGD from 26.5% to 1.% with an absolute reduction of 25% that corresponds to an NNT of 4 (43). This was a multi-center study of 136 patients that was randomized 1:1 and controlled. The study also found that RFA decreased the risk of progression of cancer from 8.8% to 1.5% with an absolute reduction of 7.4%. Total ablation of dysplasia was achieved in 92.6% of the patients in the treated group compared to only 27.9% in the control group. Total ablation of intestinal metaplasia was achieved in 88.2% of the patients in the treated group compared to 0% in the control group. Adverse effects were found in 19.1% of the treated group, however, these were mild. The most common adverse effect was stenosis, which was resolved with an average of 1 endoscopic dilatation.
The main limitations of our study are the small number of patients and the short follow-up time. Despite these limitations, our data together with the information provided in the literature from throughout the world show that RFA is a feasible and accessible therapy in our current environment that has a satisfactory potential for managing BE with any grade of dysplasia as well as with in situ carcinoma. Studies with a larger number of patients and longer follow-up times which include genetic and molecular information about BE may allow us to define which group of patients benefits most from these therapies. These studies are especially needed because of the potential morbidity and high costs despite the high level of safety.
CONCLUSIONS
RFA is an option for treating BE and any grade of dysplastic epithelia that decreases the risk of progression to malignancy. This therapy may be used conjointly with endoscopic removal in the case of visible nodules of lesions and in situ carcinoma. Adverse effects are not common, and although esophageal stenoses, thoracic pain, nausea and vomiting have been found, serious complications are rare. Post-intervention acid suppression is key to minimizing local pain and for allowing regrowth of the epithelia.
Conflicts of interest
The authors have no conflicts of interest.
This study was performed with the support of the Sustainability Project of the Office of the Vice Rector of Research of the Universidad de Antioquia.
REFERENCES
1. de Jonge PJ, van Blankenstein M, Grady WM, Kuipers EJ. Barretts oesophagus: epidemiology, cancer risk and implications for management. Gut 2014; 63: 191-202. [ Links ]











 text in
text in