Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.3 Bogotá July/Sept. 2015
Fever, Jaundice and Hepatitis: It is not always a Viral Infection
Lina Paola León S. MD. (1), William Otero MD. (2), Martín Gómez MD. (3)
(1) Internal Medicine Resident, National University of Colombia. Bogota, Colombia.
(2) Permanent Medicine Professor, Coordinator of Gastroenterology, National university of Colombia. Gastroenterologist at Fundadores Hospital. Bogota, Colombia.
(3) Profesor of Medicine, Gastroenterology Unit, National university of Colombia. Gastroenterologist at El Tunal Hospital, Bogota, Colombia.
Received: 06-04-15 Accepted: 21-07-15
Abstract
Typhoid fever is a systemic infection caused by Salmonella enterica serotype Typhi as the result of ingestion of contaminated food (fecal-oral). It is a public health problem, especially in developing countries where it is very prevalent and where it is related to poor sanitation. Hepatitis occurs in 1% to 26% of patients with typhoid, so typhoid fever should be suspected when jaundice, fever and hepatitis coexist. Nevertheless, it is difficult to distinguish it from hepatotropic hepatitis virus. The key to diagnosis is that fever disappears in these viral infections while the patient still has jaundice. Final diagnosis requires the isolation of salmonella through blood and/or cultures, but most importantly cultures of bone marrow which have the highest diagnostic yield.
Keywords
Hepatitis, salmonella, enteric fever.
INTRODUCTION
There are slight variations in the liver function profile in 21% to 60% of cases of patients with typhoid fever (1). However, acute hepatitis does not occur very frequently and has only been reported in 1% to 26% of patients (1-3). When present, it is a frequent cause of recurrence of the disease (2, 4). Although clinical manifestations of hepatitis are indistinguishable from viral hepatitis due to hepatotropic viruses (A, B, C, D, E), the diagnosis may be suspected when a patient has fever, jaundice, and hepatitis (increased transaminases) simultaneously. When jaundice appears in patients with hepatitis due to those viruses, the general symptoms including fever disappear (2,4-6). In such cases, we must also rule out other causes such as yellow fever, dengue, chickenpox, and malaria (2, 6). In addition to the coexistence of fever with jaundice and hepatitis, the characteristics of typhoid fever per se are key to the diagnosis. Definitive diagnosis requires isolating the microbes from cultures, and bone marrow culture is the key test (2, 4, 5).
Hepatic compromise by Salmonella was first described in 1889 by William Osler when he reported eight cases of hepatomegaly and jaundice in 1,500 patients with enteric fever (2). This liver compromise secondary to Salmonella infection is known as hepatitis due to Salmonella or typhoid hepatitis. In the stage of Salmonella infection, hepatitis is an entity with good prognosis if antibiotic therapy is initiated promptly. Otherwise, mortality can reach 20% when treatment in patients with severe manifestations such as intestinal perforation and hemorrhaging is delayed (1, 2, 7). Liver compromise occurs more frequently in patients with previous immunosuppression, and it is 15 to 100 times more common in patients with HIV (2, 7). Hence the importance of early diagnosis of this extra-intestinal manifestation in a patient with enteric fever (2).
Epidemiology and Impact
Enteric fever or typhoid fever is a systemic disease that occurs as a result of eating food contaminated by Salmonella typhi or paratiphy (2). Given that it is transmitted by the fecal-oral route, this condition is recognized as an important public health problem in tropical countries and in developing countries (3). It affects approximately 12 to 33 million people worldwide. In Colombia, an incidence of 0.22 cases per 100,000 people was reported for 2011. This is a low level of incidence which is probably related to underreporting of cases (8). About 500 cases are reported annually in the US with a mortality rate of up to 32% in its severe presentation (7).
Due to multi-organ compromise, Typhi S. infection has various clinical manifestations, hence it has been recognized as the great "simulator". The most common manifestations are gastrointestinal, however, extra-intestinal manifestations, which develop as secondary complications from infection by salmonella, account for 10% to 15% of cases (4, 9). They include bleeding, gastrointestinal perforation, typhoid encephalopathy (3-5%), hepatitis with or without cholestasis (26%), which may have a fulminant course (less than 5%) and are often associated to co-infection by hepatitis A and E (10-12), and hematological compromise (7, 10).
Pathophysiology
Typhi Salmonella is a gram negative bacillus, part of the enterobacteriaceae family and can be enteric or Bongori (13). It is a facultative anaerobic bacterium that does not form spores (5, 13). Within its structure it has O9 and O12 lipopolysaccharide antigens, flagellar Hd protein antigen, and Vi capsular polysaccharide antigen that confers its virological ability and that has been linked to the severity of liver compromise (2, 4).
Extra-intestinal compromise because of salmonella depends on the size of the inoculum, the virulence of the serotype, the host immune response, and the presence of local protective factors (7). The size of inoculum determines the length of the incubation period and the onset of bacteremia, which is the actual cause of extra-intestinal infections. However, the specific amount of inoculum needed to cause an extra-intestinal compromise is not known (2, 7, 14). Virulence depends on the ability of the microorganism to invade reticule endothelial cells of organs at distance, the release of endotoxins, and the production of invasin, a protein necessary for phagocytic cells to recognize bacteria (7, 15).
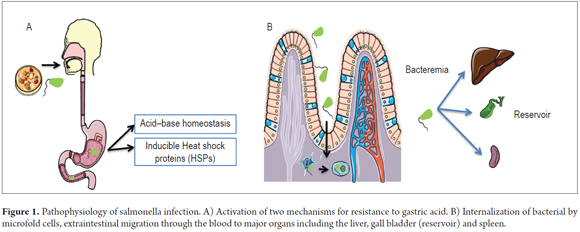
Once the microorganism is ingested, two mechanisms that allow it to survive gastric acid are activated (7, 16). The first is an inducible system of pH homeostasis that is activated when pH falls below 4.0. The second involves the synthesis of acid shock proteins that allow it to survive at a pH of 3.3 (7, 16). When they reach the small intestine, the bacteria are internalized by the M cells of Peyer's patches and are then transported to the intestinal lymphoid tissue. From there, they spread through the blood (4). Hematogenic spread allows bacterial migration to be recognized by the macrophage system of distant organs where it can survive and multiply for a period of 7 to14 days. Then, the phase of bacteremia occurs and results in secondary compromise of organs such as the liver, spleen, bone marrow and gallbladder (2, 4). The latter site is the reservoir of asymptomatic carriers in up to 5% of patients (7, 17). This situation is facilitated by the production of gallstones that allow the attachment of an exopolysaccharide covering to the microorganism which forms a biofilm whose function is to protect the bacterial structures from the action of circulating antimicrobials (Figure 1) (17). The mechanisms involved in hepatic damage are not clearly understood, but it is understood that it can be caused directly by invasion of microorganisms or by immune damage associated with endotoxemia (2, 4, 14). The host's immune response is also a determining factor of the pathogenesis and severity of organ dysfunction secondary to infection by salmonella (4, 7, 15). The subsequent release of pro-inflammatory cytokines by macrophages is responsible for the symptomatic phase of typhoid fever (4, 7, 15).
Clinical manifestations
Clinical manifestations of hepatitis due to salmonella are similar to those found in enteric fever, however, jaundice may be an important marker for the diagnosis of secondary liver compromise (2, 3, 7). Jaundice is found approximately in 12.2% of patients (3). It generally occurs at the beginning of symptoms during the first week of the fever, and it resolves itself with the clinical picture. That is different from viral hepatitis in which fever disappears when jaundice occurs, or in other words, prodromal symptoms disappear with jaundice (2, 13, 18, 19). Hepatomegaly is found in all patients with hepatitis due to salmonella (18-20). Patients may also present splenomegaly. These organ enlargements may be evident on physical examination or by abdominal ultrasound (20). In addition to systemic manifestations such as myocarditis, kidney failure, bleeding disorders, and skin disorders such as skin rash (30%), which are manifestations that can support the diagnosis (7, 9, 15, 17), it is also common to find bradycardia, despite the fever, and this situation is a classic feature of the entity (1, 2, 4, 7). Neuropsychiatric manifestations occur in 10% to 40% of cases and are important and disabling complications since they are associated with severity in the clinical presentation. They include delirium, stupor, coma, meningitis due to typhoid fever, encephalitis, Guillain Barre syndrome, psychosis, mania and apathy. These manifestations can be confused with hepatic encephalopathy, however, the presence of asterixis allows differential diagnosis (2, 4, 7).
DIAGNOSIS
Biochemical alterations
All patients with hepatitis due to salmonella show alterations in liver function (1-3). Elevated levels of transaminase are found in up to 94% of cases and can reach levels that are between three and five times the upper limit (2). Unlike viral hepatitis in which values can exceed 1,000 IU, in hepatitis due to salmonella values are under 300 IU (2). Another common finding is hyperbilirubinemia which is usually in the range of 2 mg/dl to 6 mg/dl, although it may reach 10 mg/dl to 16 mg/dl with a predominance of direct bilirubin (1, 2, 7). Alkaline phosphatase may be normal or slightly elevated, although there have been reports of cholestatic hepatitis (10).
Thrombocytopenia occurs in up to 25% of patients (1, 2, 7). An ALT/LDH ratio of less than 4 may be a useful indicator for differentiating hepatitis due to salmonella from viral hepatitis in which the ratio is greater than five (1, 2). In viral hepatitis, there is an ALT peak, higher bilirubin elevation, and slight elevation of LDH. This is in contrast to hepatitis due to salmonella in which elevated LDH predominates and levels of transaminases and bilirubin are elevated to lesser extents (1, 2). Leucopenia, anemia, and thrombocytopenia can be found in the CBC but are less common in viral hepatitis (9).
Diagnostic methods
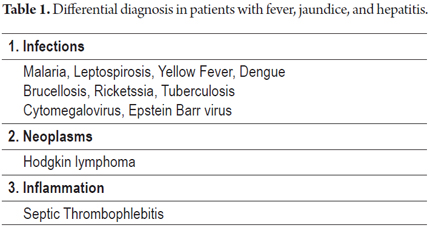
Since the symptoms that occur in hepatitis due to salmonella are nonspecific, the clinical picture may be indistinguishable from other causes of jaundice and fever. The most common entities are those shown in Table 1 (2, 11, 21-25).
For diagnosis, the isolation of salmonella from a culture of the blood, bone marrow, stool, digestive tract secretions or skin lesions is required (2, 4, 17). Blood culture is the diagnostic method most commonly used. It is positive in only 60% to 80% of patients, and its sensitivity is greater in the first week of clinical presentation (2, 4). Bone marrow cultures are the gold standard method for diagnosis, since they are more sensitive than the blood culture method: they test positive in 95% of the cases (2, 4). The usefulness of stool culture depends on the amount of fecal material cultured, but they are positive in only 30% of the patients, so this is not a routine test (2, 4). The Widal test which was developed in the 19th century is a technique of agglutination of antibodies against the lipopolysaccharide O and flagellar H antigen by serial dilution (17, 21). It is a serological test that is rarely used today because it results in cross-reactions with many other antigens and requires that samples are taken in the active period or in convalescence. Consequently, it is considered to be a methodologically difficult technique (17, 21).
Histopathological findings
A liver biopsy is a method that can be useful for differential diagnoses, however, it is not done routinely (2-4, 16, 19, 26). Histologically, hepatitis due to salmonella is characterized by the presence of nodules with hyperplastic Kupffer cells, changes due to focal mononuclear cell infiltration and fat infiltration (2-4, 16, 19, 26).
TREATMENT
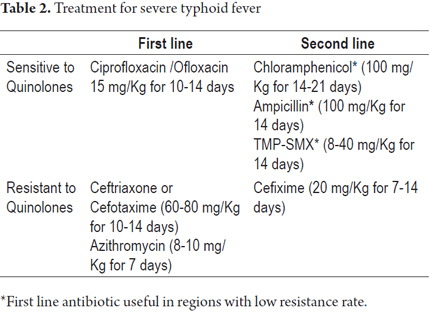
Over 90% of patients with typhoid fever can be managed on an outpatient basis with oral antibiotics. Nevertheless, a small percentage require hospital management (4). These patients also require appropriate nursing care, adequate nutrition, and control of fluids and electrolytes in addition to antibiotics (4, 27). Close monitoring allows early recognition of complications associated with this condition (1, 27). For many years, ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazole (TMP-SMX) were the first-line antibiotics for treating enteric fever, however indiscriminate use of these drugs facilitated the generation of resistant strains (21, 28). In 1972 resistant strains to chloramphenicol were isolated in countries such as Mexico, India, Vietnam, and Korea (29). In 1980 resistant strains to the three first-line drugs were isolated, and that led to the discovery of multidrug-resistant strains (29). Given the need to control the epidemic of such strains, fluoroquinolones, specifically ciprofloxacin, began to be used (5, 29). Its effectiveness at treating drug-resistant strains, good oral absorption, good tolerance, minimal side effects and low cost made it the treatment of choice for this entity (27, 30, 31). Fluoroquinolones are synthetic antibiotics that act by preventing the action of DNA gyrase (topoisomerase II) which is a protein that is necessary for DNA duplication and replication (32). They have adequate tissue penetration and act on still intracellular forms of S. typhi. They also achieve adequate levels in the gallbladder unlike other antimicrobials (27). Also, they produce a rapid therapeutic response with fever clearance in three to five days. The recovery rate is over 96% in patients infected by susceptible strains (4, 28). So far, differences with second and third generation quinolones have not yet been demonstrated (28). A study conducted by Koirala and collaborators that compared gatifloxacin and ofloxacin in the treatment of multidrug-resistant strains showed no superiority in preventing treatment failure (33). However, the use of third and fourth generation quinolones has been associated with cross-resistance to other quinolones required for treating various diseases such as tuberculosis (5). Therefore, the choice of antibiotic should be made on the basis of local antimicrobial resistance (19, 29, 30). Parenteral quinolones are the antibiotic of choice for management of typhoid fever with complications and should be administered for at least 10 days (Table 2) (4, 27). In patients with neurological manifestations, delirium, stupor, and acute behavioral changes, meningitis due to salmonella must be considered (2, 4). The addition of steroids to the treatment of these patients decreases mortality rates (1, 4, 18).
Other treatment regimens include third-generation cephalosporins (Cefixime, ceftriaxone, cefotaxime, cefoperazone) and Azithromycin widely used in pediatric patients with a cure rate of 95% (5, 34). Antibiotics such as aztreonam, imipenem and meropenem are third line schemes that are reserved for strains with reduced susceptibility to quinolones, defined by resistance to nalidixic acid (28).
CONCLUSION
Typhoid fever is a disease (pathological entity) of high impact in developing countries. It is caused by enteric Salmonella typhi serotype that has the ability to invade the intestinal mucosa and organs at distance by hematogenic spread. The most common clinical manifestations are gastrointestinal, however, it may develop extra-intestinal complications, although they are rare and can be highly lethal. Hepatitis due to salmonella is a rare complication whose clinical and biochemical features may be indistinguishable from other causes of hepatitis that are prevalent in tropical countries.
Jaundice is among the most important clinical findings that coincides with fever, unlike in viral hepatitis. The liver function is altered in all patients with hepatitis due to salmonella. In general, transaminases reach values no higher than 300 IU, and in some cases hyperbilirubinemia can develop with predominance of direct bilirubin and thrombocytopenia.
Clinical findings and isolation of the microorganism by cultures, either by blood or bone marrow culture, should be considered for diagnosis.
The treatment of choice in these patients is parenteral quinolones for 10 to 14 days although local resistance rates should be considered when choosing the antibiotic. Despite being a disease with generally good prognosis, its diagnosis involves serious difficulties. Consequently, early diagnosis as a complication typhoid fever in patients with fever, jaundice, and hepatitis is essential.
REFERENCES
1. Karoli R, Fatima J, Chandra A, Singh G. K hepatitis: An uncommon complication of a common disease. J Fam Med Prim care. 2012;1(2):160-2. [ Links ]
2. Pramoolsinsap C, Viranuvatti V. Salmonella hepatitis. J Gastroenterol Hepatol. 1998;13:745-50. [ Links ]
3. Ahmed A, Ahmed B. Jaundice in typhoid patients: Differentiation from other common causes of fever and jaundice in the tropics. Ann Afr Med. 2010;9(3):135-40. [ Links ]
4. Parry CM, Hien TT, Dougan G, White NJ, Farrar JJ. Typhoid fever. N Engl J Med. 2002;347(22):1770-82. [ Links ]
5. Wain J, Hendrikse R, Mikoleit ML, Keddy KH, Ochiai R. Typhoid fever. Lancet. Elsevier Ltd. 1981;79(panel 1):791-3. [ Links ]
6. Otero W. Hepatitis con ictericia y fiebre. Syllabus 1er Curso Internacional de Medicina Tropical y Enfermedades olvidadas. Universidad Nacional de Colombia e Instituto Suizo de Medicina Tropical. 2007 [ Links ]
7. Huang DB, DuPont HL. Problem pathogens: Extra-intestinal complications of Salmonella enterica serotype Typhi infection. Lancet Infect Dis. 2005;5:341-8. [ Links ]
8. Instituto Nacional de Salud. Comportamiento epidemiológico de la vigilancia de fiebre tifoidea y paratifoidea en Colombia, 2011. Inf Quinc Epidemiológico Nac. 2013;18(16):164-74. [ Links ]
9. Parry CM, Thompson C, Vinh H, Chinh NT, Phuong LT, Ho VA, et al. Risk factors for the development of severe typhoid fever in Vietnam. BMC Infect Dis. 2014;14(1):73. [ Links ]
10. Albayrak A, Gunbey SS, Aktas F. Cholestatic hepatitis due to Salmonella typhi. Clin Pract. 2011;1(313):22-3. [ Links ]
11. Husain EH. Fulminant hepatitis in typhoid fever. J Infect Public Health [Internet]. King Saud Bin Abdulaziz University for Health Sciences. 2011;4(3):154-6. [ Links ]
12. Ratnayake EC, Shivanthan C, Wijesiriwardena BC. Cholestatic hepatitis in a patient with typhoid fever - A case report. Acta Gastroenterol Belg. BioMed Central Ltd. 2012;75(1):65. [ Links ]
13. Longo D, Kasper D, Jameson JL, Fauci AS, Hauser SL, Loscalzo J. Harrison Principios de Medicina Interna. 18.a edición. 2012. [ Links ]
14. Dougan G, Baker S. Salmonella enterica Serovar Typhi and the pathogenesis of typhoid fever. Annu Rev Microbiol. 2014;68:317-36. [ Links ]
15. De Jong HK, Parry CM, Van der Poll T, Wiersinga WJ. Host-pathogen interaction in invasive salmonellosis. PLoS Pathog. 2012;8(10):1-9. [ Links ]
16. Waddington CS, Darton TC, Woodward WE, Angus B, Levine MM, Pollard AJ. Advancing the management and control of typhoid fever: A review of the historical role of human challenge studies. J Infect.Elsevier Ltd. 2014;68(5):405-18. [ Links ]
17. Waddington CS, Darton TC, Pollard AJ. The challenge of enteric fever. J Infect. Elsevier Ltd. 2014;68:S38-50. [ Links ]
18. Rungta N, Singhi S, Chaudhary D, Varghese G, Bhalla A, Karthi N, et al. Tropical fevers: Management guidelines. Indian J Crit Care Med. 2014;18:62. [ Links ]
19. Khosla SN. Typhoid hepatitis. Postgraduated Med J. 1990;66:923-5. [ Links ]
20. Nadhim Younis S. The role of abdominal ultrasound in the diagnosis of typhoid fever: An observational study. Travel Med Infect Dis. Elsevier Ltd. 2013;1-4. [ Links ]
21. Darton TC, Blohmke CJ, Pollard AJ. Typhoid epidemiology, diagnostics and the human challenge model. Curr Opin Gastroenterol. 2014;30:7-17. [ Links ]
22. Bathia S, Prabhu M, Saravu M, Docherla B. Spectrum of hepatic dysfunction in enteric fever. Int J Infect Dis. 2010;14:e214-5. [ Links ]
23. Isa SE, Onyedibe KI, Okolo MO, Abiba AE, Mafuka JS, Simji GS, et al. A 21-year-old student with fever and profound jaundice. PLoS Negl Trop Dis. 2014;8(1):3. [ Links ]
24. Schindler M, Kreplak N, Acevedo L, Damis H, Marquez G, Ardaiz M. Ictericia febril colestásica como forma de presentacion de linfoma de Hodgkin. Med Buenos Aires. 2014;74:60-1. [ Links ]
25. Zimhony O, Katz M. A patient with fever and jaundice. QJM. 2012;105:381-2. [ Links ]
26. Madrid M, Huguet J. Enfermedades hepáticas infecciosas. GH Contin. 2006;5:218-21. [ Links ]
27. WHO. Background document : The diagnosis, treatment and prevention of typhoid fever. Commun Dis Surveill Response Vaccines Biol. 2003. [ Links ]
28. Tatavarthy A, Luna V, Amuso PT. How multidrug resistance in typhoid fever affects treatment options. Ann N Y Acad Sci. 2014;1323:76-90. [ Links ]
29. Zaki S, Karande S. Multidrug-resistant typhoid fever: A review. J Infect Dev Ctries. 2011;5(5):324-7. [ Links ]
30. Thaver D, Zaidi AKM, Critchley J, Azmatullah A, Madni SA, Bhutta Z. Fluoroquinolones for treating typhoid and paratyphoid fever (enteric fever). Cochrane Database Syst Rev. 2008;(10). [ Links ]
31. Thaver D, Zaidi AKM, Critchley J, Azmatullah A, Madni SA, Bhutta Z. A comparison of fluoroquinolones versus other antibiotics for treating enteric fever: meta-analysis. BMJ. 2009;338:b1865. [ Links ]
32. Drlica K, Zhao X. DNA gyrase, topoisomerase IV, and the 4-quinolones. Microbiol Mol Biol Rev. 1997;61:377. [ Links ]
33. Koirala S, Basnyat B, Arjyal A, Shilpakar O, Shrestha K, Shrestha R, et al. Gatifloxacin versus ofloxacin for the treatment of uncomplicated enteric fever in nepal: an open-label, randomized, controlled trial. PLoS Negl Trop Dis. 2013;7(10). [ Links ]
34. Trivedi N, Shah P. A meta-analysis comparing the safety and efficacy of azithromycin over the alternate drugs used for treatment of uncomplicated enteric fever. J Postgr Med. 2012;58(2):112-8. [ Links ]











 text in
text in