Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.1 Bogotá Jan./Mar. 2015
Management of Esophageal Stenosis Due to Histoplasma with Self-expanding Metal Stents
René Marcelo Escobar P. MD. (1), Mónica Restrepo J, MD. (2)
(1) Specialist in Digestive Endoscopy and Gastrointestinal Surgery at the Hospital Universitario San Vicente in Medellin, Colombia. Email: remar_med@hotmail.com
(2) Second Year Resident in General Surgery at the Universidad de Antioquia in Medellin, Colombia. Email: monica626_1@hotmail.com
Received: 03-05-14 Accepted: 02-02-15
Abstract
Benign esophageal strictures are a common cause of medical consultation and gastroenterological endoscopy. Usually, given their non-neoplastic nature, they have been managed with recurrent endoscopic dilation which is uncomfortable for the patient and which generates high costs due repetition. In addition, there is always the risk of esophageal perforation at every session. The use of esophageal stents for management of benign esophageal strictures is becoming increasingly more common and is promising for various etiologies. We present a case of a benign esophageal stricture secondary to infection with histoplasma capsulatum which was managed entirely with a completely covered metal stent. This led to complete resolution of the obstruction.
Keywords
Histoplasma capsulatum, benign esophageal stricture, esophageal prosthesis.
INTRODUCTION
Esophageal infections by opportunistic pathogens have increased in frequency due to the increased number of patients with some degree of immunosuppression. Candida albicans is the most common, but other fungi reported to cause infections are Aspergillus, Histoplasma and Blastomyces. All of these should be considered in patients with esophageal infections who have any degree of immunosuppression and in patients who do not respond to antibiotic treatment.
Cases of esophageal strictures have been reported following fungal infections of the esophagus. These cases have usually been managed with serial endoscopic dilation and/or surgery. The advent of esophageal stents has opened the possibility of avoiding the complications of serial dilations while obtaining satisfactory results in the treatment of malignant esophageal strictures. Nevertheless, convincing evidence of any similar great advantages of the use of stents to treat benign strictures has not yet been demonstrated.
CLINICAL CASE DESCRIPTION
The patient was a 24 year old man who lived in a rural area of the department of Antioquia in Colombia. He came to the Hospital Universitario San Vicente Fundación in Medellín, Colombia after two months of suffering from fatigue, weakness, left hemiparesis, weight loss, night sweats, fever, loose stools, urinary incontinence and abdominal pain in the epigastrium. In the eight days prior to admission, he had suffered from loss of appetite, whitish lesions in his mouth, a sore throat, hyperpigmented lesions on his left arm and hypopigmented lesions on his legs.
He had consumed cannabinoids and smoked tobacco since the age of 14 and had had heterosexual relations with three partners without the use of condoms since he began engaging in sexual activity. He had suffered head trauma and a drug overdose two years previously.
Upon physical examination the patient was found to be hemodynamically stable but had a fever, cachexia, and lymphadenopathy of the neck, right axilla and popliteal fossae. His oral cavity had whitish lesions compatible with thrush. Widespread crackles could be heard throughout his lungs. A neurological assessment showed him to be disoriented and hypertonic with left arm spasms. He had hypertrophied muscles in all four limbs. Symmetrical movements of his face showed decreased strength on the left side similar to decreased strength in his extremities. He had rounded hyperpigmented lesions about 0.5 cm in diameter on his left arm and hand, ulcerated lesions on his penis, and flat anal warts.
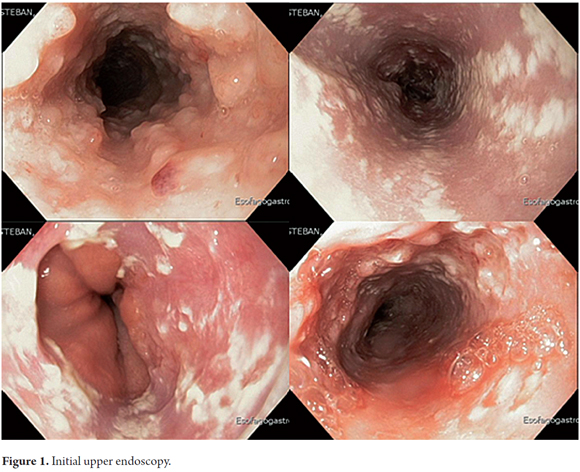
Endoscopy (Figure 1) showed severe circumferential inflammation of the mucosa in the upper and middle third of the esophagus. There were flat, friable pseudopolypoid fibrin-covered ulcers that were three to six mm in diameter and which bled easily. In the distal third of the esophagus there were cotton-like lesions which could not be washed off and which were compatible with Candida. Samples of these lesions were taken for pathological and microbiological examination.
The diagnosis of de novo AIDS with neurosyphilis and oral and esophageal candidiasis was made after testing showed 67,400 copies of the virus and CD73 (+) CD4 (+) T lymphocytes. Biopsies and cultures of from the esophagus and colon reported compromise due to Histoplasma capsulatum. Antiretroviral therapy and fluconazole were begun, but amphotericin B was substituted because of the development of liver toxicity.
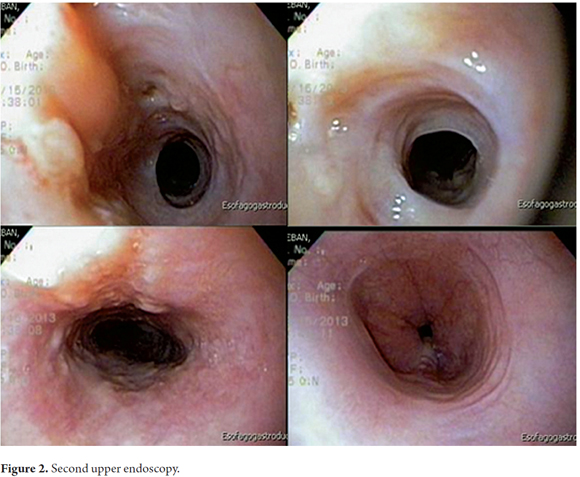
After 15 days of treatment the patient began to suffer from dysphagia and a high fever, so another endoscopy was performed (Figure 2). It found complete improvement of the lesions in the esophageal mucosa although a review of images taken during endoscopy seemed to show an esophageal stricture.
The oral antifungal voriconazole was prescribed and the patient was discharged but continued treatment as an outpatient. Twenty days later he was readmitted because of drooling and increasing difficulty of swallowing to the point that he could barely swallow liquids.
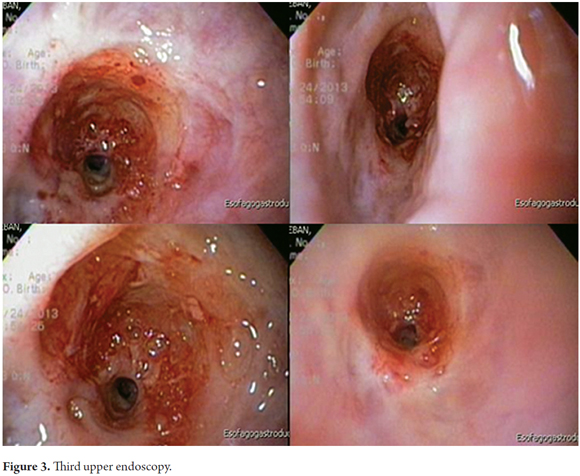
Another endoscopy (Figure 3) showed a marked decrease in the esophageal circumference to a diameter of five mm about twenty cm from the dental arch. The stricture appeared to be fibrous. It was impossible to advance the endoscope farther.
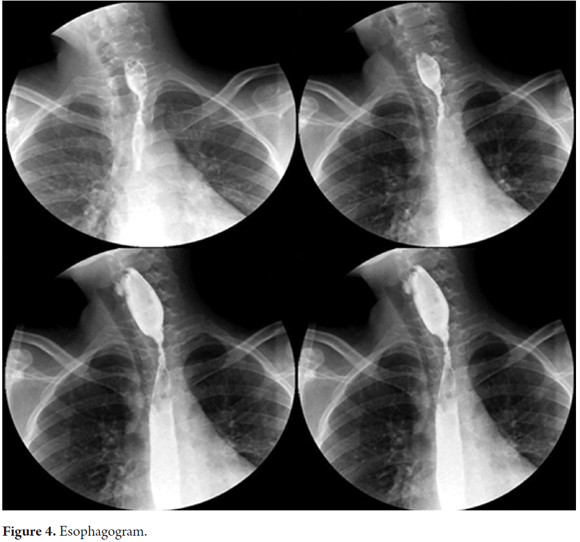
An esophagogram confirmed an esophageal stricture of approximately 3cm in length without prestenotic dilation (Figure 4).
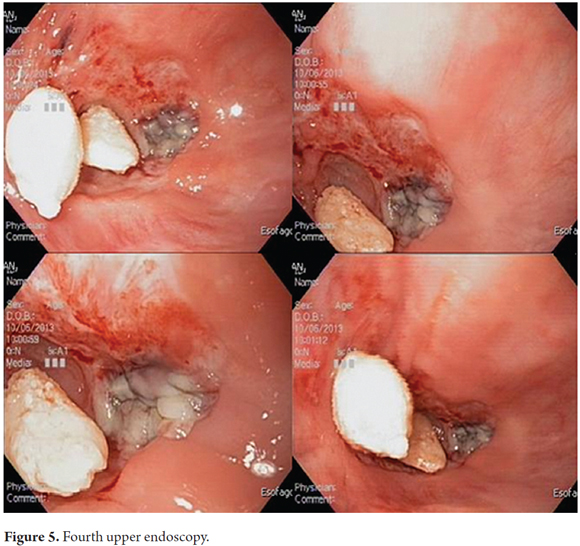
The patient was discharged with a supraglottic diet, antifungal therapy and an order for endoscopic dilation. He was readmitted six days later with severe dysphagia. Another endoscopy (Figure 5) showed a concentric stricture 19cm from the dental arch with a necrotic area on the right esophageal wall and a large number of 2mm to 4mm nodes superimposed on an ulcerated mucosa. The esophagus was impassable at the stricture.
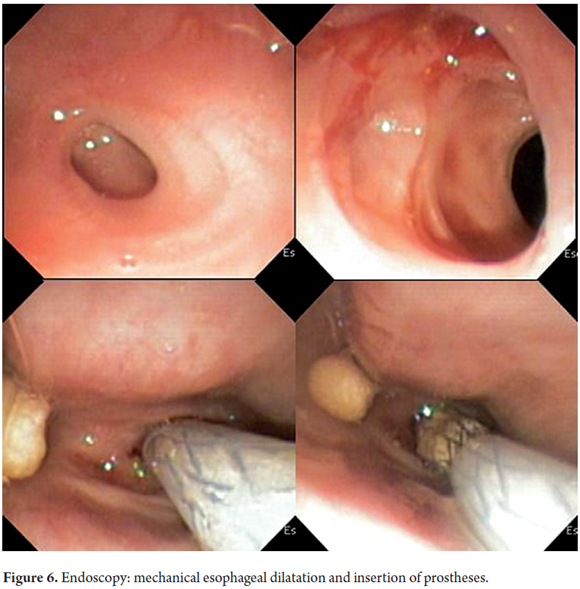
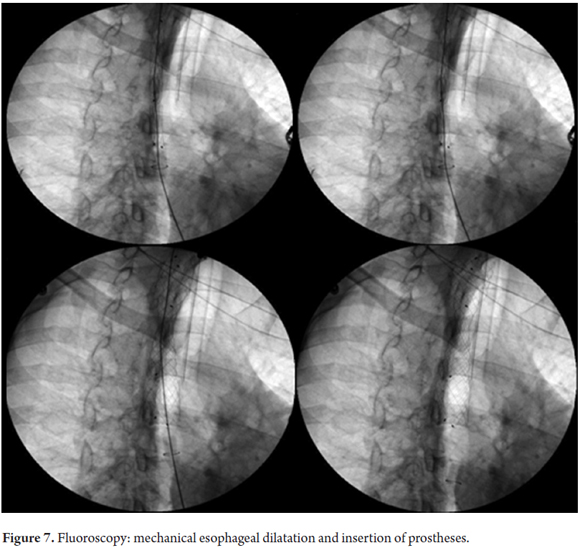
It was decided not to endoscopically dilate the esophagus. Instead a gastrostomy was opened to ensure a proper oral path, and the evolution of the necrotic area in the esophagus was closely monitored. Twenty days later another endoscopy was performed (Figure 6). It found a concentric stricture of the esophagus that was about 3mm in diameter. The mucosa was red and irritated, but there had been a complete resolution of the necrotic area. Under fluoroscopic guidance, dye was endoscopically injected into the area of the stricture for three cm on either side in order to better observe it. Three Savary-Gilliard dilators of 5 mm, 7 mm and 9 mm and a neonatal endoscope were used to dilate the esophagus. The procedure went smoothly, and the stricture was opened without problems until the circumference of the middle and distal thirds were both normal. The esophageal mucosa was also observed to be normal. Finally, an 8cm x 16mm fully covered self-expanding metal esophageal stent was released (TecnoStent, Medellín, Colombia) without complications (Figure 7).
The patient began to tolerate feeding by mouth, so the feeding tube was removed. Antifungal and antiretroviral treatment continued.
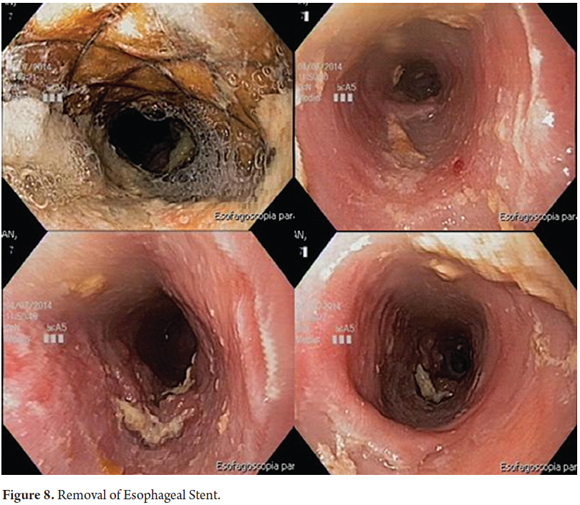
Five months later another upper endoscopy (Figure 8) was performed. It showed the proximal edge of the fully expanded esophageal stent 17cm from the dental arch. Very little food debris had stuck to the inside wall. The endoscope could be advanced without any inconvenience through to o the distal esophagus which was observed to be normal. The prosthesis was easily removed without complication. The endoscopic review showed the caliber of the esophagus to be uniform in its entirety without evidence of stricture. In the area that was covered by the prosthesis the mucosa had thickened secondary to the presence of the foreign body. No active viral or fungal infections were apparent. The esophagus was properly insufflated so there was no suspicion of perforation.
The patient continued to receive normal feeding by mouth and continued his antiretroviral and antifungal treatment which was scheduled to last for 12 months.
DISCUSSION
As the number of immunocompromised patients has increased, so too has the incidence of opportunistic esophageal infections, particularly Candida albicans, herpes simplex, cytomegalovirus and other fungal infections. Candidiasis accounts for the largest number of these cases. The increased numbers of immunocompromised patients is a result of HIV infections and immunosuppressive treatments (1-3).
Half of all fungal infections of the esophagus develop asymptomatically, but the most common symptoms are sudden onset of a sore throat with or without dysphagia, oropharyngeal thrush, chest pain, nausea, heartburn, and gastrointestinal bleeding. Other symptoms which occur much less frequently include fever, sepsis, abscesses and esophageal obstructions. It is not uncommon to find several organs compromised by the same fungal infection in immunosuppressed patients (4-6).
A clinical picture compatible with fungal infections must exist in order to make this diagnosis. Other symptoms and endoscopic findings may be associated with lesions in the oral cavity (7). Together these factors allow physicians to stage infections according to severity. The staging system classically used for candidiasis is as follows:
a. A small number of white plaques smaller than 2 mm in diameter without ulcers
b. A large number of white plaques larger than 2 mm in diameter without ulcers
c. Confluent linear plates with ulceration
d. Confluent linear plates with ulceration and associated stenosis.
Other fungi that are responsible for infections in the oral cavity include Aspergillus, Histoplasma, Blastomyces and other species of Candida. Usually these affect patients with greater degrees of immunosuppression. Aspergillus affects the lungs, and can directly affect areas contiguous to the esophagus and other neighboring organs in severely immunocompromised patients. Aspergillus should be considered in cases assumed to be esophageal candidiasis that do not respond to treatment. Histoplasma and Blastomyces usually affect mediastinal lymph nodes and can spread to the esophagus. Dysphagia due to compression can result from these infections, and there have also been cases of disseminated histoplasmosis with primary compromise of the esophagus.
Complete diagnostic certainty requires histological and microbiological studies of the biopsy samples or samples obtained by brushing the esophagus. Brushing can be guided endoscopically or even done blindly. For diagnosis, the fungus must be in its hyphae or yeast form and must be mixed with epithelial cells which causes an inflammatory reaction. It is worth noting that cytology is usually more than adequate and cultivation of samples from brushing or biopsy results in a high percentage of positive identifications (8). Nevertheless, sometimes it is impossible to distinguish between normal flora and colonization and infection, so everything must be analyzed in the context of the individual patient.
Treatment of patients with relatively intact immune systems includes unabsorbable antifungal agents such as nystatin and clotrimazole. For patients with HIV infections, orally administered absorbable antifungal agents are used. These include fluconazole, ketoconazole, and voriconazole. If the patient cannot swallow, fluconazole or amphotericin B can be administered by injection. Recurrences can be treated with oral fluconazole, ketoconazole or amphotericin B. In patients with neutropenia the risk of dissemination is high, so aggressive antifungal therapy with intravenous amphotericin B should be initiated together with very careful and precise monitoring of renal function. In extreme cases it can 5-fluorocytosine can be combined with amphotericin B (1-6). The literature reports a significant number of cases of esophageal stenosis secondary to fungal infections which have had different outcomes and which have been treated with various pharmacological options (9-17).
The management of benign esophageal strictures has changed significantly in recent years. Logically, the basic treatment for strictures caused by an infectious agent is eradication of the infection with drugs. Nevertheless, since immunosuppressed patients may suffer from dysphagia and subsequent malnutrition, the usual treatment of this complication was to use serial mechanical or pneumatic dilations while waiting for the patient's mouth to return to normal after a few months. Surgical treatment was reserved for cases that did not improve with dilation or who suffered perforation during attempted dilation.
With the advent of the covered esophageal stents, a large number of patients with benign esophageal strictures due to various causes (peptic, actinic and infectious) have been treated satisfactorily without the need for periodic dilations and difficult surgery (18-19).
The clinical case presented here included disseminated histoplasmosis in an HIV positive patient with clinical stage C3 AIDS. Only two other cases of esophageal stricture secondary to infectious compromise due to histoplasmosis were found in the literature available in PubMed (20, 21).
The particular reason point that a series of endoscopic dilations of the stricture was decided against in this case was that the patient had an area of necrosis next to the stricture. The alternative chosen was placement of a fully covered esophageal stent. The final result was satisfactory: the gastrostomy tube could be removed soon after the procedure, and the patient was able to return to a normal diet quickly. Five months after insertion of the stent, the infection and associated lesions were fully resolved although the patient continued to receive antifungal therapy (18, 19).
In conclusion, fully covered esophageal stents have an increasingly important role in the treatment benign strictures of the esophagus. They can be used much earlier in the patient's development and can guarantee quicker resolution of clinical problems while simultaneously decreasing the complication rate that would otherwise result from repeated dilation sessions (22, 23).
REFERENCES
1. Barros C, Berenguer J, Gutiérrez F. Treatment of opportunistic infections in adolescent and adult patients infected by the human immunodeficiency virus during the era of highly active retroviral therapy. Guidelines of the AIDS Study Group (GESIDA)/National AIDS Plan. Enferm Infecc Microbiol Clin 2008;26:356-79. [ Links ]
2. Böhme A, Ruhnke M, Buchheidt D, et al. Treatment of fungal infections in hematology and oncology. Ann Hematol 2003;82(Suppl 2):S133-40. [ Links ]
3. San Juan R, Aguado J, Lumbreras C. Incidence, clinical characteristics, and risk factors of late infection in solid organ transplant recipients: data from the RESISTRA Study Group. Am J Transplant 2007;7:964-71. [ Links ]
4. Slavin M, Szer J, Grigg A. Guidelines for the use of antifungal agents in the treatment of invasive Candida and mould infections. Intern Med J 2004;34:192-200. [ Links ]
5. Vazquez J. Optimal management of oropharyngeal and esophageal candidiasis in patients living with VIH infection. HIV/AIDS Research Palliative Care 2010;2:89-101. [ Links ]
6. Corti M, Villafañe M. The compromise of esophagus in HIV/AIDS diseases. Acta Gastroenterol Latinoam 2003;33(4):211-20. [ Links ]
7. Werneck-Silva A, Bedin I. Role of upper endoscopy in diagnosing opportunistic infections in human immunodeficiency virus-infected patients. World J Gastroenterol 2009;15:1050-6. [ Links ]
8. Wilcox C, Rodgers W, Lanzeby A. Prospective comparison of brush cytology, viral culture, and histology for the diagnosis of ulcerative esophagitis in AIDS. Clin Gastroenterol Hepatol 2004;2:564-7. [ Links ]
9. Chandrasekhara V, Zhang L, Floyd B, Kochman M. A rare cause of esophageal strictures: Actinomyces. Gastrointest Endosc 201275(5):1111-2. [ Links ]
10. Hyun J, Chun H, Keum B, Seo Y, Kim Y, Jeen Y, et al. Candida esophagitis complicated by esophageal stricture. Endoscopy 2010;42(Suppl 2):E180-1. [ Links ]
11. Dahl C, Fuursted K, Schrøder H. A paediatric case of Candida pericarditis and eosophagus stricture during treatment for acute lymphatic leukaemia. Actal Oncol 2007;46(6):859-61. [ Links ]
12. Sion M, Armenaka M, Georgiadis I, Paraskevopoulos G, Nikolaidis I. Aspergillus fumigatus abscesses of the thyroid with obstruction of the esophagus. Thyroid 2004;14(9):786-8. [ Links ]
13. Lingelbach A, Seidl H, Frimberger E, Traidl-Hoffmann C, Ring J, Hoffmann H. Chronic mucocutaneous candidiasis with severe esophageal stricture. Mycoses 2003;46(Suppl 1):15-8. [ Links ]
14. Kim B, Cho S, Rha S, Choi H, Choi K, Cha S, et al. Esophagomediastinal fistula and esophageal stricture as a complication of esophageal candidiasis: a case report. Gastrointest Endosc 2000;52(6):772-5. [ Links ]
15. Diotallevi P, Lacopini G, Montella F, Lauria F, Simili C. Candida esophageal stenosis in an HIV+ patient. Diagnostic imaging and palliative treatment with balloon catheter. Radiol Med 1996;92(1-2):159-61. [ Links ]
16. Kimura H, Kurachi M, Tsukioka Y, Minani M, Itou M, Fujii H, et al. Esophageal stricture secondary to candidiasis without underlying disease. J Gastroenterol 1995;30(4):508-11. [ Links ]
17. Simon G, Rákóczy G, Galgóczy J, Verebély T, Bókay J. Acremonium kiliense in oesophagus stenosis. Mycoses 1991;34(5-6):257-60. [ Links ]
18. Dua K. Expandable stents for benign esophageal disease. Gastrointest Endosc Clin N Am 2011;21(3):359-76. [ Links ]
19. Hirdes M, Vleggaar F, Siersema P. Stent placement for esophageal strictures: an update. Expert Rev Med Devices 2011;8(6):733-55. [ Links ]
20. Hull P. Systemic histoplasmosis with oesophageal obstruction due to Histoplasma granulomas. Successful treatment with rifampicin and amphotericin B. S Afr Med J 1979;14;55(16):639-40. [ Links ]
21. Marshall J, Singh R, Demmy T, Bickel J, Everett E. Mediastinal histoplasmosis presenting with esophageal involvement and dysphagia: case study. Dysphagia 1995;10(1):53-8. [ Links ]
22. Wilson J, Louie B, Farivar A, Vallières E, Aye R. Fully covered self-expanding metal stents are effective for benign esophagogastric disruptions and strictures. J Gastrointest Surg 2013;17(12):2045-50. [ Links ]
23. Van Halsema E, Wong K, Baron T, Siersema P, Vleggaar F, Ginsberg G, et al. Safety of endoscopic removal of self-expandable stents after treatment of benign esophageal diseases. Gastrointest Endosc 2013;77(1):18-28. [ Links ]











 text in
text in