Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.1 Bogotá Jan./Mar. 2015
Case Report of Rectal Ameboma with Associated Liver Abscess
Faruk Esteban Erebrie G. MD. (1), William Hernán Valencia G. MD. (2), Luis Gonzalo Guevara C. MD. (3), René Marcelo Escobar P. MD. (4)
(1) Specialist in Clinical Gastroenterology at the Hospital Universitario San Vicente Fundación in Medellin, Colombia. Email: farukerebrie@hotmail.com
(2) Specialist in Clinical Gastroenterology at the Hospital Universitario San Vicente Fundación in Medellin, Colombia. Email: wihvalen@yahoo.com
(3) Specialist Hepatology and Clinical Gastroenterology at the Hospital Universitario San Vicente Fundación in Medellin, Colombia. Email: gonzogastro@gmail.com
(4) Specialist in Gastrointestinal Surgery and Digestive Endoscopy at the Hospital Universitario San Vicente Fundación in Medellin, Colombia. Email: remar_med@hotmail.com
Received: 28-05-14 Accepted: 02-02-15
Abstract
Entamoeba histolytica infections continue to be a major public health problem in developing countries such as Colombia. Although it most often presents as dysentery or amebic liver abscess, there are cases in which a true inflammatory mass develops in the colon. This is called an ameboma. These amebomas are easily confused with neoplastic lesions so that in the absence of a high level of clinical and endoscopic suspicion, a colon resection may be performed with the postoperative diagnosis given by the presence of trophozoites without malignancy. However, when the diagnosis is made preoperatively symptoms can be without surgery. We report a rare presentation of ameboma in the rectum associated with a perforated liver abscess. This was diagnosed prior to surgey, but given the liver injury, required surgery.
Keywords
Entamoeba histolytica, ameboma, amebic liver abscess.
INTRODUCTION
Amebiasis caused by entamoeba histolytica is a health problem with b impacts in developing countries. Its clinical picture ranges from an absence of symptoms through colitis with bloody diarrhea to liver abscesses and chronic localized infections of the colon wall in which a true mass called an ameboma or amebic granuloma forms. This latter form of presentation is quite uncommon, but when it does occur it is most frequent in the cecum and right colon. The joint presentation of ameboma and liver abscesses has been seen in some cases and may be confused with metastatic colon.
CLINICAL CASE DESCRIPTION
The patient was a 55 year old male worker from Medellín, Antioquia. He had smoked eight cigarettes/day for 15 years and had had chronic constipation for eight years with frequent episodes of rectal bleeding without abdominal pain. During that time he has lost eight kilograms of weight. In November 2011 a sigmoidoscopy showed moderate proctitis and biopsies showed lymphocytic colitis. Treatment with 1g/day of sulfasalazine, twice a day mesalazine enemas, and folic acid was begun. Another colonoscopy in October 2012 reported active pancolitis, but - contradictorily - biopsies showed a "hyperplastic polyp". Nevertheless, the patient was treated with 4 grams/day of mesalazine, 40mg/day of prednisone and folic acid with a strategy to assess his clinical and endoscopic response after three months.
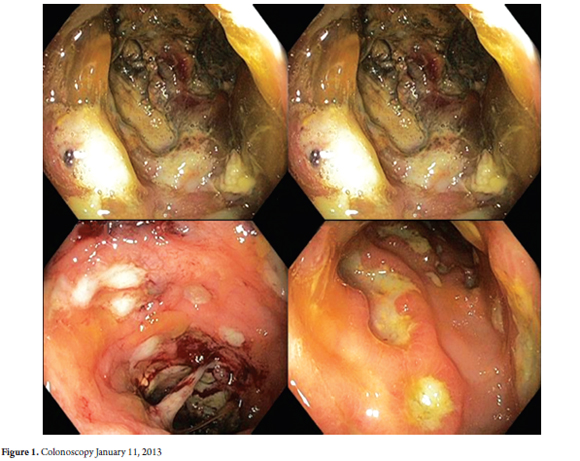
The patient was admitted into the Hospital Universitario San Vicente de Paul on August 1, 2013 because of an increased number of bowel movements, bleeding, and greater weight loss. Upon examination he was found to be malnourished with a mucocutaneous pallor, but hydrated with normal vital signs and no abdominal pain. Initial tests showed leukocytosis of 13,600, polymorphonuclear leukocytes 80%, Hb 12.6g/dl, a platelet count of 360,000, albumin 2.5mg/dl and normal blood chemistry, liver functioning and clotting times. No parasites were found in the patient's stool. A colonoscopy on November 1, 2013 (Figure 1) showed multiple ulcers of different sizes alternating with areas of normal mucosa and a circumferential tumor in the rectal mucosa. The tumor was necrotic, stenosing, friable and bled easily. For this reason biopsies could not be taken to exclude malignancy or Crohn's disease. The pathology report said, "fragments of colonic mucosa with dense mononuclear inflammatory infiltrate in the lamina propria, extensive necrosis, malignant neoplastic proliferation consisting of small to medium-sized cells with scarce cytoplasm and hyperchromatic round nuclei and nucleoli visible without mitotic figures."
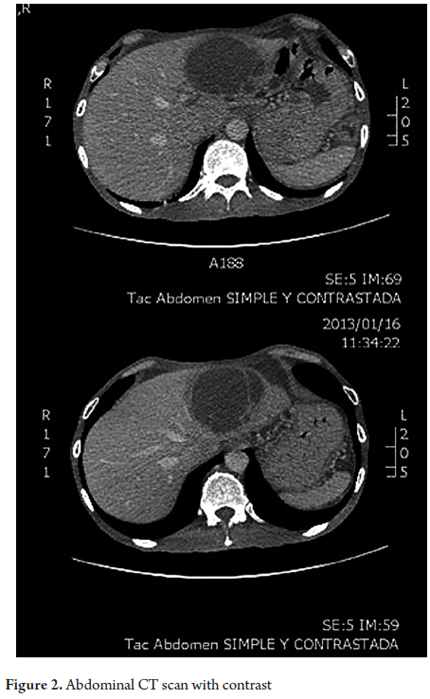
Tests for immunohistochemical markers CD3, CD20, CD10, BCL6, BCL2 and cyclin D1 were negative. It was concluded that there was a malignant neoplasm which needed to be classified. Since the sample consisted of necrotic tissue, it was not possible to reach a conclusive diagnosis. For this reason new viable tissue biopsies were requested. An abdominal CT scan with contrast (Figure 2) showed pancolitis and two hepatic lesions compatible with abscesses. Tests for HIV, ANA, ANCA, viral infections and tuberculosis were all negative. Treatment with IV ciprofloxacin and metronidazole began.
Biopsy samples taken during another colonoscopy on January 18, 2013 showed dense inflammatory mononuclear infiltrate in the lamina, extensive necrosis, and an active ulcer with a severe invasion of amoeba trophozoites but of malignancy. Intravenous antibiotic therapy was continued. On January 25, 2013, the patient reported sudden severe abdominal pain, and there were signs of peritoneal irritation.
A laparotomy found purulent peritonitis in four quadrants, an abscess in the left hepatic lobe that had broken open, a rectal mass with necrosis, and perforation and loss of the rectal wall. The abscess cavity measured approximately 15cm x 10 cm, the rectal mass with necrosis measured 4cm x 4cm, and loss of the rectal wall created a pelvic abscess with fecal matter inside. The right and transverse colon were found to have normal macroscopic appearance, but ulcers were observed in the mucosa of the descending colon. The pelvic abscess and the peritonitis were drained, the descending colon, sigmoid colon and proximal rectum, including the inflammatory lesion, were resected. The rectal stump was closed and a Hartmann type colostomy was placed followed by peritoneal lavage and closure of abdominal cavity. The patient remained in the ICU for 48 hours. His evolution was favorable and he was discharged eight days after surgery.
The macroscopic pathology report showed necrotic areas of the colon, fibrinopurulent membranes, and a 10cm long perforation associated with the presence of a hardened 4.5cm diameter mass. The microscopic report showed extensive ulceration covered by fibrin, abundant macrophages, button shaped ulcers, microabscesses, elongated crypts, severe nuclear reactive changes, amoeba trophozoites and perforation with liquefaction necrosis.
Subsequently the colostomy was closed after colonoscopy showed that the colon and rectal stump had completely normal mucosa.
DISCUSSION
Amebiasis continues to be an endemic health problem in Colombia despite improvements in hygiene in both urban and rural areas of our country (1). Acute attacks of amebic colitis with bloody diarrhea currently receive better and faster treatment which lowers the number of associated complications (2).
The ameboma (amebic granuloma) is a lesion that often appears to be a colorectal tumor (3-5). They result from hypertrophic changes and formation of granulation tissue of the colon wall surrounding a large infected ulceration which adds to secondary bacterial infection and accumulation of collagen (6, 7). Usual symptoms include recurrent diarrhea, lower gastrointestinal bleeding, lower abdominal pain, weight loss, low grade fever, an abdominal mass, and even intestinal obstruction (2, 6). The ameboma becomes symptomatic long after, even years after, an untreated or inadequately treated attack of acute dysentery (8).
They are usually solitary but may be multiple. They occur most frequently in men between the ages of twenty and sixty in the cecum, appendix and sigmoid colon. Less frequently they occur in the hepatic flexure, transverse colon and splenic angle (9). It has been estimated that amebomas form in only 1.5% of all cases of amebiasis (2, 7).
A stool sample isolated or a series of stool samples can help diagnose the presence of trophozoites or cysts, although they may not be found in patients without a recent history of dysentery. Endoscopic diagnosis is bly dependent on a high index of suspicion by the endoscopist. Biopsies taken at colonoscopy allow establishment of the diagnosis in about 60% of cases provided that the trophozoites are found for which special stains (PAS) may be necessary since tissue destruction can hide their presence (6, 7). The biopsy can also distinguish between carcinoma and adenoma, although, as in the case presented, it may also show a false negative and a report of a nonexistent carcinoma.
The differential diagnosis must consider colorectal carcinoma, adenomas, intestinal tuberculosis, ulcerative colitis, Crohn's disease, appendiceal abscesses following appendicitis, and abscesses due to acute diverticulitis (3).
Often the diagnosis cannot be established preoperatively and a surgical specimen reveals the presence of trophozoites. In the largest time series of amebomas cases, published in 1955 with data from 78 cases of the Institute of Pathology of the Armed Forces of the United States, mortality occurred in almost 40% of the cases (10). Currently, mortality rates are much lower, but the rate has not been adequately established because of the marked decrease in the total number of cases.
When the diagnosis is established endoscopically without surgery, treatment with intravenous metronidazole is the first choice for acute attacks ranging from amoebic colitis to liver abscesses and amebomas. Amebomas can even improve and disappear completely after treatment, which should also include an antibiotic given the need to eradicate secondary bacterial infection (1, 2).
Today surgery should be reserved for cases with complications such as intestinal obstruction or perforation and for cases for which a diagnosis has not been established endoscopically and histopathologically (11).
The usefulness of blood tests for amebiasis in our environment is controversial because a large percentage of the population will test positive. The measurement of antigens in stool is another good alternative when this diagnosis is suspected on the basis of endoscopic and imaging studies (1, 2).
When an ameboma is present together with a hepatic abscess, the treatment of choice remains intravenous metronidazole combined with percutaneous drainage of the liver abscess when indicated (12-14). At present, liver surgery is rarely necessary except when the abscess has ruptured, when it is located in the left hepatic lobe, when it is very large, and when is located near the diaphragm and the pericardium. The frequency of simultaneous rupture of a liver abscess and perforation of the colon is unknown.
The patient in the clinical case presented here had an ameboma in a site which is probably a less frequent site for amebomas than those reported in the literature such as the rectum. This patient also had two liver abscesses and was initially misdiagnosed. The logical result was progressive worsening despite treatment which led to simultaneous ruptures of the ameboma and liver abscess. This case enriches our clinical experience and calls for even more emphasis on high levels of suspicion in similar cases in an endemic country like Colombia.
Despite not having achieved a review of the plates and paraffin blocks from the biopsies taken in the first two colonoscopies which were performed outside of our institution, it can be said that extensive necrosis, a b inflammatory response, reactive nuclear changes and an apparent absence of trophozoites led to confusion in the histological diagnosis. This confusion continued in the first colonoscopy performed in our hospital which is similar to difficulties in diagnosis reported in the literature. Both microscopically and macroscopically, the surgical specimen showed classic signs of ameboma and transmural compromise by trophozoites.
REFERENCES
1. Gómez J, Cortés J, Cuervo S, López M. Amebiasis intestinal. Infect 2007;11(1):36-45. [ Links ]
2. Haque R, Huston C, Hughes M. Amebiasis. N Engl J Med 2003;348:1565-73. [ Links ]
3. Majeed S, Ghazanfar A, Ashraf J. Caecal amoeboma simulating malignant neoplasia, ileocaecal tuberculosis and Crohn's disease. J Coll Physicians Surg Pak 2003;13:116-7. [ Links ]
4. Ng D, Kwok S, Cheng Y, Chung C, et al. Colonic amoebic abscess mimicking carcinoma of the colon. Hong Kong Med J 2006;12:71-3. [ Links ]
5. Simsek H, Elsurer R, Sokmensuer C. Amoeboma mimicking carcinoma of the cecum: case report. Gastrointest Endosc 2004;59:453-4. [ Links ]
6. Mendell G, Benett J, Douglas R. Principles and practice of infectious diseases. 6th edition. New York: Churchill Livingstone; 2005. [ Links ]
7. Liu C, Crawford J. The gastrointestinal tract. In: Kumar V, Abbas AK, Fausto N, editors. Robbins and Cotran pathologic basis of disease. 7th edition. Pennsylvania: WB Saunders Company; 2004. p. 839-40. [ Links ]
8. Misra S, Misra V, Dwivedi M. Ileocecal masses in patients with amebic liver abscess: etiology and management. World J Gastroenterol 2006;12:1933-6. [ Links ]
9. Rodea H, Athié C, Durán M, Montalvo E, et al. El comportamiento del ameboma en las últimas cuatro décadas. Experiencia en el Hospital General de México. Cir Gen 2008;30(2). [ Links ]
10. Radke R. Ameboma of the intestine: an analysis of the disease as presented in 78 collected and 41 previously unreported cases. Ann Intern Med 1955;43(5):1048-66. [ Links ]
11. Radovanovic Z, Katic V, Nagorni A, Zivkovic V, et al. Clinical diagnostic problems associated with caecal amoeboma: Case report and review of the literature. Pathol Res Pract 2007;203:823-5. [ Links ]
12. Ray G, Iqbal N. Right colonic mass with hepatic lesion - remember ameboma. Indian J Gastroenterol 2006;25:272. [ Links ]
13. Sharma D, Patel L, Vaidya V. Amoeboma of ascending colon with multiple liver abscesses. J Assoc Physicians India 2001;49:579-80. [ Links ]
14. Sachdev G, Dhol P. Colonic involvement in patients with amoebic liver abscess: Endoscopic findings. Gastrointest Endosc 1997;46:37-9. [ Links ]











 text in
text in