Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.2 Bogotá Apr./June 2015
Atypical Herpes Esophagitis
Viviana Parra V. MD (1), Margarita Huertas Q. MD (2), Rigoberto Montoya MD (3), Diego Aponte MD (4), Luis Carlos Sabbagh MD. (5)
(1) General Surgery Resident at the Universidad Militar Nueva Granada in Bogotá, Colombia. Mail:Vivi_850@hotmail.com
(2) Specialist in General Surgeon and Gastroenterologist at the Clínica Universitaria Colombia in Bogotá, Colombia. Mail: margara312@msn.com
(3) Specialist in Internal Medicine-Gastroenterology at the Clínica Universitaria Colombia in Bogotá, Colombia.
(4) Specialist in Internal Medicine and Gastroenterology, Academic Coordinator of the Postgraduate Gastroenterology Program at the Fundación Sanitas in Bogotá, Colombia. Mail: Didimauro673@yahoo.es
(5) Specialist in Internal Medicine and Gastroenterology, Head of the Postgraduate Gastroenterology Program at Fundación Sanitas in Bogotá, Colombia and President of the Colombian Association of Gastroenterology. Mail: lsabbagh@colsanitas.com
Received: 04-08-14 Accepted: 06-04-15
Abstract
Esophageal herpes viral infections are rare condition that have been reported most frequently in immunocompromised patients. This infection primarily affects patients with human immunodeficiency virus (HIV) and patients receiving immunosuppressants or chemotherapy. The severity of symptoms is related to the degree of esophageal involvement. Odynophagia is the most common clinical presentation while the most common endoscopic finding is multiple well-circumscribed ulcers. These typically occur in the distal third of the esophagus. Standard treatment is oral acyclovir for one to two weeks.
Keywords
Herpes esophagitis, herpes simplex virus type I, immunosuppression.
INTRODUCTION
Infectious esophagitis is relatively uncommon, but it can lead to increased morbidity and mortality in immune compromised when it is not accurately diagnosed (1). This condition is most often seen in immunocompromised patients whose resistance has been altered by various conditions (1, 2). Immune deficiencies, malignancies, severe infections and use of immunosuppressive drugs, broad spectrum antibiotics and/or chemotherapy are some of the conditions associated with the risk of developing this condition (2, 3).
Candida albicans, with a reported prevalence of up to 93%, is by far the most common etiology in these patients (4, 5). Herpes Simplex virus type I (HSV 1) is the next most common cause although it accounts for only 0.5% to 6% of the cases. It is followed by cytomegalovirus which accounts for just 0.02% of cases (1, 3, 6). Other pathogens including Aspergillus, Blastomyces, Cryptococcus, Histoplasma, Mycobacterium tuberculosis, Actinomyces, and Varicella Zoster are part of the wide variety of opportunistic microorganisms that have been reported (6-8).
Esophageal herpes virus infections are rare and are most often seen in immunocompromised patients. It has been reported that the occurrence of herpes esophagitis (EH) is mainly due to reactivation of a previous viral infection and occurs less often as a primary infection. When it is a primary infection, HSV 1 is usually responsible (2, 8, 9).
This article presents a case of esophageal herpes in a patient who had been receiving chemotherapy for breast cancer at the Fundación Universitaria Clínica Colombia. At the beginning, she developed severe upper gastrointestinal tract symptoms with insidious onset that at first was attributed to and treated as esophagitis Candida.
CLINICAL CASE
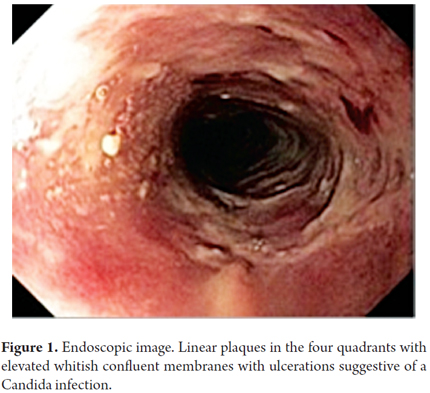
The patient was a 42 year old woman who had been diagnosed with stage IV breast cancer which had metastasized to her bones, liver and brain. She had been receiving palliative chemotherapy and radiation therapy before she came to the emergency department after 20 days of difficulty swallowing both solid foods and liquids, choking and vomiting. An examination showed that the patient was hemodynamically stable, lucid, dehydrated and cachectic. Her oropharyngeal examination was normal. Paraclinical tests showed no biochemical alterations or inflammation. Upper digestive tract endoscopy was interpreted as Candida esophagitis predominantly in the middle third of the esophagus (Kodsi's grade III for esophageal candidiasis) (Figure 1). Biopsies of lesions were taken for histopathological examination. The gastroesophageal junction, stomach (corpus, antrum and pylorus) and duodenum were found to be without pathologies.
On the basis of the endoscopic findings, daily treatment was begun with 200 mg oral fluconazole. Symptoms and tolerance to a liquid diet improved partially within 48 hours, so the patient was discharged and treated with fluconazole continued on an outpatient basis.
The patient was readmitted to the emergency room seven days later because of widespread pain associated with weakness, jaundice and a temporarily altered state of consciousness. Symptoms were not diminished by opioids. During the interview with the patient it was evident that the patient had again been suffering from dysphagia and vomiting for 72 hours despite continuing oral fluconazole but had not come to the hospital.
The patient refused to have another endoscopic examination. She was admitted to the hospital and comprehensive palliative treatment was started, but she subsequently died of liver failure due to metastasis of her cancer.
Following the patient's death, histopathological studies presented conclusive evidence that she had suffered from esophageal herpes (Figure 2).
DISCUSSION
EH was first identified in 1940 by Johnson (3, 10), but the first histopathological descriptions were provided by Pearce and Dagradi in 1943 (3, 11).
The clinical presentation of EH is similar in healthy and immunocompromised patients. The most frequently found symptom is odynophagia which is found in between 60% and 80% of these patients (6, 12, 13). This is followed by chest pain (46% to 50%) and fever (44%) (12, 13). It is rare to find oropharyngeal or skin lesions in physical examinations. Oropharyngeal lesions have been reported in up to 20% of patients, and skin lesions have been reported in up to 13% of patients (12, 13).
Upper endoscopy plays a key role in diagnosis of EH because it allows the physician to see lesions and take biopsy samples at the same time. Regardless of the state of the patient's immune system, the most common endoscopic finding is multiple well-circumscribed ulcers (59% to 86%) (6, 12, 14). They are usually in friable esophageal mucosa (84%) (13, 14) and are often accompanied by whitish exudates (44%) (12). The most common location of EH lesions is in the lower third of the esophagus (63% to 80%) (12). Nevertheless, in up to 15% of the time, they affect the entire esophagus and in 2% of the patients lesions even affect the stomach (6, 10, 15).
Histologically the EH is primarily characterized by the multinucleated giant cells, ballooning degeneration, Cowdry Type A inclusion bodies, intranuclear "ground glass" and marginalization of chromatin (2, 8, 10, 12, 13).
In our case, the diagnosis was made histologically. Although the patient belonged to a high risk group for EH, her condition was secondary to immunosuppression related to treatment for cancer, had a nonspecific clinical presentation, and the endoscopic findings were highly suggestive of a Candida infection which is more frequently found in immunosuppressed patients. A similar case was reported at the Case University Hospital in Cleveland, Ohio in 2005. The patient had colon cancer which had metastasized. The initial endoscopic diagnosis was Candida esophagitis, but pathology subsequently reported characteristic findings for EH (16).
CONCLUSION
EH is rare but should be considered in immunocompromised patients with esophageal symptoms. Moreover, although endoscopic diagnosis can be highly suggestive of another entity, it must always be checked against the histopathological diagnosis.
REFERENCES
1. Infective Esophagitis. En: Takubo K. Pathology of the esophagus. 3rd edition. Japan: Springer Japan; 2009. p. 58-69. [ Links ]
2. Mulhall BP, Wong RKH. Infectious esophagitis. Curr Treat Options Gastroenterol. 2003;6(1):55-70. [ Links ]
3. Itoh T, Takahashi T, Kusaka K, Kawaura K, Nakagawa Y, Yamakawa J, et al. Herpes simplex esophagitis from 1307 autopsy cases. J. Gastroenterol. Hepatol. 2003;18(12):1407-11. [ Links ]
4. Kliemann DA, Pasqualotto AC, Falavigna M, Giaretta T, Severo LC. Candida esophagitis: species distribution and risk factors for infection. Rev Inst Med Trop Sao Paulo. 2008;50(5):261-3. [ Links ]
5. Olmos MA, Araya V, Concetti H, Ramallo J, Piskorz E, Pérez H, et al. Oesophageal candidiasis: clinical and mycological analysis. Acta Gastroenterol Latinoam. 2005;35(4):211-8. [ Links ]
6. Namasivayam V, Murray JA. Infectious esophagitis. En: Shaker R, Belafsky PC, Postma GN, Easterling C. Principles of Deglutition. New York: Springer; 2013. p. 657-66. [ Links ]
7. Wilcox CM. Gastrointestinal consequences of infection with human immunodeficiency virus. En: Freidman LS, Brandt LJ, eds. Sleisenger & Fordtrans gastrointestinal and liver disease. 9th edition. Philadelphia: WB Saunders; 2010. p. 523-36. [ Links ]
8. Katzka DA. Esophageal disorders caused by medications, trauma, and infection. En: Freidman LS, Brandt LJ, eds. Sleisenger Fordtrans Gastrointest and liver disease. Philadelphia: WB Saunders; 2010. p. 735.44. [ Links ]
9. Lee B, Caddy G. Case report. A rare cause of dysphagia : Herpes simplex esophagitis. World J Gastroenterol. 2007;13(19):2756-7. [ Links ]
10. Canalejo Castrillero E, García Durán F, Cabello N, García Martínez J. Herpes esophagitis in healthy adults and adolescents: report of 3 cases and review of the literature. Medicine. 2010;89(4):204-10. [ Links ]
11. Johnson HN. Visceral lesions associated with varicella. Arch Pathol. 1940;30:292-307. [ Links ]
12. Lavery EA, Coyle WJ. Herpes simplex virus and the alimentary tract. Curr Gastroenterol Rep. 2008;10(4):417-23. [ Links ]
13. Ramanathan J, Rammouni M, Baran J, Khatib R. Herpes simplex virus esophagitis in the immunocompetent host: an overview. Am J Gastroenterol. 2000;95(9):2171-6. [ Links ]
14. Bando T, Matsushita M, Kitano M, Okazaki K. Herpes simplex esophagitis in the elderly. Dig Endosc. 2009;21(3):205-7. [ Links ]
15. al-Samman M, Zuckerman MJ, Verghese A, Boman D. Gastric ulcers associated with herpes simplex esophagitis in a nonimmunocompromised patient. J Clin Gastroenterol. 1994;18(2):160. [ Links ]
16. Wong RCK, Abdul-Karim FW. Atypical herpes simplex esophagitis. Gastrointest Endosc. 2005;61(2):291-2. [ Links ]











 text in
text in