Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.2 Bogotá abr./jun. 2015
Two Case Reports and a Literature Review of Liver Transplantation for Epithelioid Hemangioendothelioma
Juan Ignacio Marín MD (1), Óscar Santos MD (1), Octavio Muñoz MD (1), Germán Osorio MD (2), Carlos Guzmán MD (1), Sergio Hoyos MD (1), Álvaro Mena MD (1), Juan Carlos Restrepo MD (1)
(1) Hepatology and Liver Transplantation Unit at the Hospital Pablo Tobón Uribe and the Universidad de Antioquia in Medellín, Colombia.
(2) Department of Pathology at the University of Antioquia in Medellin, Colombia.
Received: 28-05-14 Accepted: 06-04-15
Abstract
Hepatic epithelioid hemangioendothelioma is a rare, aggressive and unpredictable tumor. Its incidence is less than one case per million people per year. Most commonly, it occurs in young women who exhibit nonspecific symptoms such as abdominal pain and weight loss. Radiologically it presents as multiple bilateral and peripheral nodules or masses with retraction of the capsule of the liver. In some cases there is calcification and vascular compromise. A liver biopsy should be performed to confirm the diagnosis and to rule out alternative diagnoses such as angiosarcoma, hepatocellular carcinoma, cholangiocarcinoma and metastasis. Management depends on the extension at presentation, but only 10% of cases are amenable to resection. Although in recent decades liver transplantation has become a management option, only studies of isolated cases reported by various transplant centers around the world have been published so far. In this article, we report our experience with two patients who were diagnosed with hepatic epithelioid hemangioendothelioma in which there were no possibilities of resection. Diagnoses were histologically confirmed, and since the patients had no extra-hepatic compromises, liver transplantations were performed. Both were successful and without recurrence at 4 and 6 years after transplantation.
Keywords
Liver transplantation, hepatic epithelioid hemangioendothelioma, liver tumor.
INTRODUCTION
Hepatic epithelioid hemangioendothelioma (HEH) is a rare tumor of vascular origin that involves soft tissue and different specific organs (1, 2), with an incidence of less than 1 case per million people per year. Pathogenesis is unknown but there is data regarding association with the use of oral contraceptives (3), exposure to vinyl chloride (4), and previous infection with the hepatitis B virus (HBV) and hepatitis C virus (HCV) (5).
HEH was first reported by Ishak in 1984 in a series of 32 patients (2-6). Since then it has been described in organs such as the spleen, bones, meninges, breast, heart, stomach and lymph nodes (6). It commonly affects women and is characterized by epithelioid or histiocytoid morphology and by a growth pattern with evidence of endothelial histogenesis (5). HEH has an unpredictable clinical course and malignant potential. Its behavior is in between hemangioma and angiosarcoma. Differential diagnosis from the latter is very difficult to establish because it requires specific findings in immunohistochemistry to confirm the diagnosis (7). There is no consensus regarding the treatment of these patients because of HEH's clinical nature and variable course (8, 9). The primary treatment of these lesions is surgical resection, but usually diagnosis of the advanced disease happens late, and other options such as chemotherapy, radiation therapy, and in some cases liver transplant are considered. However, up to 25% of patients receive no treatment (2-9). Our goal is to report our experience with liver transplants in two patients with HEH and to review the literature.
CASE REPORTS
Case 1
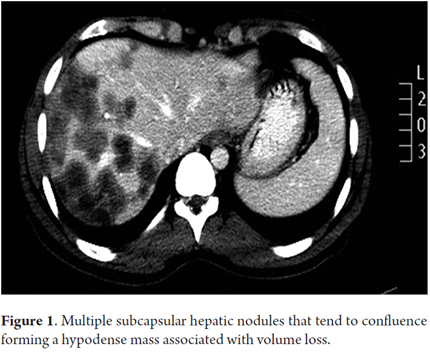
The patient was a 36-year-old woman with no personal medical history of importance, who was not taking drugs and who had no toxic exposure. She was referred to the liver transplant program in 2006 because of a clinical picture of six months of abdominal pain with an increasing perimeter and weight loss. Laboratory tests showed AST: 54 U/L, ALT: 36 U/L, total bilirubin: 1.2 mg/dL, alkaline phosphatase: 382 U/L, gamma glutamyl transpeptidase: 155 U/L, albumin: 3.0 gr/dL, Alpha-fetoprotein: 5.2 ng/mL, with negative serology for hepatitis B and hepatitis C. On examination, the patient showed malnutrition, moderate ascites and hepatomegaly. The contrasted abdominal CT scan showed multiple nodular lesions in both peripheral hepatic lobes tending to coalesce, without findings of cirrhosis or portal hypertension, and without thrombosis of vascular structures (Figure 1). Clinical suspicion for a middle-aged patient without liver cirrhosis called for ruling out liver metastases, angiosarcoma and HEH. To diagnose hepatic epithelioid hemangioendothelioma, a liver biopsy with studies of anatomic pathology and immunohistochemistry were performed (Figure 2). The chest tomography and bone scintigraphy showed no extra-hepatic disease. Since surgical resection was not an option given the advanced condition of the hepatic HEH, liver transplant was defined as the management option. There were no complications in surgery and no vascular, nodal or peritoneal compromise was found in the explant study. In the post-transplant period there were two episodes of late acute moderate cellular rejection which were treated with steroid boluses. Today, eight years after transplantation, the patient is in good clinical condition, with good function of the liver graft, without recurrence of the underlying disease, and under immunosuppressive treatment with low doses of Cyclosporine and Mycophenolate Mofetil.
Case 2
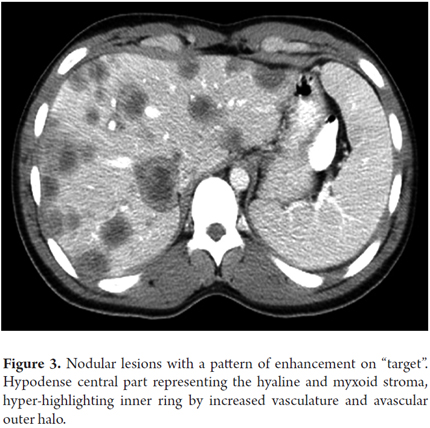
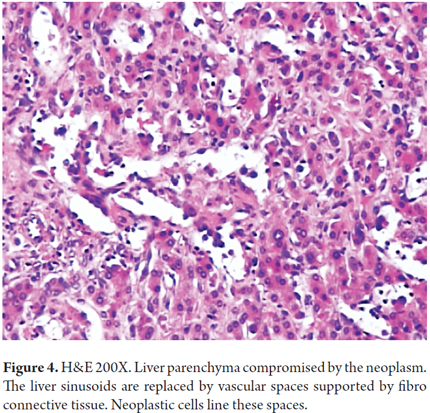
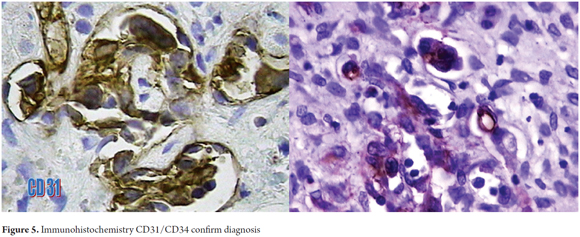
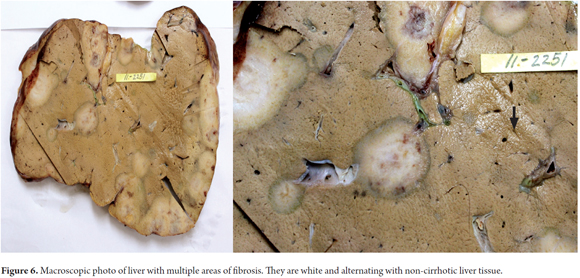
A 21-year-old male patient, with no previous medical history, who consulted in 2010 about a mass and feeling of weight in the right upper quadrant associated with weight loss. In the physical examination the only relevant finding was hepatomegaly. Hepatic biochemical tests reported AST: 46 U/L, ALT: 36 U/L, total bilirubin: 0.8 mg/dL, alkaline phosphatase 179 U/L, gamma glutamyl transpeptidase: 111 U/L, albumin: 4.5 gr/dL, Alfa-fetoprotein: 2.43 ng/mL, negative serology for hepatitis B and hepatitis C. Abdominal ultrasound reported liver enlargement with the presence of nodular lesions throughout the parenchyma. Contrasted abdominal CT was performed and peripheral bilateral lesions with a pattern of enhancement on target and retraction of the liver capsule were found (Figure 3). The main diagnostic possibility was liver metastases. A percutaneous liver biopsy was performed and a histology compatible with epithelioid hemangioendothelioma (Figure 4), which was confirmed by immunohistochemistry that was positive for CD31 and CD34 (Figure 5). A search for extra-hepatic disease was carried out with chest tomography and bone scintigraphy and no metastases were found. Since this was a tumor without the possibility of surgical resection, orthotopic liver transplant was performed on the patient without complications in surgery or during the early postoperative period. The study of the explant (Figure 6) confirmed the diagnosis and ruled out vascular and peritoneal lymph node involvement. One month after transplantation, the patient developed acute moderate cellular rejection, but received recycling with Methyl-prednisolone and immunosuppression adjustment with good clinical and biochemical response. As of this writing the patient has completed four years of transplantation with a functioning graft, without disease recurrence, and with re-entry into the workforce.
DISCUSSION
Hepatic epithelioid hemangioendothelioma is a tumor of vascular origin with potential malignant behavior. It is a rare disease. Only 1 to 2 cases per million inhabitants are usually found. It occurs most often in women and the peak age is between 20 to 40 years (1, 2). Its etiology is unknown but it has been linked to the consumption of oral contraceptives, polyvinyl chloride exposure, exposure to Thorotrast contrast medium, and to chronic infection with hepatitis B and C (3-5). The most common symptoms are abdominal pain and weight loss, but in some cases patients are asymptomatic or may even consult with acute liver failure. Physical examination may be normal or may find jaundice, ascites and hepatosplenomegaly. Regarding diagnosis, there are increased levels of alkaline phosphatase and gamma-glutamyl transferase in 50% of cases. Tumor markers, including alpha-fetoprotein, are negative and diagnosis is based on studies of radiology and pathology. Computed tomography and nuclear magnetic resonance imaging reveal nodular, multiple, bilateral, peripheral lesions, with retraction of the capsule, and with mild peripheral contrast enhancement. Calcifications are found in 20% of lesions. Eventually the lesions join to form a single mass that pervades much of the liver and is usually associated with portal tumor thrombosis. Metastases are common, and can be found in 40% of patients at diagnosis, and the most common locations are the lungs, lymph nodes, peritoneum, bones, spleen, and diaphragm (2). Any patient suspected of having HEH should undergo liver biopsy, and the most likely findings would be fibrotic or myxomatous stroma and the presence of cells of epithelioid characteristics with evidence of vascular differentiation by the presence of erythrocytes in the light. The diagnosis is not easy and should be distinguished from sclerosing hemangioma, angiosarcoma, cholangiocarcinoma, and metastatic carcinoma. For that reason, biopsies must be evaluated by expert pathologists. The endothelial origin with CD31/CD34/FVIII-Rag immunohistochemical staining should be confirmed (2, 7).
With the diagnosis already established, the treatment of choice is resection of the tumor. The problem is that only 10% of patients are candidates for surgical resection at initial assessment. Surgery should be done with oncological purposes because partial resections are associated with accelerated tumor growth. Other treatment strategies have been considered such as radiotherapy, chemotherapy, hormonal therapy, embolization or chemoembolization, percutaneous ablation and liver transplant with different success rates. Systemic chemotherapy has been applied to patients with metastatic disease using drugs like Doxorubicin, 5-fluorouracil, and Vincristine with survival at 5 years of less than 20%. Embolization or chemoembolization is used as a bridge to liver transplantation therapy when waiting times are long, with no good scientific support for this intervention. There is no use of radiotherapy except for palliative purposes, for example in lung and bone metastases. Liver transplant then emerges as the main treatment option, considering that almost 90% of patients show up with the disease in both lobes and there is no possibility of resection. The fear of recurrence is the problem when liver transplant is offered to patients with tumors. However, as described Madariaga et al in an early series (1), the survival of these patients was greater than 60% at 5 years, even in patients with vascular or nodal involvement, these being better results than those reported by the Center for hepatocellular carcinoma itself at that time. The most recent reports confirm a patient survival at 1, 5, and 10 years of 93, 83 and 72% respectively, which is comparable to the survival of liver transplant patients with non-tumoral etiologies (9). These results have changed the global perception regarding liver transplant for patients with HEH (2).
In studies of patients who have undergone liver transplantation, the average age is 30 years, they are predominantly female, and most of them are without comorbidities (9, 10). These characteristics are factors favoring good post-liver transplantation results. Nineteen percent of patients are asymptomatic at the time of transplantation. It is important to note that independently of the clinical presentation, the hepatic tumor involvement is what defines the instruction for transplantation (9). Although 50% of patients show up with advanced disease and vascular invasion, and that this finding constitutes an adverse factor for recurrence, liver transplantation is not contraindicated and must be analyzed on case by case basis. In 17% of the patients had extra-hepatic disease, including nodal involvement, but without affecting the long-term survival.
Regarding surgery, it should be noted that in most cases the standard procedure was conducted, and minor technical difficulties were reported due to the absence of portal hypertension and fewer blood transfusions. Prior surgical procedures did not negatively impact the results of transplantation. Tumor disease recurrence occurs in 20-38% of patients and this is the main cause of death for these individuals. Patients with recurrence should be treated aggressively with systemic chemotherapy, angiogenesis inhibiting drugs, and using mTor type immunosuppressants, although it should be clarified that the above treatments have not been supported by clinical trials yet.
CONCLUSION
In conclusion, hepatic epithelioid hemangioendothelioma should be suspected in all non-cirrhotic young patients who consult with multiple, bilateral, peripheral hepatic nodules and enhancement pattern on target. Although the treatment of choice is liver resection, it can only be performed on a small group of patients. Therefore, liver transplant is the main treatment option, even in patients with advanced disease.
REFERENCES
1. Madariaga J, Marino IR, Starzl TE, et al. Long-term results after liver transplantation for primary hepatic epithelioid hemangioendothelioma. Ann Surg Oncol. 1995;2(6):483-7. [ Links ]
2. Primary malignant hepatic epithelioid hemangioendothelioma, comprehensive review of the literature with emphasis on the surgical therapy. Cancer. 2006;107:2108-21. [ Links ]
3. Dean PJ, Haggitt RC, OHara CJ. Malignant epithelioid hemangioendothelioma of the liver in young women. Relationship to oral contraceptive use. Am J Surg Pathol. 1985;9:695-704. [ Links ]
4. Gelin M, Van de Stadt J, Rickaert F, De Prez C, Levarlet M, Adler M, et al. Epithelioid hemangioendothelioma of the liver following contact with vinyl chloride. Recurrence after orthotopic liver transplantation. J Hepatol. 1989;8:99-106. [ Links ]
5. Lauffer JM, Zimmermann A, Krahenbuhl L, Triller J, Baer HU. Epithelioid hemangioendothelioma of the liver. A rare hepatic tumor. Cancer. 1996;78:2318-27. [ Links ]
6. Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970-81. [ Links ]
7. Fujii T, Zen Y, Sato Y, Sasaki M, Enomae M, Minato H, et al. Podoplanin is a useful diagnostic marker for epithelioid hemangioendothelioma of the liver. Mod Pathol. 2008;21:125-30. [ Links ]
8. Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999;85:562-82. [ Links ]
9. Lerut JP, Orlando G, Adam R, Schiavo M, Klepnauer J, Mirza D, et al. The place of liver transplantation in the treatment of hepatic epitheloid hemangioendothelioma. Report of the European Liver Transplant Registry. Ann Surg. 2007;246:949-57. [ Links ]
10. Rodriguez JA, Becker NS, OMahony C, et al. Long-term outcomes following liver transplantation for hepatic hemangioendothelioma: The UNOS Experience from 1987 to 2005. J Gastrointest Surg. 2008;12:110-6. [ Links ]











 texto en
texto en