Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.2 Bogotá Apr./June 2015
Three Case Reports of Neoplasms of the Esophagogastric Junction
Roberto Rodríguez MD (1), Isabel Díaz MD (2), Alejandro Flórez MD (2), Fabiola Donado MD. (3)
(1) Internist, Gastroenterologist, Endoscopist in the Gastroenterology and Endoscopy Unit, Professor of Gastroenterology in the Graduate Department of Internal Medicine at the Universidad Libre de Barranquilla and the Clínica General del Norte in Barranquilla, Colombia.
(2) Resident in Internal Medicine at the Universidad Libre de Barranquilla in Barranquilla, Colombia.
(3) Medical Pathologist at the Clínica General del Norte in Barranquilla, Colombia.
Received: 08-09-14 Accepted: 06-04-15
Abstract
Patterns of esophageal tumor incidence have changed in recent decades, now esophageal adenocarcinomas have become more common than squamous cell carcinoma among men. There is evidence of biological differences in behavior among adenocarcinomas and squamous cell carcinomas according to their locations. Many discrepancies exist in the literature regarding the etiology, classification and surgical treatment for these tumors.
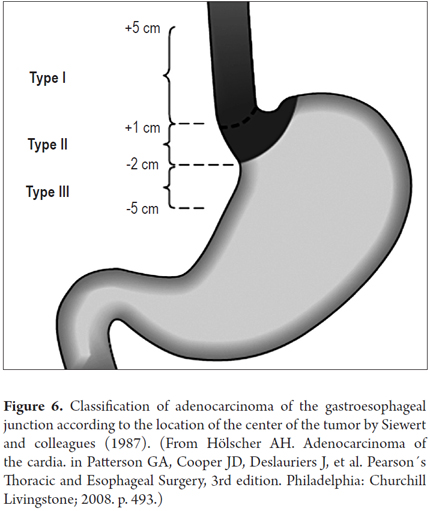
Adenocarcinomas of the gastroesophageal junction include tumors that arise in the distal esophagus as a result of invasion from the proximal stomach through the gastroesophageal junction and the cardiac glands. The usual topographic classification is that proposed by Siewert and Stein. It divides tumors into Type 1, which is used when the compromise is proximal to the gastroesophageal junction, Type 2 when the tumor is found directly in the cardia, and Type 3 when the tumor is in the proximal stomach. Here we present three cases and a review of the diagnostic approach to, and management of, these lesions.
Keywords
Adenocarcinomas of the gastroesophageal junction, Siewert-Stein classification of adenocarcinoma of the esophagogastric junction.
INTRODUCTION
Adenocarcinomas of the gastroesophageal junction include tumors that originate in the distal esophagus, the gastric cardia and the proximal stomach (1). Until the 1960s, esophageal tumors were squamous cell tumors, but in recent decades the incidence of esophageal adenocarcinoma and tumors of the gastroesophageal junction have come to represent more than 60% of all esophageal cancers in the USA (2). This type of cancer is often deadly and has become a major public health problem in recent years. Risk factors such as smoking, obesity and gastroesophageal reflux disease have been associated with the development of adenocarcinoma of the gastroesophageal junction. There are also genetic factors that include deactivation of E-cadherin, IL-1 polymorphism and/or tumor suppressor gene p53. On the other hand, Helicobacter pylori infection and consumption of fiber are associated with lower incidences of this cancer (3). Paradoxically, the Cag A strains of Helicobacter pylori provide the greatest protection against adenocarcinoma of the gastroesophageal junction. Tumors of the gastroesophageal junction occur at the point between the distal esophagus and the proximal stomach where the squamous epithelium of the esophagus changes into the columnar epithelium of the gastric cardia (4).
This article presents three cases of adenocarcinoma of the gastroesophageal junction recently seen in our hospital.
CASE PRESENTATIONS
We report the cases of three patients seen by gastroenterology service of the CARI ESE university hospital in the city of Barranquilla in the Department of Atlántico in Colombia.
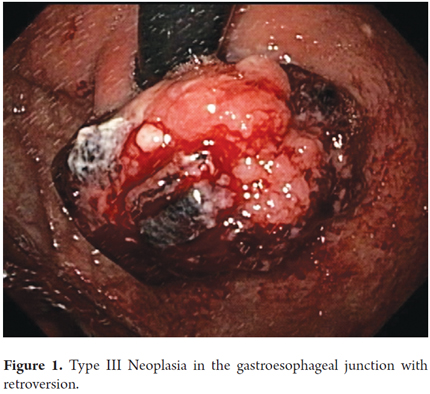
The first two patients were admitted to this institution with upper gastrointestinal bleeding, enlarged hearts to anemia, and constitutional symptoms. Upon admittance, both had hemoglobin levels below 5g/dl. Both were men: one was 59 years old, and the other was 87 years old. Endoscopic examination showed a bleeding 4 x 4 cm exophytic polypoid lesion with jagged edges just below the gastroesophageal junction of the 59 year old patient. Biopsies showed moderately differentiated adenocarcinoma (Figure 1).
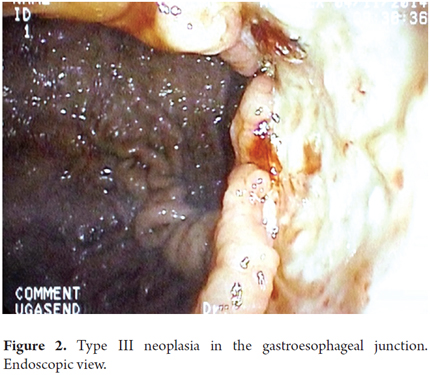
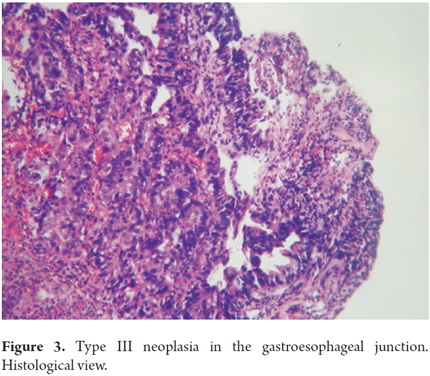
The 87 year old patient presented a 4 x 6 cm ulcerated lesion with whitish adherents and clotted blood located two to three cm below the gastroesophageal junction on the posterior wall. The biopsy reported a poorly differentiated adenocarcinoma. After an evaluation by an oncological surgeon, it was decided to provide only palliative treatment because of the patient's poor prognosis, requirements for intensive support and fatal outcome (Figures 2 and 3).
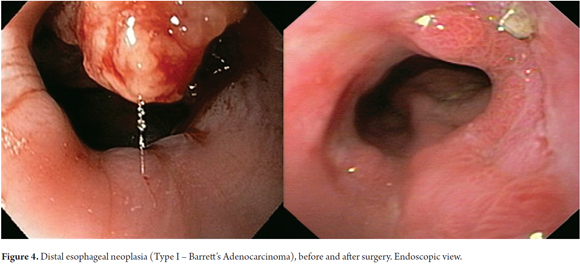
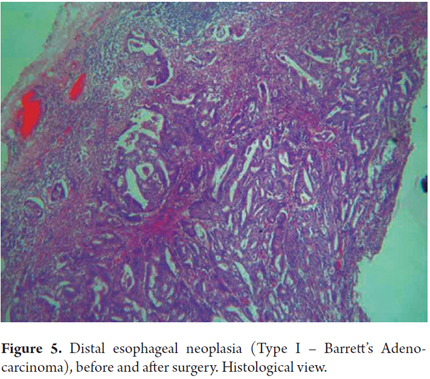
The third case was a 79 years old man who had two coronary stents placement and was being treated with Clopidogrel plus acetyl salicylic acid. He came to the hospital because of intermittent difficulty swallowing solid food over a two month period that had worsened in week prior to consultation. On three occasions he had had melena and coffee ground vomiting. An esophagogastroduodenoscopy showed a raised lesion of approximately 3 cm located in the distal third of the esophagus over a 4 cm hiatal hernia. Biopsies reported Barrett's adenocarcinoma. An esophagectomy of the middle and distal third of the esophagus was performed with simultaneous laparoscopy and thoracoscopy. Histological examination of the surgical specimen showed superficial compromise of the mucosa, submucosa and muscularis propria which had not compromised the lymph nodes (Figures 4 and 5).
DISCUSSION
The gastroesophageal junction is anatomically located at the Angle of His where the esophagus meets the gastric cardia. Endoscopically it is at the most proximal extent of the longitudinal gastric folds (5).
In the USA, the incidence of adenocarcinoma of the esophagus and gastroesophageal junction has increased over the last 40 years while the incidence of gastric adenocarcinoma has decreased. The same trend has also been reported in Canada, Britain, Switzerland and elsewhere in Europe (6-8). According to Globo-can's 2008 estimates, the incidence of gastric cancer in Colombia was 3,959 cases among men per one hundred thousand inhabitants and 3,008 deaths per one hundred thousand inhabitants. In Colombia, esophageal adenocarcinoma ranks second in frequency after prostate cancer and is first cause of death among cancers. Nevertheless, Globo-can's document does not mention the prevalence and mortality of cancers of the gastroesophageal junction (9, 10).
Paradoxically, while the prevalence of gastric cancer if falling, the prevalence of cancer of the gastroesophageal junction is increasing worldwide. Patterns of incidence of esophageal adenocarcinoma are now more common than squamous cell cancer (11).
According to the seventh edition of the TNM (Tumor, nodes, metastasis) staging manual, tumors of the gastroesophageal junction are defined as tumors arising in the gastroesophageal junction or within 5 cm of the junction in the gastric cardia and extending to the proximal esophagus or stomach. Other tumors with an epicenter in the stomach and located more than 5 cm from the junction are classified as gastric antrum and corpus neoplasms (12).
In 1987, Siewert and Stein published an outline of topographic-anatomic subclassification for adenocarcinoma which was adopted and approved by the International Society for Diseases of the Esophagus in 1995 and by the Second International Gastric Cancer Congress in 1997. The classification of adenocarcinoma of the gastroesophageal junction includes all tumors with an epicenter within 5 centimeters on either side of the anatomic z line dividing the esophageal mucosa from the gastric mucosa (Figure 6) (13, 14).
Siewert described three categories of adenocarcinomas of the gastroesophageal junction, based on their anatomical locations:
Type I includes adenocarcinomas that are 5 cm to 1 cm distant from the gastric cardia. These are adenocarcinomas of the distal esophagus that usually occur in an area with specialized intestinal metaplasia of the esophagus (Barrett's esophagus) which can creep into the gastroesophageal junction.
Type II are adenocarcinomas located between 1 cm and 2 cm from the distal gastric cardia. They are considered to be true carcinoma of the cardia, cardia epithelium-derived or short segment intestinal metaplasia, also known as carcinoma of the gastroesophageal junction.
Type III adenocarcinoma are found from 2 cm to 5 cm distal from the gastric cardia. They are subcardial gastric carcinoma that infiltrate the gastroesophageal junction (13).
In most cases, classification is relatively simple. It is based on the results of x-rays, endoscopy, CT scans, and sonography. In some cases it may be difficult to distinguish the type of tumor when it is very advanced locally. Currently, these tumors share common morphological features and have similar prognoses, but the epidemiology, etiology, distribution and pattern of metastases in esophageal tumors, proximal tumors and distal stomach tumors differ.
In our first two cases, adenocarcinomas that originated in the perimeter of the gastric cardia presented as upper digestive tract bleeding associated with enlarged hearts due to anemia. The diagnoses were made by upper endoscopy and biopsies. Because of his age, good nutritional status and the absence of comorbidities, one of the two patients was able to undergo surgery after interdisciplinary management. Unfortunately, the second patient's terminal condition precluded surgery. In the third case, the patient had a history of difficulty swallowing solids and gastrointestinal tract bleeding. After an endoscopy showed a lesion in the distal esophagus, the distal two thirds of the esophagus and the gastric ascent were resected. These cases match the clinical courses of this pathology described in the literature of the world. Cases that are detected early and which have multidisciplinary management sometimes can be cured, but cases that are detected late and that have evolved slowly over longer periods of time are fatal.
On the basis of tumor locations and simple macroscopic views, the first two cases were classified as tumors of the gastroesophageal junction. Nevertheless, this anatomical location has generated controversy. In some cases it is not possible to determine whether the tumor is esophageal or gastric. In these cases Siewert's classification is used (13,15).
According to Siewert's classification, the first two patients had Type III tumors of the gastroesophageal junction since both lesions were more than two centimeters from the gastroesophageal junction. In the third case, the lesion was 5 cm above the gastroesophageal junction. Although overall the prognoses for patients with these tumors is poor, with early diagnosis and multidisciplinary management, they can sometimes be cured. Endoscopic therapy or limited resection is recommended for tumors confined to the mucosa. Tumors that have penetrated the submucosa have high probabilities of involvement of the lymph nodes and therefore require radical resection.
For Type I tumors, transthoracic esophagectomy en bloque with dissection of lymph nodes in two fields is the procedure of choice. If the patient has compromised lung functioning, the transhiatal approach should be considered (13, 15). For Type II and Type III tumors, esophagectomies with proximal gastrectomy or total extended gastrectomy with lymphadenectomy should be considered in order to obtain tumor free margins. All patients with Type III tumors or nodal involvement should be considered for neoadjuvant chemotherapy and radiation therapy (5, 11, 16).
It is important to note that in most cases when the diagnosis is made after the tumor is already in an advanced, stage, surgery is the mainstay of treatment. New protocols of neoadjuvant treatment have shown decreased tumor sizes, clinical stages and increased survival rates, but only about 50% of patients respond to treatment. Patients who undergo neoadjuvant treatment should have a PET scan two weeks after starting treatment, again if there has been no response after the third month of treatment has begun, and again after the first cycle of chemotherapy. If there has been no response, the final option elective surgery (12, 17).
Anastomotic leakage, the most common complication, occurred in two of our three patients (18-20).
CONCLUSION
The incidence of tumors of the gastroesophageal junction has increased worldwide in the past five decades.
Due to the fact that clinical manifestations of these tumors develop late, early diagnosis is difficult. This has a big impact on the prognoses of these patients.
Endoscopy, endosonography and other imaging methods such as CT scans and MRIs help with staging of these lesions.
Neoadjuvant therapy has improved survival rates and prognoses of these patients when tumors have not metastasized and when this treatment is merited.
REFERENCES
1. Stein H, Feith M, Siewet L. Cancer of the esophagogastric junction. Surg Oncol. 2000;9:35-41. [ Links ]
2. Baquet CR, Commiskey P, Mack K, et al. Esophageal cancer epidemiology in blacks and whites: racial and gender disparities in incidence, mortality, survival rates and histology. J Natl Med Assoc. 2005;97:1471. [ Links ]
3. Buas MF, Vaughan TL. Epidemiology and risk factors for gastroesophageal junction tumors: Understanding the rising incidence of this disease. Sem Radiat Oncol. 2013;23(1):3-9. [ Links ]
4. Rusch VW. Are cancers of the esophagus, gastroesophageal junction, and cardia one disease, two, or several? Semin Oncol. 2004;31:444-9. [ Links ]
5. Botterweck AA, Schouten LJ, Volovics A, et al. Trends in incidence of adenocarcinoma of the oesophagus and gastric cardia in ten European countries. Int J Epidemiol. 2000;29:645-54. [ Links ]
6. Ychou M, Boige V, Pignon JP, Conroy T, Bouché O, Lebreton G, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesphageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29(13):1715-21. [ Links ]
7. Hansson LE, Sparén P, Nyrén O. Increasing incidence of carcinoma of the gastric cardia in Sweden from 1970 to 1985. Br J Surg. 1993;80:374-7. [ Links ]
8. Parfitt JR, Miladinovic Z, Driman DK. Increasing incidence of adenocarcinoma of the gastroesophageal junction and distal stomach in Canada. An epidemiological study from 1964-2002. Can J Gastroenterol. 2006;20:271-6. [ Links ]
9. Wayman J, Forman D, Griffin SM. Monitoring the changing pattern of esophago-gastric cancer: Data from a UK regional cancer registry. Cancer Causes Control. 2001;12:943-9. [ Links ]
10. International Agency for Research on Cancer (IARC), World Health Organization (WHO). Globocan 2008: Cancer incidence and mortality worldwide in 2008. Lyon: IARC; 2008. [ Links ]
11. Pardo Ramos C, Cendales Duarte R. Incidencia estimada y mortalidad por cáncer en Colombia 2002-2006. Bogotá: Instituto Nacional de Cancerología; 2010. [ Links ]
12. Sjoquist KM, Burmeister BH, Smither BM, Zalcberg JR, Simes RJ, Barbour A, et al. Survival after neoadjuvant chemotherapy of chemoradiotherapy for resectable esophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12(7):681-92. [ Links ]
13. Mönig SP, Hölscher AH. Clinical classification system of adenocarcinoma of the esophagogastric junction. Recent Results Cancer Res. 2010;182:19-28. [ Links ]
14. Siewert JR, Stein H. Classification of carcinoma of the oesphagogastric junction. Br J Surg. 1998;85:1457-9. [ Links ]
15. Hölscher AH. Adenocarcinoma of the cardia. En: Patterson GA, Cooper JD, Deslauriers J, et al. Pearson´s thoracic and esophageal surgery, 3rd edition. Philadelphia: Churchill Livingstone; 2008. p. 493. [ Links ]
16. Siewert JR, Stein H. Adenocarcinoma of the gastroesophageal junction: classification, pathology and extent of resection. Dis Esophagus. 1996;9:173-82. [ Links ]
17. Fox MP, van Berkel V. Management of gastroesophageal junction tumors. Surg Clin N Am. 2012; 92:1199-212. [ Links ]
18. Edge S, Byrd DR, Compton CC, et al (editors). American Joint Committee on Cancer Staging Manual. 7th edition. New York: Springer; 2010. [ Links ]
19. Devesa SS, Blot WJ, Fraumeni JF Jr. Changing patterns in the incidence of esopagheal and gastric carnicoma in the United States. Cancer. 1998;83(10):2049-53. [ Links ]
20. Weber WA, Ott K, Becker K, Dittler HJ, Helmberger H, Avril NE, et al. Prediction of response to preoperative chemotherapy in adenocarcinoma of the esophagogastric junction by metabolic imaging. J Clin Oncol. 2001;19(12):3058-67. [ Links ]











 text in
text in