Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.4 Bogotá Oct./Dec. 2014
Case Report of Eosinophilic Gastroenteropathy and a Literature Review
Sandra Roberto A. (1), Rómulo Bonilla G. MD. (2), Gabriel Pérez G. MD. (3)
(1) Fourth year medical student at the Hospital Universitario de Santander of the Universidad Industrial de Santander in Bucaramanga, Colombia. sandrarobertomd@gmail.com
(2) Surgeon, Gastroenterologist and Adjunct Professor at the Hospital Universitario de Santander of the Universidad Industrial de Santander in Bucaramanga, Colombia.
(3) Medical Pathologist and Adjunct Professor at the Hospital Universitario de Santander of the Universidad Industrial de Santander in Bucaramanga, Colombia.
This case was presented at the XXVII International Scientific Congress (XXVII Congreso Científico Internacional FELSOCEM) in Santiago, Chile from the 25th to the 29th of September, 2012. The poster's name was Gastroenteritis Eosinofilica. Reporte de un Caso y Revisión de la Literatura (Case Report of Eosinophilic Gastroenteropathy and a Literature Review)
Received: 23-04-14 Accepted: 05-11-14
Abstract
Introduction: Eosinophilic gastroenteropathy is a rare disease characterized by infiltration of eosinophils into one or more layers in different parts of the gastrointestinal tract especially the stomach and the duodenum. Although in most cases it presents with abdominal pain, vomiting, diarrhea, ascites and weight loss may also appear.
Case report: The patient was a 41 year old man with a clinical picture of 9 months of sudden, intermittent abdominal pain (predominantly mesogastric pain which radiated to the lumbar region). He had been treated with antispasmodics but had not improved. Eleven years earlier he had had a right nephrectomy because of hydronephrosis. Three years earlier he had been diagnosed and treated for hypochromic microcytic anemia with hypereosinophilia. Two years earlier he had had an acute myocardial infarct, although angiography showed healthy coronary arteries. Seven months earlier he developed acute appendicitis. The pathology report at that time showed eosinophilic infiltrates, and a bone marrow biopsy revealed eosinophilia. Physical examination showed normal vital signs, but his bowel sounds were more intense and frequent (40/min) than normal, and he suffered mesogastric pain on palpation. There were no masses or organomegaly. Laboratory tests revealed anemia and 16% eosinophilia. Diagnostic images showed esophageal and gastric ileitis with microscopic evidence of eosinophil infiltration in all samples. Eosinophilic gastroenteropathy was diagnosed, and the patient was started on a hypoallergenic diet and treated with prednisone. Up to 25% of patients with hypereosinophilic syndrome may have gastrointestinal infiltration. Eosinophilic gastroenteropathy should be suspected in any patient with abdominal pain and peripheral eosinophilia. However, peripheral eosinophilia is not always present, and histopathological diagnosis is necessary.
Keywords
Gastroenteropathy, eosinophilic gastroensteritis, hypereosinophilic syndrome.
INTRODUCTION
Eosinophilic gastrointestinal disorders are quite rare and unusual diseases which are characterized by excessive infiltration of the bowel wall. Kaijser first described this entity in 1937 in two patients who had syphilis and who were allergic to neoarsphenamine (1). Between that time and 2008 more than 300 cases have been reported (2). Of the 4 million patients estimated to have been treated at the Mayo Clinic between 1950 and 1987, only forty were diagnosed with eosinophilic gastroenteritis: an incidence of 1 in 100,000 patients treated (3, 4). Our review found only three cases reported in Colombia since 2007 which confirms this entity's rarity (5).
Although its cause and pathogenic mechanism are not yet clear, up to 75% of these patients have allergies to medicines and/or foods and/or have atopic diseases such as asthma (5-8). This condition can affect any area of the gastrointestinal tract although the stomach and small intestine are the most frequently compromised. The symptoms of eosinophilic gastroenteropathy (GE) are not specific to this condition and vary according to the histologically affected layer (9). We present a case of hypereosinophilic syndrome in a patient with chronic abdominal pain with no history of allergy or atopic reactions.
CASE DESCRPTION
The patient was a forty-one year old man who had suffered chronic abdominal pain for nine months. He had seen several physicians for sudden onset of intermittent pain of moderate intensity (9/10 on a subjective scale of pain). The pain was located predominantly in the mesogastric region but radiated to the lumbar region and was associated with fatigue, weakness and pallor. This condition had been managed with antispasmodics without complete resolution of symptoms. The patient stated that he had had no fever, diarrhea or vomiting. His medical history showed that 11 years earlier he had undergone a retroperitoneoscopic nephrectomy because of hydronephrosis. Four years before we examined him, he had been diagnosed with gastritis and a biopsy showed eosinophilic infiltrates. The following year he was diagnosed with hypochromic microcytic anemia with hypereosinophilic for which he had required a total of 12 transfusions of packed red blood cells and continuous administration of ferrous sulfate and folic acid. Two years before we examined him he had suffered an acute myocardial infarct although angiography showed that he had healthy coronary arteries. Seven months prior to our examination of the patient, he underwent an appendectomy. The pathology report stated that the diagnosis was, "acute fibrinopurulent appendicitis with eosinophilic infiltration". The patient stated that he had no type of atopy or allergic reaction to medications or food.
The patient had lost 20 kg which was associated with hyperoxia. Physical examination showed normal vital signs, generalized mucocutaneous paleness, loud and frequent bowel sounds (40/min), a soft abdomen which was painful upon deep palpation in the mesogastric region, and no masses or organomegaly.
Laboratory reports showed hemoglobin of 5.8 g/dL, hematocrit at 19.9%, and 16% eosinophilia. Endoscopy identified gastritis, duodenitis, terminal ileitis, colitis and aphthoid ulcers in the rectum. Biopsies of all samples showed edema and congestion of the lamina propria and the mucosa with a mixed leukocyte influx that was predominately eosinophilic (up 22 per high power field). There were no signs of H. pylori in the glandular apical surface. Also, a bone marrow biopsy revealed greater than usual number of eosinophils.
When all patient data, records and examinations were correlated a diagnosis of eosinophilic gastroenteropathy in the context of hypereosinophilic syndrome was made. A treatment plan was developed and implemented. It consisted of a hypoallergenic diet which eliminated all wheat, milk, soy, peanuts, seafood and eggs, and administration of 25 mg of prednisone each day. A week after implementation of treatment, the patient reported significant improvements of symptoms.
DISCUSSION
Eosinophils in the gastrointestinal tract are responsible for innate immunity to parasites, regulation of lymphocytes, antigen presentation and protection against tumors. Nevertheless, over-stimulation of eosinophils generates excessive degranulation which can lead to severe inflammation, production of neurotoxins and reactive oxygen species which are responsible for the typical symptoms of eosinophilic gastroenteropathy (10, 11). Apparently allergic processes in which there are excessive release of mast cells and eosinophils and excessive TH2 cell responses to allergens bear a significant relationship with this uncontrolled activation. An association with Interleukin 5 has also been reported because it induces proliferation, growth, differentiation, activation and apoptosis of eosinophils (5).
Depending on the location of the compromised tissue, eosinophilic gastroenteropathy may be identified as esophagitis, gastritis, duodenitis or colitis. The last is exceptionally rare and only a few cases have been reported since 1979. It has a very non-specific symptoms of fever, diarrhea, abdominal pain and weight loss (12).
In 1970, Klein classified this disease according to the depth of involvement (13):
- The Mucosal Form (25% to 100%) most often affects the stomach and is manifested by anemia, fecal blood loss and weight loss.
- The Muscular Form (13% to 70%) manifests through nausea, vomiting, diarrhea, abdominal cramps, and intestinal obstruction.
- The Serosal Form (12% to 40%) manifests through eosinophilic ascites, high levels of peripheral eosinophilia and severe inflammation (3, 5, 9, 10).
Hypereosinophilic syndrome is a rare disorder defined by a peripheral eosinophilia greater than 1,500 cells/mL for more than six consecutive months, the absence of an underlying cause of hypereosinophilia and the presence of organ damage or dysfunction associated with hypereosinophilia. The most frequently affected organs are the heart, lungs, central nervous system, kidneys and skin (7, 14).
In this case the patient had suffered peripheral eosinophilia for three years with the involvement the appendix and gastrointestinal tract which are both very infrequent sites for hypereosinophilic syndrome (14). It is also important to highlight that this patient had undergone a myocardial infarct event though he had healthy coronary arteries. This could be attributed to eosinophilic infiltration although confirmation of this diagnosis would require a heart biopsy which is not available in our area. Consequently, the exact cause of the heart attack remains unknown.
Diagnosis of eosinophilic gastroenteropathy is based on three criteria: gastrointestinal symptoms, eosinophilic infiltration in one or more areas and exclusion of other causes of intestinal eosinophilia such as tuberculosis and Helicobacter pylori infections which are very frequent in our environment (3, 4).
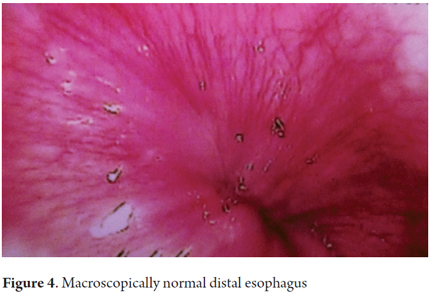
Diagnosis of 80% of these patients is done through upper digestive tract endoscopy of the stomach and small intestine. In most cases, macroscopic study of the gastrointestinal mucosa shows normal mucosa, slight edema and congestion, and even ulcers or lesions with nodular configurations (15).
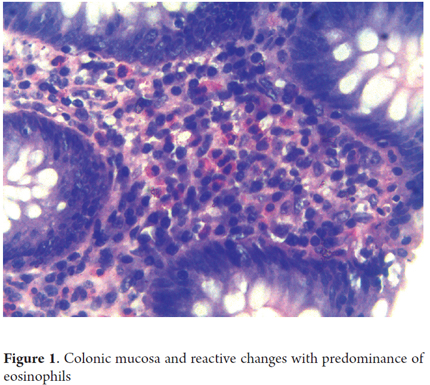
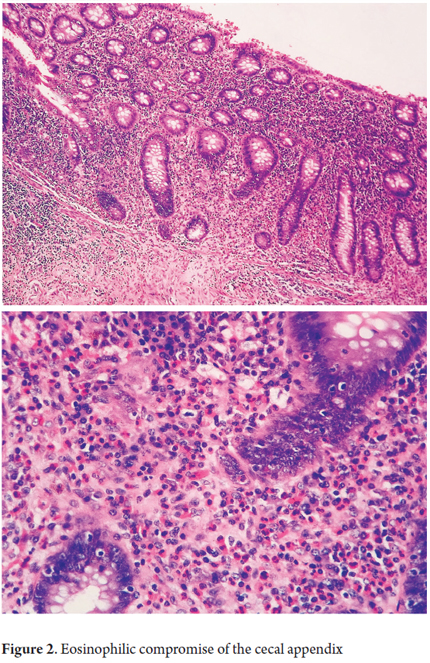
Microscopic examination will find dense, predominantly eosinophilic, inflammatory infiltrate in which there can be up to 20 eosinophils per high-power field (Figure 1). This infiltrate is distributed in the lamina propria and may also be accompanied by formation of aggregates in crypt abscesses that permeate the glandular epithelium. These can be distributed in diffuse or nodular patterns and can be accompanied by outbreaks of ulceration of the glandular epithelium with regenerative alterations and severe edema. Tissue damage may extend beyond the mucosa into the muscle and serous layers (Figure 2). In addition, up to 10% the study of mucosal biopsies may show no changes (Figures 3 and 4). At least six biopsies may be required to reach a diagnosis of one segment (15-17).
A large group of diseases must be considered in differential diagnosis. These include parasites such as roundworms and hookworms; reactions to drug such as enalapril, carbamazepine, and clotrimazole; connective tissue diseases including scleroderma, dermatomyositis and lupus; vasculitis syndrome (Churgstrauss Disease and poliarteririts nodosa); celiac disease; eosinophilic leukemia; Crohn's disease and ulcerative colitis (2, 3, 5).
Steroids are the cornerstone for treatment of eosinophilic gastroenteropathy. The most commonly recommended is prednisone at a dosage of 1-2 mg/kg/day for eight weeks. Improvement usually occurs within two weeks. Budesonide has also been widely used, but it does not have enough high impact studies to be recommended (18). Nevertheless, relapses are common with these drugs. When they occur repeated or longer maintenance therapy at low doses is required (3-6, 10).
Although not enough studies have been done about making dietary modification a part of the established therapy, a prospective study of adults with eosinophilic gastroenteropathy conducted by Gonsalves et al. has demonstrated clinical remission with dietary elimination in six weeks. In that study, significant reductions in symptoms, complete histological resolution and endoscopically verifiable normalization of peripheral eosinophilia was achieved in six weeks for three of the seven adults who participated in an empirical food elimination diet. The diet eliminated wheat, corn, eggs, milk, peanuts, fish and seafood (19). Other drugs which have been used in various studies include cromolyn sodium (20, 21), ketotifen (22, 23), montelukast (24, 25) and omalizumab (26), but these drugs have not been shown to have greater efficacy than prednisone (10).
This case demonstrates how correlation of signs, symptoms, history and an appropriate clinical approach make diagnosis of a rare disease possible. This is reflected in the absolute remission of a chronic condition suffered by the patient. It should be noted that the prevalence of this disease is increasing and proper guidance can completely change the prognosis for these patients if we are well informed about this entity.
REFERENCES
1. Kaijser R. Zur Kenntnis der allergischen Affektionen des Verdawungskanal vom standpunkt desi Chirugen aus. Arch Klin Chir 1937; 188: 36-64. [ Links ]
2. Famularo G, Prantera C, Nunnari J, Gasbarrone L. Eosinophilic gastroenteritis in a young man. CMAJ 2011; 183(1): E65-7. [ Links ]
3. Gamarra V, Nova A, Herrera A. Gastroenteritis eosinofílica con ascitis: presentación de un caso clínico. Rev Gastroenterol Perú 2011; 31(2): 173-7. [ Links ]
4. Liao W, et al. A rare case of spontaneous resolution of eosinophilic ascites in a patient with primary eosinophilic gastroenteritis. Chang Gung Med J 2012; 35(4): 354-9. [ Links ]
5. Rocha N, Aponte D, Huertas S, Sabbagh LC. Gastroenteritis eosinofílica: reporte de caso y revisión de la literatura. Rev Medica Sanitas 2011; 14 (2): 8-11. [ Links ]
6. Rodríguez R, Bohórquez M, González I, Torregroza G. Desórdenes eosinofílicos gastrointestinales (DEGI): presentación de dos casos. Rev Col Gastroenterol 2007; 22(2): 138-148. [ Links ]
7. Alnaser S, Aljebreen AM. Endoscopic ultrasound and histopathologic correlates in eosinophilic gastrienteritis. Saudi J Gastroenterol 2007; 13(2): 91-4. [ Links ]
8. Busoni V, et al. Gastroenteropatía eosinofílica: una serie pediátrica. Arch Argent Pediatr 2011; 109(1): 68-73. [ Links ]
9. Martinez D, et al. Colitis eosinofílica. Rev cubana med 2012; 51(1):91-8. [ Links ]
10. Baig M, Qadir A, Rasheed J. A Review of Eosinophilic Gastroenteritis. J NatI Med Assoc 2006; 98: 1616-9. [ Links ]
11. Hepburn IS, Sridhar S, Schade RR. Eosinophilic ascites, an unusual presentation of eosinophilic gastroenteritis: A case report and review. World J Gastrointest Pathophysiol 2010; 1(5): 166-170. [ Links ]
12. Alfadda AA, Storr MA, Shaffer EA. Eosinophilic colitis: epidemiology, clinical features, and current management. Ther Adv Gastroenterol 2010; 4(5): 301-9. [ Links ]
13. Klein NC, Hargrove RL, Sleisenger MH, et al. Eosinophilic gastroenteritis Medicine (Baltimore) 1970; 49(4): 299-319. [ Links ]
14. Roufosse FE, Goldman M, Cogan E. Hypereosinophilic syndromes. Orphanet J Rare Dis. 2007; 2: 37. [ Links ]
15. Bhattacharya B. Chapter 3. Non-Neoplastic disorders of the stomach. Lacobuzio-Donahue CA, Montgomery E. Gastrointestinal and liver pathology. Second edition. Philadelphia: Elsevier; 2012. p. 105-107. [ Links ]
16. Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut 1990; 31(1): 54-8. [ Links ]
17. Lee JH, Rhee PL, Kim JJ, Koh KC, Paik SW, Han JH, Ree HJ, Rhee JC. The role of mucosal biopsy in the diagnosis of chronic diarrhea: value of multiple biopsies when colonoscopic finding is normal or nonspecific. Korean J Intern Med 1997; 12(2): 182-7. [ Links ]
18. Prussin C. Eosinophilic Gastroenteritis and Related Eosinophilic Disorders. Gastroenterol Clin N Am 2014; 43: 317-27. [ Links ]
19. Serrano OJ, Bonilla RA. Colitis eosinofílica perforada. Med UIS 2010; 23: 255-8. [ Links ]
20. Gonsalves N, Doerfler B, Yang G, Hirano I. A prospective clinical trial of six food elimination diet or elemental diet in the treatment of adults with eosinophilic gastroenteritis. Gastroenterology 2009; 136(5): A280. [ Links ]
21. Van Dellen RG, Lewis JC. Oral administration of cromolyn in a patient with protein-losing enteropathy, food allergy, and eosinophilic gastroenteritis. Mayo Clin Proc 1994; 69(5): 441-4. [ Links ]
22. Pérez-Millán A, Martín-Lorente JL, López-Morante A, López-Morante A, Yuguero L, Sáenz- Rayuela F. Subserosal eosinophilic gastroenteritis treated efficaciously with sodium cromoglycate. Dig Dis Sci 1997; 42(2): 342-4. [ Links ]
23. Melamed I, Feanny SJ, Sherman PM, Roifman CM. Benefit of ketotifen in patients with eosinophilic gastroenteritis. Am J Med 1991; 90(3): 310-4. [ Links ]
24. Bolukbas FF, Bolukbas C, Uzunkoy A, Baba F, Horoz M, Ozturk E. A dramatic response to ketotifen in a case of eosinophilic gastroenteritis mimicking abdominal emergency. Dig Dis Sci 2004; 49(11-12): 1782-5. [ Links ]
25. Neustrom MR, Friesen C. Treatment of eosinophilic gastroenteritis with montelukast. J Allergy Clin Immunol 1999; 104(2Pt 1): 506. [ Links ]
26. Quack I, Sellin L, Buchner NJ, et al. Eosinophilic gastroenteritis in a young girl--long term remission under Montelukast. BMC Gastroenterol 2005; 5: 24. [ Links ]
27. Foroughi S, Foster B, Kim N, et al. Anti-IgE treatment of eosinophil-associated gastrointestinal disorders. J Allergy Clin Immunol 2007; 120(3): 594-601. [ Links ]











 text in
text in