Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.1 Bogotá jan./mar. 2015
Percutaneous Endoscopic Gastrostomy in elderly, indications, safety and outcomes
Diana Patricia Atencio (1), Ángela Gabriela Blanco Pérez (1), William Otero Regino MD. (2)
(1) Fourth year residents in Geriatrics at the National University of Colombia in Bogotá, Colombia.
(2) Professor of Medicine in the Gastroenterology Unit at the National University of Colombia and Gastroenterologist at the Clínica Fundadores in Bogotá, Colombia.
Received: 23-07-14 Accepted: 02-02-15
Abstract
Introduction: Percutaneous endoscopic gastrostomies (PEG) are performed more and more frequently in elderly patients suffering from problems with swallowing. The procedure is used regardless of patients' physical, mental and functional status, but little is known about complications and outcomes here in Colombia.
Objective: The purpose of the study is to determine indications for performance of PEG, rate of complications, and outcomes in short and long term follow-ups (five years).
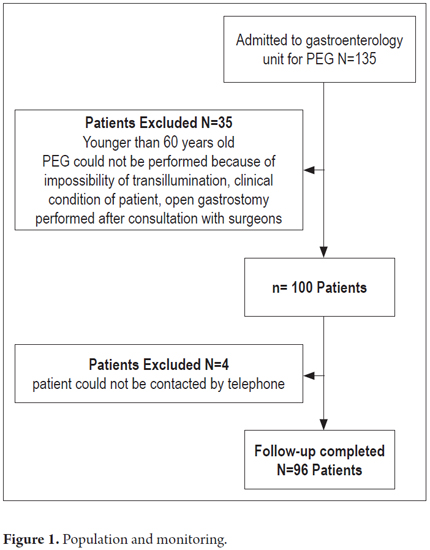
Patients and methods: This is a retrospective and descriptive study of patients over the age of 60 who were hospitalized for percutaneous endoscopic gastrostomy at the Clínica Fundadores between January 2008 and June 2013. Patients younger than 60 years of age, those who had open gastrostomies, and those whose PEG procedure failed were excluded. Patients medical records were reviewed and telephone follow-ups of patients were conducted.
Results: Of the 135 patients with indications for PEG, 96 patients were included. The mean age was 77.5 ± 9 years, and 38 of the patients were men (39.5%). The reasons for performance of PEG were inability to swallow due to a cerebrovascular event (32.89%), dementia (30.26 %) and other causes (36.85). Hypertension was the most common comorbidity. The most common complications associated with PEG were gastrointestinal symptoms (32.9%). There was no mortality associated with the procedure.
Conclusions: PEG is a safe way for elderly patients to receive enteral tube feeding (ETF), but we found no benefit for patients with dementia. Interdisciplinary management prior to the procedure is important to determine whether or not ETF should be used for elderly patients.
Keywords
Elderly, percutaneous endoscopic gastrostomy, complications.
INTRODUCTION
Today, growth of the elderly population is a reality. It is estimated that the world's over 60 population will have doubled from 11% in 2006 to 22% by 2050. In the Americas one in five people will be over 65 years of age (1). In Colombia people over the age of 60 account for 10.5% of the total population (2). With increasing life expectancy the occurrence of chronic diseases and nutritional problems increases and along with them, social and family burdens and use of economic resources increase (1, 2). In this age group the risk of malnutrition risk is high primarily because of the limitation of food intake due to various morbidities, polypharmacy, dental problems, disabilities, depression, isolation and poverty (3).
Nutritional disturbances occur in up to 86% of all patients with dementia (4). Part of the integral management of elderly patients consists of nutritional assessments and support (3, 4). Throughout the world, percutaneous endoscopic gastrostomy (PEG) has had a great impact since its initial description in 1980 (5). Its safety, simplicity and efficiency provides a potent method of treating people with swallowing disorders who have intact digestive systems and whose disorder is expected to last more than one month (6, 7). Although this group includes terminally ill patients and patients in advanced stages of chronic neurological diseases, there is little good quality evidence to support the use of PEG for treating these patients (8, 9). Skelly, et al. (10) have found that the number of gastrostomies performed in the United States increased from 61,000 in 1988 to 121,000 in 1995 and that in the UK the administration of enteral nutrition at home increased 6.5% from 2004 to 2005 and that 82% of those receiving enteral nutrition at home were adults who had undergone PEG (11). In 2005, the British Artificial Nutrition Survey (BANS) (11) report stated that over 65% of PEG were performed in patients over the age of 60 years and about 45% were performed in patients over the age of 70 years.
Currently we do not have data about Latin America. PEG is indicated when there is decreased food intake due to neurological processes that produce neuro-motor dysphagia, dementia, stroke, amyotrophic lateral sclerosis, multiple sclerosis, and Parkinson's disease, among others (12-14). It is also indicated for tumor diseases in the oropharyngeal cavity, neck and esophagus (15). There are other less common indications such as decompression of the upper gastrointestinal tract in advanced carcinomas, extensive burns, cystic fibrosis, advanced AIDS and very serious trauma (12, 16).
The ideal is to determine whether or not a patient can benefit from the PEG before performing the procedure (10). This includes determining the patient's chances of surviving more than 30 days after the procedure is performed (9). There is evidence that patients with stroke sequelae and those with head and neck malignancies undergoing treatment with radiation therapy and/or chemotherapy can benefit from PEG (14, 15, 17). In contrast, the benefit of a PEG is questionable for patients with advanced dementia and dysphagia or a rapidly progressing disease because there is no evidence that PEG improves survival, quality of life, or nutritional status but it can reduce the risk of aspiration and pressure ulcers (13, 18). Nevertheless, PEG is considered to be a safe procedure with low morbidity rates (3% to 12%) and mortality rates (0% to 2%) (16, 17, 19, 20).
Major complications occur in 3% of patients who undergo PEG. These complications include necrotizing fasciitis, buried bumper syndrome (21), peritonitis, gastro-esophageal perforation and gastrocolic fistulas and colocutaneous fistulas. Minor complications occur later, but more frequently. They include local infections and/or cellulitis, drainage of gastric contents, bleeding, pneumoperitoneum, obstruction or displacement of the feeding tube, gastric ulcers and gastrointestinal discomfort at the start of feeding including vomiting, diarrhea and straining (10, 19, 20). Although enteral nutrition is proposed as a therapeutic measure, there is currently controversy over whether it should be part of the basic support for patients with terminal diseases (22, 23). A doctor who is unfamiliar with interventions at the end of a patient's life may make decisions which go against the best quality of life for a particular patient (22, 23). Management of these patients requires an interdisciplinary team in which the specialists in geriatrics and gastroenterology must be key decision making figures.
Taking into account that PEG is available and offered by most hospitals in Colombia, and that there are no studies of the long-term outcomes of PEG among elderly patients, we decided to conduct this study of the rate of complications and outcomes in the short term among patients who are over 60 years of age who have undergone the procedure in order to better determine indications for performing PEG.
PATIENTS AND METHODS
This study was conducted in the Gastroenterology and Digestive Endoscopy Unit of the Clínica Fundadores between January 2008 and June 2013. The study population included patients older than 60 years of age who had undergone PEG. We excluded patients who were younger than 60 and those older than 60 years who had previously undergone gastrostomy surgery, had undergone an unsuccessful PEG, and whose data were incomplete. We retrospectively reviewed patients' medical records and then contacted them or their caregivers for an interview using a questionnaire designed for data collection from patients who met the inclusion criteria. The data were tabulated in Excel and analyzed to verify validity.
PERCUTANEOUS ENDOSCOPIC GASTROSTOMY TECHNIQUE
PEG procedures were conducted in the usual way in the endoscopy unit using a 20Fr Kimberly gastrostomy kit which costs 780,000 Colombian pesos. The technique used has been described previously (7, 24). PEG procedures were performed without sedation in 90% of the patients.
STATISTICAL ANALYSIS
The population under study was described with descriptive statistics for socio-demographic variables.
Comparisons between groups and estimations of relationships found in the descriptive analysis were done with logistic regression used as an econometric tool. In some cases the groups were compared using Student's T test which compares the average of the variable of interest of both groups and determines whether the difference between them is statistically different from zero. The logit model is commonly used to predict the probability of an event whose occurrence depends on other factors when the event and the majority of factors studied are measured with dichotomous variables (variables that take only two values (0 and 1) as in the case of this study.
The coefficients estimated for each factor or independent variable were converted into odds ratios (OR) for interpretation. These are read as the proportional change that occurs in the probability of occurrence of the event under study for each unit change in the independent variable or factor in question.
ETHICAL CONSIDERATIONS
According to the definitions in Resolution No. 8430 of 1993, no interventions that put patients' lives at risk occurred during this study which collected data through reviews of medical records and endoscopic procedure reports and through telephone interviews. Therefore, this study was classified as "safe research" which does not require informed consent from patients.
RESULTS
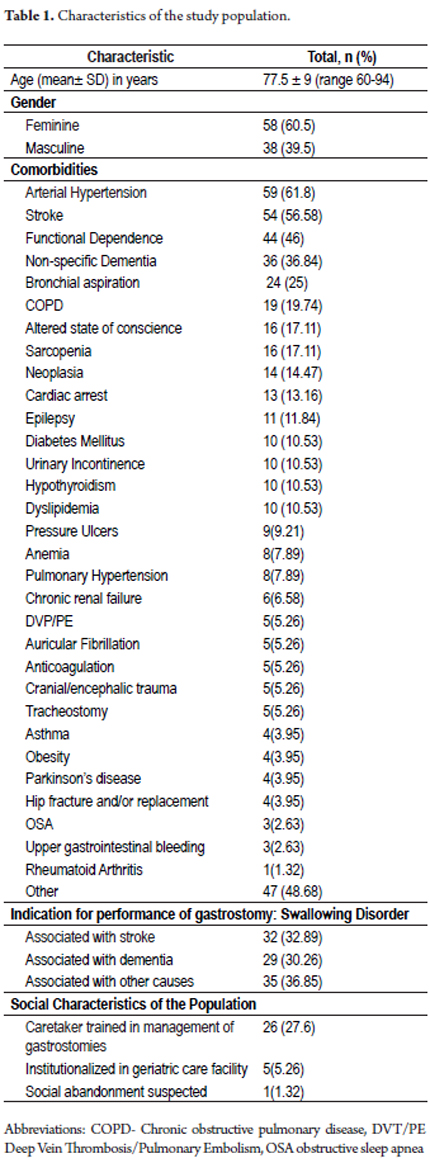
During the study period, performance of PEG procedures was requested 135 times from the Gastroenterology and Digestive Endoscopy Unit of the Clínica Fundadores in Bogotá. Of these, 100 were performed and follow-ups were done on 96 patients (Figure 1). Of these 96 patients, 38 were male (39.5%). The average age of the study population was 77.5 ± 9 years (range 60 to -94 years) (Table 1).
Indications for the procedure and patients' comorbidities are shown in Table 1.
In the study population, five patients (5.26%) had tracheostomies at the moment of the PEG procedure, five patients were receiving anticoagulants which were suspended before the procedure. 27.6% of the patients had health care personnel who were in charge of their gastrostomies, 5.26% came from nursing homes and/or chronic care units, and 1.32% had a diagnosis of "suspicion of social abandonment" (Table 1).
Of the patients included, 66 patients (68.42%) required re-hospitalization for medical reasons not directly related to technical aspects of the procedure. Among readmission diagnoses, the most important were urinary tract infections, aspiration pneumonia, functional decline, and breathlessness. Table 2 shows the frequency of occurrence of these diagnoses.
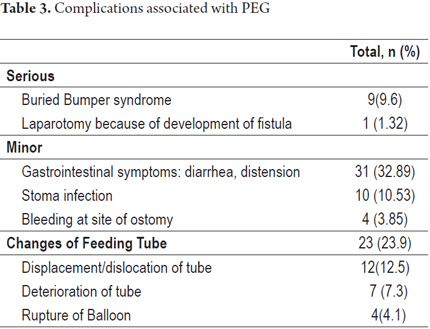
Forty patients (41.67%) required at least one hospitalization after PEG. Thirty-one (32.89%) had gastrointestinal symptoms such as diarrhea and bloating. Ten (10.53%) superficial infections at the site of the PEG that did not require removal. Nine (9.6%) had buried bumper syndrome, four (3.85 %) had minor bleeding at the site of the gastrostomy which was controlled by injecting adrenaline. Twenty-three (23.9%) of the 96 patients had their gastrostomy tubes changed. Of these, twelve (12.5%) tubes were simply displaced, and seven (7.3%) had tubes that had deteriorated. In four cases (4.1%) the balloon ruptured when the tube was replaced (Table 3).
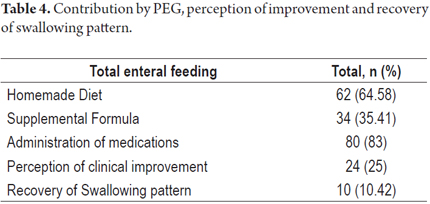
Sixty-two patients (64.58%) of patients with enteral feeding tubes received diets prepared at home while 34 (35.6%) received nutritional supplement formula. Drugs were administered through the feeding tube to eighty patients (83%). In twenty-four cases (25%) either the patient or caregiver perceived improvements in the patient's clinical condition after PEG, but only ten patients' (10.42%) swallowing patterns improved during follow-up (Table 4).
Thirty-seven (38.16%) of the 96 patients died after the PEG. Of this group, six (16.22%) died between day 0 and day 5 following PEG. Eight (21.62 %) died between day 11 and day 30, and twenty-three (62.16%) died after thirty days had passed. The average time between PEG and death was 68.7 days. Neither the patients' medical records nor the study's telephone interviews were able to document any direct relation between PEG and causes of death (Table 5).
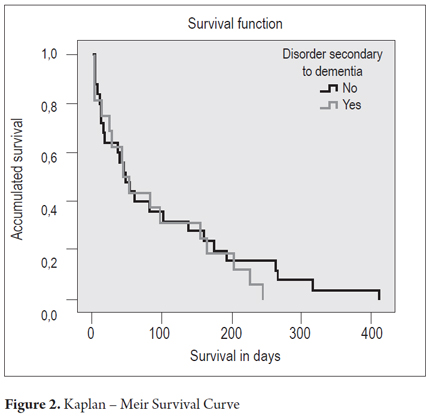
Figure 2 shows that patients who underwent PEG for reasons other than dementia had better survival times than those who underwent PEG for reasons associated with dementia.
Logistic regression analysis showed that the probability of dying after PEG is three times greater for patients whose indication for the procedure was a swallowing disorder associated with dementia (The difference is significant at 5%). This reflects the fact that fifteen (51.7%) patients who underwent PEG because of swallowing disorders associated with dementia died after the procedure. Four (26.6%) of these died within 5 days of the procedure. Patients who underwent PEG because of swallowing disorders associated with stroke or other causes had a death rate of 32.8% (n = 22). Two (9.52%) died within 5 days of the procedure (Table 6).
None of the patients whose indication for PEG was a swallowing disorder associated with dementia showed improvement in the swallowing process after completion of the PEG while ten patients (15%) subjects who underwent this procedure because of swallowing disorders associated with strokes or other causes did improve (significant difference at 5%) (Table 7).
Of the 31 patients who developed gastrointestinal symptoms, eighteen (59%) had undergone PEG because of symptoms related to dementia, and thirteen (41%) were patients with swallowing disorders associated with other causes (Table 8).
DISCUSSION
To date, this is the largest study to evaluate post-PEG clinical outcomes among elderly patients in Colombia. The indications for PEG in this study were classified into 3 groups: swallowing disorders associated with acute strokes (32.88%), dementia (30.26%) and other causes (47.37%). The last category included head and neck cancer, cranial-cerebral trauma, tracheoesophageal fistulas, sequelae of hypoxic ischemic encephalopathy, cardiac arrest, and compromised swallowing resulting from diseases of the central nervous system,. This is similar to other international studies including a Peruvian study (20, 25, 26). The frequency of occurrence of these indications varies according to the age of the patients, but swallowing disorders associated with dementia are very common among the elderly (26, 27).
Our study found that the most frequent comorbidities among the elderly patients who had undergone PEG were hypertension (61.8%), acute strokes (56.58%), functional dependence (46%), and dementia (36.84%). There was at least one episode of aspiration (25%) which agrees with the results of other authors (20, 29). Complications directly related to PEG occurred during follow-up in 26% of the patients. Mild infections of the stoma that did not require the removal of the probe occurred in 10.53% of the patients. Occurrence of this complication in other studies varies between 6.9% (19) at 31.2% (7, 16, 25). Another minor complication was bleeding at the feeding tube insertion which occurred in 3.85% of the patients. This was controlled in all cases by injection of adrenaline. This complication is similar to that found in other series (20).
The only major complication found in this cohort was buried bumper syndrome which occurred in approximately 10% of patients which is more than occurred in other studies (30, 31). This complication is usually caused by improper handling of the feeding tube by caregivers or accidental pulling by the patient (21). Its impact varies from population to population but is related to whether or not there is endoscopic monitoring of patients and to mortality rates related to underlying diseases (21, 31).
Overall, PEG-related complications occurred in 41.7% of the patients in this study which is a larger proportion than that found in other studies (17, 20, 29). Nevertheless, it should be noted that these were managed by the hospital management in less than two days. Diarrhea and abdominal distension were the most frequent complications, occurring in 32.89% of cases. These were probably related to the type of nutrition provided. The 40% rate of occurrence of these complications in other studies is higher the rate found in this study (19). In our study no patient developed adverse cardiorespiratory events between admission to the procedure room and discharge, nor were there any major complications such as abscesses, severe bleeding, peritonitis, massive aspiration or pneumothorax which have been described in other studies. Similarly, and in contrast to other studies, there were no cases of mortality directly related to the procedure in our study (8,17,25,29,32).
Feeding tubes were changed 23.9% of the patients in our study: 12.5% because the tubes had been displaced, 7.3% because the tubes had deteriorated, and 4.1% because of balloon rupture. These are considered to be minor mechanical complications (19). A study from the in the hospital in Alicante, Spain (19) reported that the feeding tubes were lost in 10.3% of the cases studied, and in 1.7% of cases, feeding tubes were lost more than once. Gundogan, et al. reported that 12% of patients required feeding tube changes due to malfunctions, displacement or extravasation of gastric contents (20). Chicharro found that tubes were accidentally lost in 25% of the cases studied (17). The differences in these results may be due to the significant number of patients with dementia in the Spanish study since behavioral disorders that can cause traumatic extraction of the feeding tube are often associated with dementia (33-35).
In our study, 38.16% of the patients died after PEG. Within this group, 17.24% died between day 0 and day 5, 20.69% died between day 11 and day 30, and 62.12% died more than 30 days after the procedure. While this rate is higher than that found in most series (36-39), it is similar to that in the study by Gundogan (20). The most likely explanation is that the larger the number of patients dementia, the larger the number of patients with advanced and/or terminal conditions. The Kaplan Meir curve found that the patient survival rate is lower when PEG was performed because of a swallowing disorder associated with dementia than when it is performed because of other alterations. Given that approximately 40% of patients died within the first month after PEG, and that most patients with this outcome had dementia, it is advisable that the decision to perform this procedure be made by a multidisciplinary board since a PEG kit is costly in Colombia.
The relevance of PEG for patients with advanced dementia should be assessed in light the high probability of death among these patients and the debatable benefits from this procedure (23). This is especially true because other studies have not shown clear benefits from PEG for patients with dementia (13, 43). Pathophysiologically, enteral nutrition increases gastric secretions and the occurrence of fecal and urinary incontinence and pressure ulcers (43). Some authors consider that PEG and nutritional support only prolongs the process of dying for these patients (44). Some believe that the decision to perform PEG in a patient with dementia should be made according to ethical considerations (45-49). Scientific societies like ESPEN do not recommend this type of nutrition for people with severe dementia (50).
As in other studies spontaneous recovery of the ability to swallow normally occurred 10.53% of the patients in our study. (19, 20) Feeding tubes were removed successfully from these patients, but this did not happen in any of the patients with advanced dementia.
Our study has the limitations of a retrospective study performed in a single institution which means that the results cannot be generalized.
Based on our results, we conclude that the PEG procedure is a technically safe and easy procedure but with potential complications during long-term follow up, and that no benefits were found when the procedure was performed because of swallowing disorders associated with dementia.
Financing
The costs of this work were borne entirely by the authors.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
We wish to extend our gratitude to the Gastroenterology and Digestive Endoscopy Unit of the, Liver of Founders Clinic for allowing us access to the gastrostomy reports and medical records that were used in this study. We also want to express special thanks to Andrea Atencio De Leon for organization of the database and statistical analysis and to Liliana Oino, a gastroenterology assistant and a student in biomedical engineering, for her diligence and promptness in making available medical records and the database of patients used for this study.
REFERENCES
1. United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2013. [ Links ]
2. DANE (Departamento Administrativo Nacional de Estadística). Estimación y proyección nacional, departamental y municipal total por área 1985-2020. Disponible en: http//www.dane.gov.co, consultado en enero de 2014. [ Links ]
3. John BK, Bullock M, Brenner L, McGaw C, Scolapio J. Nutrition in the elderly. Frequently asked question. Am J Gastroenterol 2013;108:1252-66. [ Links ]
4. Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG, et al. The clinical course of advanced dementia. N Engl J Med 2009;361:1529-1538. [ Links ]
5. Gauderer MWL, Ponsky Jl, Izant J. Gastrostomy without laparotomy, a percutaneous technique. J Pedriatr Surg 1980;15:872-5. [ Links ]
6. Volkert D, Berner YN, Berry E, Cederholm T, Coti BP, Milne A. et al. ESPEN (European Society for Parenteral and Enteral Nutrition). Guidelines on Enteral Nutrition: Geriatrics. Clin Nutr 2006;25:330-60. [ Links ]
7. Sebastian JJ. Gastrostomía endoscópica percutánea. Técnica e indicaciones. Endocrinol Nutr. 2004;51:158-62. [ Links ]
8. Pereira JL, Belda O, Parejo J, Serrano P, Bozada JM, Fraile J, et al. La gastrostomía endoscópica percutánea. Realidad en la práctica nutricional clínica intra y extrahospitalaria. Rev Clin Esp 2005;205:472-7. [ Links ]
9. Razavi F, Gross S, Katz S. Endoscopy in the elderly: Risks, benefits, and yield of common endoscopic procedures. Clin Geriatr Med 2014;30:133-47. [ Links ]
10. Skelly R. Are we using percutaneous endoscopic gastrostomy appropriately in the elderly? Curr Opin Clin Nutr Metab Care 2002;5:35-42. [ Links ]
11. Jones B, Holden C, Dalzell M, Micklewright A, Glencorse C. Annual BANS Report Artificial Nutrition Support in the UK 2005. A Report by the British Artificial Nutrition Survey (BANS), a committee of BAPEN (The British Association for Parenteral and Enteral Nutrition) UK 2005:13-17. [ Links ]
12. Slater R. Percutaneous endoscopic gastrostomy feeding: Indications and management. Brit J Nur 2009;18:1036-43. [ Links ]
13. Sampson EL, Candy B, Jones L. Enteral tube feeding for older people with advanced dementia. Cochrane Database of Systematic Reviews. 2009;2:1-25. [ Links ]
14. Britton JE, Lipscomb G, Mohr PD, Rees WD, Young AC. The use of percutaneous endoscopic gastrostomy (PEG) feeding tubes in patients with neurological disease. J Neurol 1997;244:431-4. [ Links ]
15. Saunders J, Brown MS, Hirata RM, Jaques DA. Percutaneous endoscopic gastrostomy in patients with head and neck malignancies. Am J Surg. 1991;162:391-93. [ Links ]
16. Erdogan A. Single endoscopist-performed percutaneous endoscopic gastrostomy tube placement. World J Gastroenterol 2013;19:4172-6. [ Links ]
17. Chicharro L. Complicaciones inmediatas de la gastrostomía percutánea de alimentación: 10 años de experiencia. Nutr Hosp 2009;24:73-6. [ Links ]
18. Gillick MR. Rethinking the role of tube feeding in patients with advanced dementia. N Engl J Med 2000;342:206-10. [ Links ]
19. Wanden-Berghe C, Muñoz J, Cantó C, Domenech MD, Reyes MD, Pérez Moya C. Gastrostomía Endoscópica Percutánea (PEG): 10 años de experiencia. Nutr Hosp 2010;25:949-53. [ Links ]
20. Gundogan K, Yurci A, Coskun R, Baskol R, Gursoy S, Hebbar G, et al. Outcomes of percutaneous endoscopic gastrostomy in hospitalized patients at a tertiary care center in Turkey. Eur J Clin Nutr 2014;68:437-40. [ Links ]
21. Moreno N, Otero W, Gómez M. Síndrome de "buried bumper" (botón interno de la gastrostomía enterrado): desenterrando la solución. Rev Col Gastroenterol 2007;22:51-7. [ Links ]
22. Cardin F. Special considerations for endoscopists on PEG indications in older patients. ISRN ISRN Gastroenterol 2012;2012:60714. [ Links ]
23. Peñaloza A, Suárez J, Blanco L, Peñaloza A. Gastrostomía endoscópica percutánea: ¿Es éticamente aceptable? Rev Col Gastroenterol 2013;28:150-60. [ Links ]
24. Chang WK, Hsieh TY. Safety of percutaneous endoscopic gastrostomy in high-risk patients. J Gastroenterol Hepatol 2013;28(Suppl 4):118-22. [ Links ]
25. Yriberry S, Monge V, Cabrera F, Barriga E, Vesco E. Gastrostomía endoscópica percutánea: experiencia prospectiva de un centro privado nacional. Rev Gastroenterol Perú 2004;24:314-22. [ Links ]
26. Elia M, Russell CA, Stratton RJ, Shaffer J, Micklewright A, Wood S, et al. Trends in artificial nutritional support in the UK during 1996-2000. A report by the British Artificial Nutrition Survey (BANS). British Association of Parenteral and Enteral Nutrition. Maidenhead, UK: BAPEN 2001. [ Links ]
27. Mendiratta P, Tilford JM, Prodhan P, Curseen K, Azhar G, Wei JY. Trends in percutaneous endoscopic gastrostomy placement in the elderly from 1993 to 2003. Am J Alzheimers Dis Other Demen 2012;27:609-13. [ Links ]
28. Malmgren A, Hede G, Karlström B, Cederholm T, Lundquist P, Wirén M, et al. Indications for percutaneous endoscopic gastrostomy and survival in old adults. FoodNutr Res 2011;55:6037-42. [ Links ]
29. McClave SA, Chang WK. Complications of enteral access. Gastrointest. Endosc 2003;58:739-51. [ Links ]
30. Finocchiaro C, Galleta R, Rovera G, Ferrari A, Todros L, Vuolo A, et al. Percutaneous endoscopic gastrostomy a long term follow-up. Nutrition 1997;13:520-3. [ Links ]
31. Meine G, Lukashok H, Mello G, Mansur G, Guimarães D, Carvalho R, et al. Buried Bumper Syndrome as a complication of percutaneous endoscopic gastrostomy in cancer patients: The brazilian experience. Digest Endosc 2007;19:22-5. [ Links ]
32. Schrag S, Sharma R, Jaik N, Seamon M, Lukaszczyk J, Martin N, et al. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis 2007;16:407-18. [ Links ]
33. Warren J, Rohrer J. Frontotemporal dementia. BMJ 2013;347:4827-35. [ Links ]
34. Ahronheim JC, Mulvihill M, Sieger C, Park P, Fries BE. State practice variations in the use of tube feeding for nursing home residents with severe cognitive impairment. J Am Geriatr Soc 2001;49:148-52. [ Links ]
35. Mitchell SL, Teno JM, Roy J, Kabumoto G, Mor V. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. JAMA 2003;290:73-80. [ Links ]
36. López L, Iñiguez F, Santos E, Balado M, Pérez-Carnero A. Gastrostomía percutánea endoscópica. Experiencia en un hospital general. Rev Esp Enferm Dig 1994;85:173-6. [ Links ]
37. Martín A, Espinós J, Forné M, Rius J, Corbera G, Quintana S, et al. Gastrostomía endoscópica percutánea: estudio de 35 enfermos. Med Clin 1994;103:449-51. [ Links ]
38. Park R, Allison M, Lang J, Spence E, Morris A, Danesh B, et al. Randomised comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with persisting neurological dysphagia. BMJ 1992;304:1406-9. [ Links ]
39. Gencosmanoglu R, Koc D, Tozun N. Percutaneous endoscopic gastrostomy: results of 115 cases. Hepatogastroenterology 2003;50:886-8. [ Links ]
40. Kaw M, Sekas G. Long-term follow-up of consequences of percutaneous endoscopic gastrostomy (PEG) tubes in nursing home patients. Dig Dis Sci 1994;39:738-43. [ Links ]
41. Callahan C, Haag K, Weinberger M, Tierney WM, Buchanan NN, Stump TE, et al. Outcomes of percutaneous endoscopic gastrostomy among older adults in a community setting. J Am Geriatr Soc 2000;48:1048-54. [ Links ]
42. Mccann R, Hall W, Groth-Juncker A. Comfort care for terminally ill patients. The appropriate use of nutrition and hydration. JAMA 1994;272:1263-6. [ Links ]
43. Candy B, Sampson E, Jones L. Enteral tube feeding in older people with advanced dementia: Findings from a Cochcrane systematic review. Int J Palliative Nurs 2009;55:396-404. [ Links ]
44. Morgenstern L, Laquer M, Treyzon L. Ethical challenges of percutaneous endoscopic gastrostomy. Surg Endosc 2005;19:398-400. [ Links ]
45. Sanders D, Carter M, D'Silva J, James G, Bolton R, Bardhan K. Survival analysis in percutaneous endoscopic gastrostomy feeding: A worse outcome in patients with dementia. Am J Gastroenterol 2000;95:1472-5. [ Links ]
46. Nair S, Hertan H, Pitchumoni CS. Hypoalbuminemia is a poor predictor of survival after percutaneous endoscopic gastrostomy in elderly patients with dementia. Am J Gastroenterol 2000;95:133-6. [ Links ]
47. Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact of survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med 1997;157:327-32. [ Links ]
48. Murphy LM, Lipman TO. Percutaneous endoscopic gastrostomy does not prolong survival in patients with dementia. Arch Intern Med 2003;163:1351-3. [ Links ]
49. Dharmarajan TS, Unnikrishnan D, Pitchumoni CS. Percutaneous endoscopic gastrostomy and outcome in dementia. Am J Gastroenterol. 2001;96:2556-2563. [ Links ]
50. Körner U, Bondolfi A, Bühler E, MacFie J, Meguid M, Messing B, et al. Ethical and legal aspects of enteral nutrition. ESPEN guidelines. Clin Nutr 2006;25:196-202. [ Links ]











 texto em
texto em