Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.2 Bogotá abr./jun. 2015
Evaluation of the Safety of ERCP in Older Patients in the Experience of a University Hospital in Bogota
Viviana Parra MD. (1), Margarita Huertas Q. MD. (2), Johnny Beltrán MD. (3), Douglas Ortiz MD. (2)
(19 General Surgery Resident at the Universidad Militar Nueva Granada in Bogotá, Colombia. Mail: vivi_850@hotmail.com
(2) Specialist in General and Gastroenterological Surgery in the Department of General and Gastroenterological Surgery at the Hospital Universitario Clínica San Rafael in Bogotá, Colombia.
(3) Specialist in Internal Medicine and Epidemiology
(4) Specialist in General and Gastroenterological Surgery, Head of the Department of Gastroenterology at the Hospital Universitario Clínica San Rafael in Bogotá, Colombia.
Received: 05-11-14 Accepted: 06-04-15
Abstract
Background: Although endoscopic retrograde cholangiopancreatography (ERCP) is the method of choice for management of choledocholithiasis, there are still controversies about its safety for elderly patients.
Objective: To determine whether there is increased risk of complications from ERCP in the management of choledocholithiasis in patients over 70 years valued at University Hospital Clínica San Rafael (HUCSR).
Methodology: A cross-sectional analytical study that included patients admitted to the emergency department of HUCSR during the period of one year (2011-2012) with a diagnosis of choledocholithiasis was performed. The demographic, clinical and paraclinical findings and procedure were analyzed taking into account two groups of patients (older and younger than 70 years). Univariate statistical analysis was performed and bivariate.
Results: A total of 171 patients were included. The presence of comorbidities (eg, diabetes and hypertension), the levels of direct bilirubin and transaminases were variables significantly associated with patients with greater than or equal to 70 years old. Procedure-related complications were presented the most frequent post-ERCP pancreatitis and post papilotomy bleeding; however, were not related to patient age.
Conclusion: ERCP is safe in patients with choledocholithiasis. Age over 70 years does not increase the mortality associated with the procedure.
Keywords
Endoscopic retrograde cholangiopancreatography (ERCP), choledocholithiasis, elderly, complications.
INTRODUCTION
Elderly patients frequently consult physicians about biliary disease because changes in biliary anatomy and physiology create greater predisposition for some diseases such as choledocholithiasis (1). These changes include increased lithogenicity, decreased synthesis of bile salts, impaired gallbladder motility, peripapillary diverticula, decreased response to cholecystokinin and increased diameters of the common bile duct.
Endoscopic retrograde cholangiopancreatography (ERCP) has been established as the method of choice for treatment of choledocholithiasis. Its success rate is 85% to 90% (2). Nevertheless, like any invasive procedure it may have complications which have been reported to be in the range of 5% to 10%. Consequently, ERCP is reserved for patients who have confirmed choledocholithiasis or a high probability of choledocholithiasis (3). Among the most frequent complications are pancreatitis following ERCP (5%) (3), bleeding following sphincterotomies (2%) (4), and perforations (1%) (3). Other complications include cholangitis, cholecystitis, cardiopulmonary events, and side effects of sedation. Mortality rates are low (0.5%) (3).
Studies that attempt to assess the efficacy, safety and complication rate of ERCP in patients older than 70 years are scarce, have inappropriate sample sizes and have not been conducted in ethnically mixed populations like that of Colombia. Consequently, no consensus exists in Colombia about comorbidities and complications. The aim of this study is to establish factors and frequencies of those factors related to the safety of performing ERCPs in patients older than 70 years of age. On this basis we hope to provide a better safety profile and generate proposals for action to reduce complication rates.
MATERIALS AND METHODS
Study Population
This was a cross-sectional analytical study which included 171 consecutive adult patients between September 2011 and August 2012 at Hospital Universitario Clínica San Rafael (HUCSR). All patients were admitted to the emergency department and had at least one of the following conditions (5): biliary obstruction and/or acute cholangitis, biliary pancreatitis, high level of suspicion of choledocholithiasis or diagnosis with ultrasound, CT scan, and/or Magnetic resonance cholangiopancreatography (MRCP) or clinical diagnosis of symptomatic choledocholithiasis (i.e., biliary colic, cholelithiasis, ultrasound indicating biliary duct dilation greater than 7mm, altered hepatic profile, jaundice, acholia and/or dark urine).
The study design was approved by the institutional research committee of the HUCSR.
Each patient was evaluated by two experienced endoscopists. Sociodemographic, clinical and paraclinical data were obtained by interviews, reviews of medical histories, physical examinations and findings from ERCP procedures. All data were collected in an electronic database.
ERCP Procedures
ERCP procedures were performed by two endoscopists with experience with ERCP and certifications in sedation. All patients were given 10% topical oropharyngeal lidocaine spray and sedated with 3.1 mg of midazolam or 30-50 mg of meperidine according to the criteria of the endoscopist. Patients were given a single 20 mg dose of the antispasmodic drug, hyoscine butylbromide. Patients were strictly monitored during procedures in accordance with institutional protocols.
An Evis-Exera Olympus (Olympus, Inc. Tokyo, Japan) duodenoscope was used for procedures. Following cannulation of the bile duct the cholangiography was used to verify the presence of choledocholithiasis. Upon confirmation, stones were extracted using a Dormia basket or balloon dilation.
All patients remained in the hospital for an average period of two days with a minimum 24-hour period of fasting.
The success or failure of procedures was evaluated on the basis of whether or not there were any anatomical alterations such as periampullary diverticula and peripapillary fistulas that hindered procedures, whether or not papillotomies were performed, and whether or not there were any post ERCP complications.
Complications
Any adverse event related to ERCP occurring within 30 days of the procedure was considered to be a complication (3). Mortality was attributed to the procedure when death occurred within 30 days of the ERCP as a complication of the procedure itself (6). Among the post ERCP/sphincterotomy complications that were evaluated in the study were pancreatitis, duodenal perforations, bleeding, cholangitis, acute cholecystitis, and cardiopulmonary complications secondary to sedation. Post ERCP pancreatitis was defined as new pancreatic type abdominal pain or worsening of existing pain associated with at least one three-fold increase in serum lipase or amylase from the reference level within the first 24 hours after ERCP (4, 7). Duodenal perforations can be checked during the procedure or after through clinical radiology or identification of symptoms and compatible with perforations such as persistent abdominal pain and verification of pneumoperitoneum (4).
Post sphincterotomy bleeding can occur early or be delayed. Early occurrence is defined as documented bleeding during the procedure while late bleeding occurs more than 24 hours after the procedure (4, 7). Gastrointestinal bleeding includes melena and hematemesis. Post ERCP cholangitis occurs when cholangitis is absent prior to the procedure according to clinical and/or x-ray evidence but urgent intervention is then required after the ERCP (4, 8, 9). When acute cholecystitis develops following ERCP when it has also been absent prior to the procedure according to clinical and/or x-ray evidence, urgent cholecystectomy or drainage of the gallbladder is required (4). Cardiopulmonary complications secondary to sedation include acute myocardial infarction, stroke, respiratory failure, arrhythmia, pulmonary thromboembolism and aspiration (10).
Statistical Analysis
Univariate analysis was performed first. Categorical variables were analyzed using frequencies. The Kolmogorov-Smirnov test was performed to assess the normality of continuous quantitative variables. Parametric data were expressed as means and standard deviations (SD), and non-parametric data were described as medians and interquartile ranges (IQR).
Bivariate analysis was conducted to identify associations of procedural complications with ages of patients older than 70 years. The presence of complications and/or mortality was assessed using either the chi-square test or Fisher's exact test (used when the variable was dichotomous). Parametric values were analyzed using the Student t test. Nonparametric values were tested with the Mann-Whitney U-Test A value of p <0.05 was considered significant.
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS v.20, Chicago, IL).
RESULTS
Description of patients undergoing ERCP
In total, 312 ERCPs were performed. However, 141 patients were excluded from the analysis: ninety-two were excluded because they were outpatients, twenty-three were excluded because they underwent ERCPs for reasons other than choledocholithiasis, and twenty-six were excluded because of incomplete clinical histories. A total of 171 patients met all the criteria of the study.
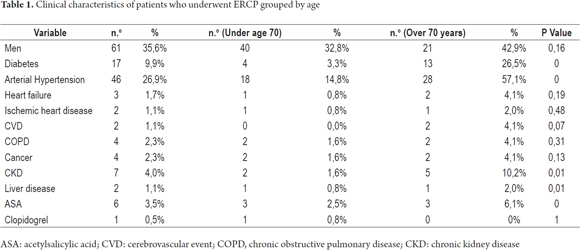
Of the total study population, 64.3% were women (110/171). Patients 70 years of age or older accounted for 28% (48/171) of the patients. The comorbidities most frequently encountered were hypertension (26.9%, 46/171) and diabetes mellitus (9.9%, 17/171). For a detailed description see Table 1.
Age Group Comparison: Bivariate Analysis
Statistically higher frequencies of chronic renal failure and liver disease were found in patients who were older than 70 years compared to younger patients (10.2% vs. 1.6%, p = 0.01 and 2.0% vs. 0.8%, p = 0.01) (Table 1).
Analysis of patients' liver functions upon admission to the emergency room shows that direct bilirubin and aspartate transaminase (AST) levels were significantly higher in the population over 70 years of age than in the younger population (3.8 vs. 2.9, p = 0.05 and 283 vs. 171, p = 0.01). In contrast, alanine transaminase (ALT) levels were higher among younger patients and the differences were also statistically significant (207 vs. 382, p <0.001). No significant differences in the values of total bilirubin, alkaline phosphatase, amylase or diameters of the common bile ducts were found between the two groups.
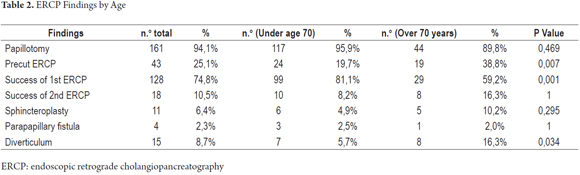
Endoscopic findings show that about one third of patients required papillary pre-cuts. This was required more often for those over 70 years of age than for younger patients (38.8% vs. 19.7%, p = 0.007). In addition, peripapillary diverticula were more common among older patients than among younger patients (16.3% vs. 5.7% p = 0.034). No statistically significant associations were found for differences in performances of papillotomies and sphincteroplasties or for peripapillary fistulas. Of the total number of procedures performed, complete removal was achieved in the first ERCP in 128 patients (74.8%). Of these, 81.1% were under age 70 and 18.9% were 70 years or over (p = 0.001). ERCPs were unsuccessful the first time in 43 (25.1%) cases. Of these, 21 patients underwent a second ERCP which was successful in 18 cases and failed in three cases. There were no significant differences according to ages (Table 2).
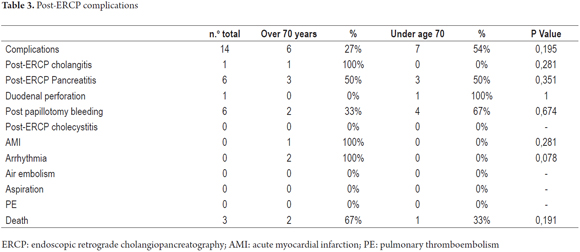
Complications developed in 8.1% of the patients (14/171) who underwent cholangiography conducted, and 1.75% of the total number died (3/171). The most frequent complication was pancreatitis following ERCP and bleeding following papillotomy (3.5% each). According to the APACHE II system for calculating severity of pancreatitis, four patients had mild pancreatitis and two had severe pancreatitis. The latter two (1.6%) both died as a result of pancreatitis (1.6%). All cases of bleeding following papillotomy was identified early and controlled in a timely manner through sclerotherapy during the same procedure without requiring any additional intervention. All patients underwent endoscopic follow-up examinations to control bleeding, and none required transfusions. Frequencies of complications were not significant in either of the two age groups studied (Table 3).
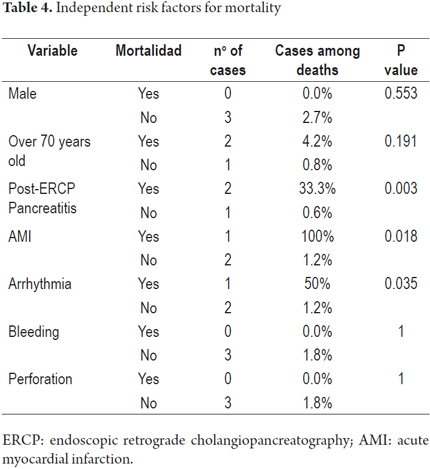
All three patients who died were women. Risk factors for mortality were post-ERCP pancreatitis, arrhythmia and myocardial infarction but were not associated with age (Table 4).
DISCUSSION
Clinical characteristics of patients
Our study identified higher frequencies of comorbidities and greater consumption of ASA among people over 70 years of age. These findings are consistent with what has been published in the literature about older patients undergoing ERCP (11, 12). Recently, published findings similar to those in our population have shown that risk increases 0.8% per year of life, is higher among men than among women (OR 1.2, 95% CI: 1.1-1.2), is higher among patients with diabetes (OR 1.1, 95% CI: 1.0 -1.2), and higher among patients with hypertension (OR 1.1, 95% CI: 1.0 -1.2) (13).
Laboratory Tests Performed upon Admission
Changes in AST, ALT and total bilirubin levels are recognized as paraclinical markers for choledocholithiasis (14), and it has been found that people above the age of 70 have significantly higher levels of all three markers. The levels of total direct and indirect bilirubin are directly related to strengthening of oxidative processes in patients with choledocholithiasis which suggests that patients older than 70 years are exposed to longer processes that damage tissue and may have greater amounts of liver damage (15).
Endoscopic findings, findings on ERCP procedure
This study identified a large number of patients over the age of 70 who had peripapillary diverticula. These may be related to increased likelihood of recurrent biliary obstructions (16). A previous study which compared patients who were over 75 years old with those who were younger than 75 found no statistically significant differences regarding the frequency of occurrence of peripapillary diverticula. The differences between the two studies may be explained by characteristics of the study populations such as ages, disease severity and comorbidities or by the manner in which patients were classified (17).
This study has demonstrated a high first time success rate of 75% of patients plus an additional 10% in the second procedure. It was further found success is achieved in the first procedure in a significantly higher proportion of patients under 70 than the proportion in those over 70. Some studies have explored factors related to failure of first ERCP procedures. Sphincteroplasties, peripapillary diverticula, and the size and number of calculi are factors that reduce the first ERCP success rate according to recent publications (18). The higher success rate reported in patients younger than 70 years of age may be related to any of these factors reported in other studies.
Our ERCP combined first and second attempt success rate of 85% is similar to those reported in the literature which vary from 80% to 100% although these studies report less frequent need for a second procedure (19-21). The difference may be related to the characteristics of the populations studied and of the studies.
Post-ERCP complications
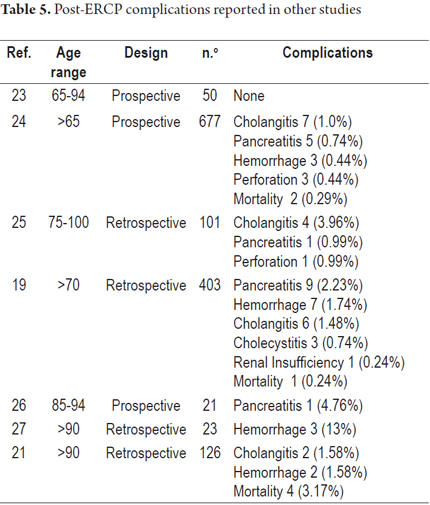
The frequency of complications in this study was low (8%). None of the complications that occurred had statistically significant relations with age. The two most common complications in the study are also common in other studies (Table 5) (19, 21, 22-27).
This study suggests that patient age over 70 is not a factor that increases mortality in patients undergoing ERCP for choledocholithiasis. However, as previously reported, cardiovascular complications and pancreatitis are factors that increase mortality related to ERCP.
CONCLUSION
ERCP is a safe procedure which shows no increase in mortality or complications for patients over the age of 70. Additional prospective studies with more robust statistical analysis are needed to explore the safety of the procedure with greater certainty.
Acknowledgements
We wish to thank General Surgery and Gastroenterology Clinic of the Hospital Universitario Clínica San Rafael for supporting this project.
REFERENCES
1. Ross SO, Forsmark CE. Pancreatic and biliary disorders in the elderly. Gastroenterol Clin North Am. 2001;30:531-45. [ Links ]
2. Attasaranya S, Fogel EL, Lehman GA. Choledocholithiasis, ascending cholangitis, and gallstone pancreatitis. Med Clin North Am. 2008;92:925-60. [ Links ]
3. Freeman ML. Complications of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin N Am. 2012;22:567-86. [ Links ]
4. Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-18. [ Links ]
5. Ángel A, Rosero GVJ. Guía de manejo de coledocolitiasis. Bogotá: Hospital Universitario Clínica San Rafael; 2009. p. 6-7. [ Links ]
6. Peñaloza-Ramírez A, Leal-Buitrago C, Rodríguez-Hernández A. Adverse events of ERCP at San José Hospital of Bogotá (Colombia). Rev Esp Enferm Dig. 2009;101:837-49. [ Links ]
7. Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-93. [ Links ]
8. Mayumi T, Someya K, Ootubo H, Takama T, Kido T, Kamezaki F, et al. Progression of Tokyo Guidelines and Japanese Guidelines for management of acute cholangitis and cholecystitis. J UOEH. 2013;35:249-57. [ Links ]
9. Frossard JL, Morel PM. Detection and management of bile duct stones. Gastrointest Endosc. 2010;72:808-16. [ Links ]
10. Balmadrid B, Kozarek R. Prevention and management of adverse events of endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am. 2013;23:385-403. [ Links ]
11. Li C, Ford ES, Zhao G, Wen X-J, Gotway CA. Age adjustment of diabetes prevalence: Use of 2010 U.S. Census data. J Diabetes. 2014;6:451-61. [ Links ]
12. Bao YS, Jia XB, Ji Y, Yang J, Zhao S-L, Na S-P. High prevalence and risk factors for kidney dysfunction in patients with atherosclerotic cardio-cerebrovascular disease. QJM. 2014;107:443-9. [ Links ]
13. Wolfgang CL. Predicting complicated choledocholithiasis. J Surg Res. 2013;185:502-3. [ Links ]
14. Yriberry Ureña S, Monge Zapa V. Alterations in laboratory tests as predictors of choledocholithiasis in patients who underwent ERCP: experience in a national private center. Rev Gastroenterol Peru. 2007;27:253-8. [ Links ]
15. Damnjanović Z, Jovanović M, Nagorni A, Radojković M, Sokolović D, Damnjanović G, et al. Correlation of inflammation parameters and biochemical markers of cholestasis with the intensity of lipid peroxidation in patients with choledocholithiasis. Vojnosanit Pregl. 2013;70:170-6. [ Links ]
16. Pereira-Lima JC, Jakobs R, Winter UH, Benz C, Martin WR, Adamek HE, et al. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457-64. [ Links ]
17. Zippi M, De Felici I, Pica R, Occhigrossi G, Traversa G. Comparison of endoscopic retrograde cholangiopancreatography between elderly and younger patients for common bile duct stones. Clin Ter. 2013;164:e353-8. [ Links ]
18. Tantau M, Mercea V, Crisan D, Tantau A, Mester G, Vesa S, et al. ERCP on a cohort of 2,986 patients with cholelitiasis: a 10-year experience of a single center. J Gastrointestin Liver Dis. 2013;22:141-7. [ Links ]
19. Sugiyama M, Atomi Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc. 2000;52:187-91. [ Links ]
20. Obana T, Fujita N, Noda Y, Kobayashi G, Ito K, Horaguchi J, et al. Efficacy and safety of therapeutic ERCP for the elderly with choledocholithiasis: comparison with younger patients. Intern Med. 2010;49:1935-41. [ Links ]
21. Rodríguez-González FJ, Naranjo-Rodríguez A, Mata-Tapia I, Chicano-Gallardo M, Puente-Gutierrez JJ, López-Vallejos P, et al. ERCP in patients 90 years of age and older. Gastrointest Endosc. 2003;58:220-5. [ Links ]
22. Talar-Wojnarowska R, Szulc G, Woźniak B, Pazurek M, Małecka-Panas E. Assessment of frequency and safety of endoscopic retrograde cholangiopancreatography in patients over 80 years of age. Pol Arch Med Wewn. 2009;119:136-40. [ Links ]
23. MacMahon M, Walsh TN, Brennan P, Osborne H, Courtney MG. Endoscopic retrograde cholangiopancreatography in the elderly: a single unit audit. Gerontology. 1993;39:28-32. [ Links ]
24. Deans GT, Sedman P, Martin DF, Royston CM, Leow CK, Thomas WE, et al. Are complications of endoscopic sphincterotomy age related? Gut 1997;41:545-8. [ Links ]
25. Ashton CE, McNabb WR, Wilkinson ML, Lewis RR. Endoscopic retrograde cholangiopancreatography in elderly patients. Age Ageing. 1998;27:683-8. [ Links ]
26. Clarke GA, Jacobson BC, Hammett RJ, Carr-Locke DL. The indications, utilization and safety of gastrointestinal endoscopy in an extremely elderly patient cohort. Endoscopy. 2001;33:580-4. [ Links ]
27. Mitchell RMS, OConnor F, Dickey W. Endoscopic retrograde cholangiopancreatography is safe and effective in patients 90 years of age and older. J Clin Gastroenterol. 2003;36:72-4. [ Links ]











 texto en
texto en