Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.3 Bogotá July/Sept. 2015
A Case Report of Biliary Tract Intraductal Papillary Mucinous Neoplasm
Martín A. Gómez Z. MD. (1), Javier Riveros V. MD. (2), William Otero R. MD. (3)
(1) Associate Professor. Gastroenterology unit. Department of Internal Medicine. National university of Colombia. Hospital tunal. Bogota, Colombia.
(2) Gastroenterologist. National university of Colombia. Hospital El Tunal. Bogota, Colombia.
(3) Head of Unit of Gastroenterology. National university of Colombia. Clinic founders. Bogota, Colombia.
Received: 10-11-14 Accepted: 21-07-15
Abstract
Papillary mucinous neoplasms are rare and are usually located in the pancreatic pathway. We present a case of a woman with this disease located in the bile duct, an even rarer occurrence. This is the first case in Colombia. We review the literature, describe the tests used for diagnosis, and include an evaluation of the usefulness of a new tool, the Spyglass.
Key words
Cholestasis, mucinous neoplasm, cholangioscopy.
Intraductal papillary mucinous neoplasms (IPMN) are very rare. This is the first case reported in Colombia and one of the few cases found in the world. It is associated with the overproduction of mucus called mucobilia and is included within the spectrum of biliary malignancies with hepatolithiasis. It was initially described as a variant of pancreatic papillary mucinous neoplasms (PPMN) due to their histological similarities (1). IPMNs tends to occur predominantly in women such as our patient. Clinically it presents a cholestatic pattern by overproduction of mucus in bile and a rise in tumor markers such as CEA and CA 19-9 (2). In contrast, PPMNs are more common in men, only 66% present hypersecretion of mucin, it is not associated with cholestasis or elevated bilirubin, and tumor markers are usually normal (3).
CASE PRESENTATION
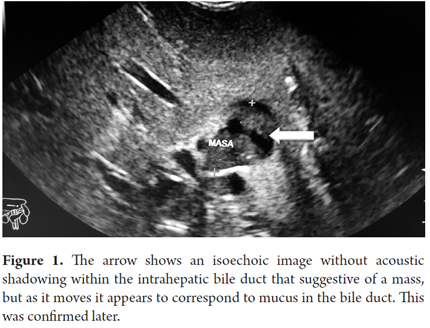
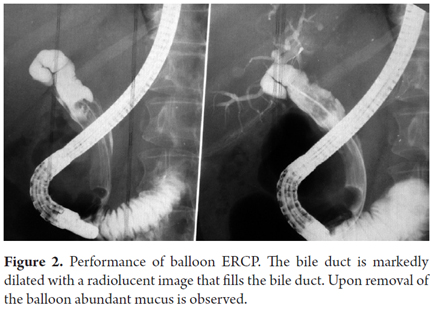
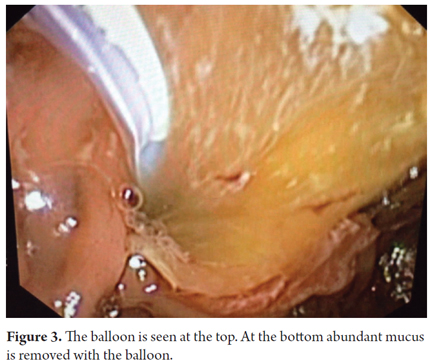
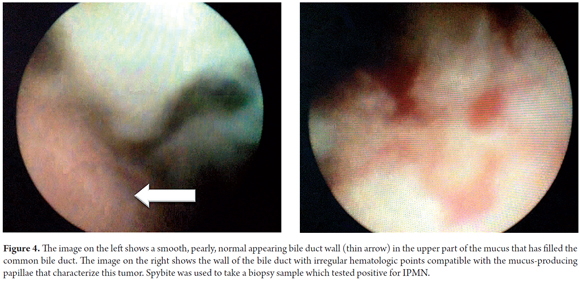
Our patient was a 58 year old woman who had had a cholecystectomy. She consulted because of symptoms compatible with choledocholithiasis after having undergone an ERCP outside of our institution which reported stone removal. Nevertheless, obstructive symptoms and weight loss had continued. She had been tested for tumor markers (CEA and Elevated CA19-9), had had a CT scan and magnetic resonance cholangiopancreatography (MRCP), but the cause of her symptoms remained unclear. She was referred to our institution. We decided to use endoscopic ultrasound to check here marked biliary obstruction. Isoechoic images in the bile duct were compatible with acoustic shadowing of the mucus (Figure 1). Another ERCP found a dilated common bile duct (Figure 2) and abundant mucus but stones obstructed the bile duct (Figure 3). Since the diagnosis had not yet been clarified, the patient underwent SpyGlass choledochoscopy which found abundant mucus (Figure 4) in the bile duct and segmental irregularities of the bile duct wall due to multiple papillae. A biopsy confirmed the diagnosis of papillary mucinous biliary neoplasia (IPMN). The patient underwent chemotherapy given the multiple foci of the lesion. The results were excellent.
DISCUSSION
This paper presents a rare cause of cholestasis which must be considered in the differential diagnosis of biliary obstruction from causes other than calculi which are the most common cause. It also shows how modern techniques such as endoscopic ultrasound allow us to make an educated guess about the cause of the obstruction which in this case was an obstruction due to mucus. This was confirmed with Spyglass which achieved a direct view of the wall of the common bile duct which revealed goblet cells producing mucus which in turn allowed us to confirm the diagnosis.
IPMN is defined as an epithelial tumor in a bile duct characterized by the formation of papillae in the bile duct and mucus production. IPMN can develop anywhere along the biliary tree within the liver or outside of the liver (4, 5). Mucin hypersecretion leads to clogging and consequently to the dilation of the bile duct. Microscopically, IPMN consists of papillae with fine vessels and neoplastic epithelial cells showing a spectrum of atypical cellular architecture ranging from low-grade dysplasia to invasive carcinoma (6, 7). Because of these characteristics, IPMN is considered to be a premalignant lesion that can lead to invasive cholangiocarcinoma (8). In the WHO classification (9), IPMN is classified as low or intermediate grade intraepithelial papillary mucinous neoplasms (PMNs), high-grade intraepithelial neoplasia, and PMN with associated invasive carcinoma. This classification is similar to that of PMNs of the pancreas since PMNs are assumed to have similar formation sequences (10).
The most common clinical manifestations are intermittent abdominal pain, acute cholangitis and jaundice (4, 11). Nevertheless, patients are frequently (29.5%) asymptomatic (12-14) About 30% of patients have a history or concomitant gallstones, as shown in the reports from the Far East and occurred with our patient (15). This has not been reported in Western countries (12). Tumor locations vary with some reports showing that most IPMNs are in the intrahepatic bile duct, but one report shows that the most common location is the porta hepatis (12, 15, 16).
Diagnostic tools other than ERCP exist, as we see in this report. Peroral cholangioscopy using the Spyglass system may have a key role because it allows us to look at the bile duct directly to assess tumor extension along the biliary epithelium, and it also allows direct use of the biopsy forceps to sample papillae which provides accurate information for choosing the best treatment (17).
In conclusion, not every patient with biliary obstructive syndrome has calculi. We must suspect that IPMN is a possibility. It is a premalignant lesion that, unlike cholangiocarcinoma, if detected and treated early is curable.
REFERENCES
1. Kubota K, Nakanuma Y, Kondo F, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: A multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci. 2013;39:123-130. [ Links ]
2. Minagawa N, Sato N, Mori Y. A comparison between intraductal papillary neoplasms of the biliary tract (BTIPMNs) and intraductal papillary mucinous neoplasms of the pancreas (P-IPMNs) reveals distinct clinical manifestations and outcomes. EJSO. 2013;39:554-8. [ Links ]
3. Kim BS, Joo SH, Lim SJ, et al. Intrahepatic Biliary Intraductal Papillary Mucinous Neoplasm With Gallbladder Agenesis: Case Report. Surg Laparosc Endosc Percutan Tech. 2013;23:e61-4. [ Links ]
4. Barton JG, Barrett DA, Maricevich MA, et al. Intraductal papillary mucinous neoplasm of the biliary tract: A real disease? HPB. 2009;11:684-91. [ Links ]
5. Chang WF, Huang GS, Chang WC. An unusual but important cause of biliary obstruction. Gastroenterology. 2013;145:59-62. [ Links ]
6. Lim JH, Jang KT, Choi D. Biliary intraductal papillary mucinous neoplasm manifesting only as dilatation of the hepatic lobar or segmental bile ducts: imaging features in six patients. AJR. 2008;191:778-82. [ Links ]
7. Lim JH, Yi CA, Lim HK, Lee WJ, Lee SJ, Kim SH. Radiological spectrum of intraductal papillary tumors of the bile duct. Korean J Radiol. 2002;3(1):57-63. [ Links ]
8. Zen Y, Fujii T, Itatsu K, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006;44(5):1333-43. [ Links ]
9. Nakanuma Y, Curado M, Fransceschi S, et al. "Intrahepatic cholangiocarcinoma" in: Bosman F, Carneiro F, Hruban RH, Theise ND (editors). WHO Classification of tumours of the digestive system. 4th edition. Lyon, France: IARC; 2010. p. 217-27. [ Links ]
10. Zen Y, Fujii T, Itatsu K, et al. Biliary cystic tumors with bile duct communication: A cystic variant of intraductal papillary neoplasm of the bile duct. Modern Pathol. 2006;19(9):1243-54. [ Links ]
11. Ohtsuka M, Kimura F, Shimizu H, et al. Similarities and differences between intraductal papillary tumors of the bile duct with and without macroscopically visible mucin secretion. Am J Surg Pathol. 2011;35(4):512-21. [ Links ]
12. Rocha FG, Lee H, Katabi N, et al. Intraductal papillary neoplasm of the bile duct: A biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 2012;56(4):1352-60. [ Links ]
13. Onoe S, Shimoyama Y, Ebata T, et al. Prognostic delineation of papillary cholangiocarcinoma based on the invasive proportion: A single-institution study with 184 patients. Surgery. 2014;155(2):280-91. [ Links ]
14. Yeh C, Jan Y, Yeh T, Hwang T, Chen M. Hepatic resection of the intraductal papillary type of peripheral cholangiocarcinoma. Ann Surg Oncol. 2004;11(6):606-11. [ Links ]
15. Kim KM, Lee JK, Shin JU, et al. Clinicopathologic features of intraductal papillary neoplasm of the bile duct according to histologic subtype. Am J Gastroenterol. 2012;107(1):118-25. [ Links ]
16. Jung G, Park KM, Lee SS, et al. Long-term clinical outcome of the surgically resected intraductal papillary neoplasm of the bile duct. J Hepatology. 2012;57(4):787-93. [ Links ]
17. Yang J, Wang W, Yan L. The clinicopathological features of intraductal papillary neoplasms of the bile duct in a Chinese population. Digest Liver Dis. 2012;44(3):251-6. [ Links ]











 text in
text in