Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.4 Bogotá Oct./Dec. 2015
Quality Of Life Predictors in Patients with Chronic Liver Disease in Colombia
Ismael Yepes Barreto MD. PhD. (1), Lourdes Lepesqueur Guillen MD. (2), Sergio Cadavid Asis (2)
(1) Pharos Biomedical Research Center of the coast at the University of Cartagena in Cartagena, Colombia.
(2) Faculty of Medicine of the University of Cartagena in Cartagena, Colombia.
Received: 13-03-15 Accepted: 20-10-15
Abstract
Quality of life is a concept that reflects the positive and negative aspects of the life of an individual. The impact of physical and mental health on feelings of personal welfare are known as health-related quality of life (HRQOL). Cirrhosis causes a number of symptoms and complications that can have a profound negative impact on HRQOL as fatigue, pruritus, loss of self-esteem or depression, among others. So far there have been few studies in Latin America on HRQOL for patients with liver cirrhosis, (9) and those that exist have not studied its determining factors in our population in any detail. The aim of this study is to identify predictors of quality of life in a cohort of patients with liver cirrhosis in Cartagena, Colombia using Version 2 of the 36-Item Short Form Health Survey (SF-36 V2).
Patients and Methods: This cross-sectional study was conducted from June 1, 2014 to August 31, 2014. A Spanish language version of the SF-36 V2 survey was used to consecutively evaluate 49 patients with liver cirrhosis. Epidemiological and clinical information was gathered and analyses were updated at the moment of data entry. Univariate analysis using the t-student test to compare means in the case of dichotomous independent variables and the Pearson correlation coefficient in the case of numerical independent variables was used for initial identification of the determinants of quality of life. The relationship was considered statistically significant at p <0.05.
Results: The etiology (viral versus non-viral) was associated with decreased HRQOL in all scales of SF-36 V2 especially in the PF subscale (- 21.2 points; p = 0.017). This was also true in patients with chronic liver disease secondary to NASH in the DC subscales (-6.18; p = 0.44) and VT (-3.7; p = 0.57). Female patients had lower scores in almost all areas (FF, DC, VT, PF, SF, PE, SM, RCF and the RCM). This relationship was statistically significant in the 40% of the scale areas of the survey. The severity of the disease also had a negative impact estimated by the Child-Pugh classification, transient elastography, and albumin.
Conclusion: Being female and albumin were the variables that were frequently associated with HRQL in our population. The implementation of comprehensive care programs for patients with advanced chronic liver disease is necessary to reduce the impact of disease on the quality of life of these patients.
Keywords
Liver cirrhosis, Latin America, quality of life.
INTRODUCTION
Quality of life is a concept that reflects the positive and negative aspects of the life of an individual. The impact of physical and mental health on the feeling of wellbeing is known as health related quality of life (HRQOL).
Recent reviews have emphasized the importance of identifying the determinants of quality of life in patients with chronic liver disease and the importance of designing comprehensive care programs aimed at reducing its impact on these patients' senses of wellbeing (1-3).
Since sociocultural differences between and among countries and regions are crucial determinants of HRQOL, information from other regions may not be generalizable to Latin America and other developing countries.
Liver cirrhosis is the end stage of various infectious and autoimmune metabolic processes that cause ongoing necroinflammatory reactions that produce the appearance of advanced fibrosis. The epidemiological burden of chronic liver disease is growing and is expected to continue growing worldwide in the coming next years (4-6).
The disease is now recognized to have two stages: compensated and decompensated. The first is characterized by the absence of complications from cirrhosis and has an annual survival rate of 97% to 99%. The decompensated stage begins with the onset of ascites, variceal hemorrhaging and/or encephalopathy and marks a more aggressive disease stage (7, 8).
In every case, regardless of the stage, cirrhosis causes a number of symptoms and complications that can have profound negative impacts on HRQOL. These include fatigue, pruritus, loss of self-esteem and depression. So far there have been few studies in Latin America on HRQOL in patients with liver cirrhosis (9), and there have been no detailed studies of which determinants are factors in our populations.
The aim of this study is to identify predictors of quality of life in a cohort of patients with liver cirrhosis in Cartagena, Colombia through the use of the 36-Item Short Form Health Survey Version 2 (SF-36 V2).
PATIENTS AND METHODS
This is a cross-sectional study that was conducted from June 1, 2014 to August 31, 2014. All patients who had been unequivocally diagnosed with liver cirrhosis by clinical, radiological or histological criteria and who had been referred for treatment to Gastropack SAS (Soluciones Integrales en Gastroenterología y Hepatología - Integrated Solutions in Gastroenterology and Hepatology) were systematically included in this study. Gastropack SAS is clinic which centralizes the first level hepatology health care services of five the largest providers in the city of Cartagena. A trained interviewer used the Castilian version of the SF-36 V2 survey to interview each patient and collected the most up-to-date epidemiological, clinical and analytical information available for each patient on the date of the interview. Patients with hepatic encephalopathy or with physical or mental limitations on filling out the SF-36V2 were excluded. Patients with ascites were not excluded since the sample was representative of patients in all stages of the disease. Qualitimetric Inc. gave permission for the use of the SF-36V2 certified survey and researchers from the International Quality of Life Assessment (IQOLA project) prepared a Castilian version of the survey (10). That version was reviewed by linguists and Colombian investigators who confirmed that this translation was acceptable in Colombia. All patients signed an informed consent form before being included in the study.
Transient elastography
Transient elastography was performed using Fibroscan Touch 502 (Ecosense). This device emits a vibrating wave which passes through the parenchyma of the liver to estimate liver stiffness. The rate at which this wave travels through the body generates an estimate of the degree of fibrosis expressed in kilopascals (kPa): the higher the velocity, the greater the degree of fibrosis that is indicated. All patients must fast for at least eight hours prior to the test. The procedure is performed with the patient in a supine position with the right arm at maximum abduction and after determination of the mid-axillary line. The evaluation of liver stiffness took into account the average of 10 estimates. If the results failed to meet quality criteria of the manufacturer, they were not included in the analysis. To guarantee the reliability of the results an interquartile range < 30% and a percentage of validity (number of valid measurements/total measurements) > 60% were considered essential. The following cut-off points reported in the literature for diagnosis of cirrhosis based on the etiology of the disease were used: NAFLD -17 kPa; hepatitis C -14.5 kPa; hepatitis B - 11 kPa; Alcoholic cirrhosis - 22 kPa; and autoimmune hepatitis - 18.5 kPa. All procedures were performed without charges to the patients as part of the study protocol to estimate the relationship between elastography and the quality of life as well as for confirmation of the diagnosis of cirrhosis.
SF -36V2
The SF-36V2 consists of a 36 item questionnaire that assesses eight areas of HRQoL. It also generates two indicators that summarize the physical and mental components of the scale.
1. Physical functioning (PF): Evaluates the limitation of physical activities due to the disease.
2. Role-Physical (RP): Evaluate the impact of physical health on work and activities of daily life.
3. Bodily Pain (BP): Evaluates patient limitations due to pain.
4. General Health (GH): Evaluates how the subject sees their personal health and its risk of worsening.
5. Vitality (VT): Assesses the degree of fatigue or energy of an individual.
6. Social Functioning (SF): Evaluates whether physical or emotional problems associated with the condition interfere with normal social activities.
7. Role-Emotional (RE): Determines the impact of emotional problems on work and activities of daily life.
8. Mental Health (MH): Assesses the patient's overall mood (depressed, happy, etc.)
9. Physical Component Summary (PCS): Summarizes the physical components of the SF-36V2: PF, RP, BP and GH
10. Mental Component Summary (MCS): Summarizes the mental component of the SF-36V2: VT, SF, RE and MH.
Each of the scales of the SF-36V2 has a range from 0 to 100 where 100 is the best possible score.
Statistical analysis
Numerical variables were expressed as mean +/- standard deviation and categorical variables were expressed as percentages. Univariate analyses to identify the determinants of the quality of life used the t-student test to compare means in the case of dichotomous independent variables and used the Pearson correlation coefficient in the case of independent numerical variables. The relationship was considered statistically significant at p <0.05.
RESULTS
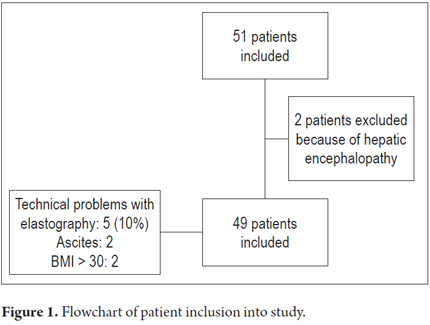
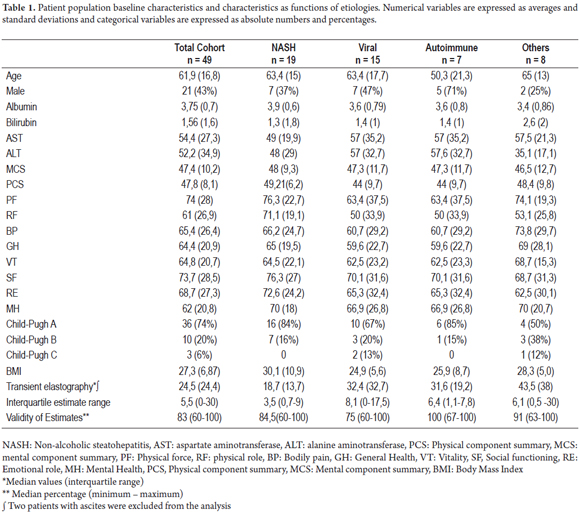
Forty-nine subjects were available for analysis. Figure 1 shows the flow of patient inclusion in the study. Of the sample, 75% had no history of liver decompensation. The sample was composed of equal numbers of men and women. The most frequent etiology was nonalcoholic steatohepatitis (NASH), followed by viral etiologies, and then by autoimmune etiologies. Transient elastography was successfully in 44 patients or 89% of the sample. Technical problems were encountered in patients who were obese and had ascites (n = 3), although valid results were obtained 75% of the subjects with BMI> 30. The average measurement obtained was 24.5 kPa. All measurements met the manufacturer's quality criteria. The baseline characteristics of the patients can be seen in Table 1.
SF 36V2 Scales and Subscales
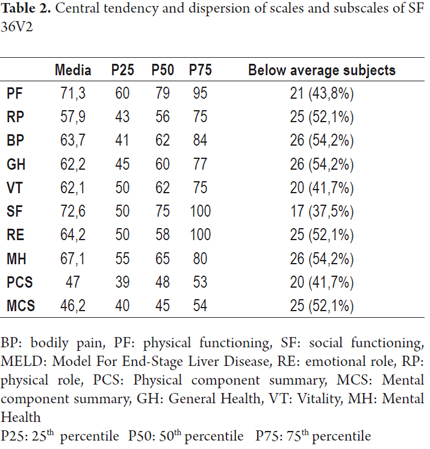
The areas most affected in patients with cirrhosis, with lower scores in the survey, were Role-Physical, General Health, Vitality and Bodily Pain. The largest percentage of subjects (54.2%) with below average scores were encountered in the BP, GH and MH subscales and in the MCS. In contrast, social functioning and physical functioning scales had the best evaluations with 62% of the subjects with above average SF scores, and 56% with above average PF scores (Table 2).
Etiology
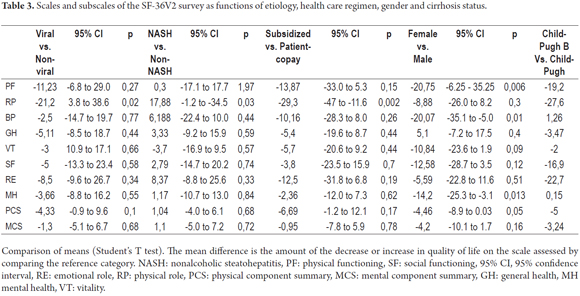
Fifteen patients had cirrhosis of viral origins: five had Hepatitis B and ten had Hepatitis C. These subjects had lower scores on every scale and subscale of the survey. This was particularly important on the RP subscale where these patients had a score that was 21.2 points less than those with other etiologies (p = 0.017).
Moreover, in patients with chronic liver disease secondary to NASH, lower levels of subscales BP and VT were observed, but the RP subscale was 17.8 points higher (p = 0.003).
Age, gender and health care regimen
No relationships with age were found for any of the scales and subscales of the SF-36. In contrast, female sex was associated with lower scores in almost all scales and subscales (PF, BP, VT, RP, SF, RE, MH, PCS and the MCS). This relationship was statistically significant in 40% of the areas evaluated by the survey (Table 3).
Belonging to the subsidized health care system was associated with a decreased quality of life in all areas assessed, but only the lower levels was statistically significant only for the RP subscale for which it was 29.3 points lower (p = 0.002).
Severity
An analysis of the data based on the Child-Pugh classification found lower scores in Stage B and Stage C patients in 8 of the tested areas (PF, RP, GH, VT, SF, RE, PCS and MCS). These differences were statistically significant for PF (-19.2 points; p = 0.05), RP (-27.6 points; p = 0.002) and RE (-22.7 points; p = 0.017).
Similarly, a direct relationship between other estimates of the severity of cirrhosis and quality of life in these patients was also observed. Seven SF 36V2 scales decreased as the elastography values increased. This ratio reached statistical significance in the RP scale (p = 0.014). Also, as MELD scores increased, six scales decreased. Nevertheless, this association was statistically significant only for the RP subscale.
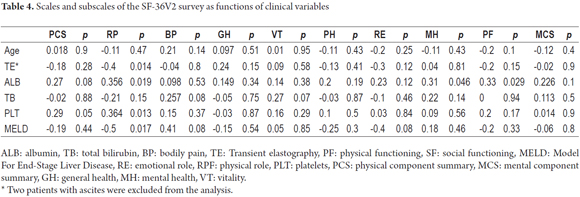
The serum albumin level was one of the factors most often associated with quality of life, showing a statistically significant relationship in 3 of the 10 scales evaluated (RP, MH, PF). Positive and significant relationships between platelet counts and the PCS and RP subscales (Table 4) were also observed.
DISCUSSION
This study is one of the few conducted on the quality of life of patients with liver cirrhosis in Latin America, and to date it is the only one that has estimated the relationship between quality of life and transient elastography.
The areas that seem to be most affected are the impact of physical health on work and activities of daily living, physical limitations because of pain, self-perception of wellbeing and the energy level of the individual. On the other hand, in a cohort composed mostly compensated cirrhosis patients the disease does not seem to intervene in the social performance of study subjects
Albumin and gender were the variables most frequently associated with HRQOL in patients with liver cirrhosis.
Female sex was associated with lower levels of HRQOL on almost every scale and subscale of the survey. These differences were significant in PF, BP, MH and PCS. These results are similar to those observed in a study involving a cohort of 1,103 American and Italian patients with chronic liver disease in which being female was associated with lower quality of life in the same areas (11).
The deterioration observed in our population, seems however to be more marked than in the European-American population. In that study ratings differences between women and men ranged from -3.6 to -10 points while in the Colombian population the differences ranged from -4.46 to -20.7 points. It is possible that these studies may indicate particular needs of females which are not being met within current treatment guidelines.
Patients with Child-Pugh classes B and C had poorer quality of life than did patients in Child-Pugh class A. These differences were significant for the PF, RP and RE scales. Other studies have noted a deterioration in other areas of the SF-36V2 questionnaire for Child-Pugh classes B and C patients but this was not confirmed by our study (11-13). It is possible that the small number of patients with decompensated cirrhosis included in this sample has prevented statistically significant differences from becoming evident.
In addition, although ascites is one of the components of the Child-Pugh classification, none of the patients with decompensated cirrhosis had developed ascites at the time they were interviewed. This may have attenuated the relationship between Child-Pugh classifications and other aspects evaluated.
Albumin levels were significantly associated with the RP, PF and MH subscales. Today, cirrhosis of the liver is no longer considered to have unique static stages, but rather it is accepted that there is a wide range of phases with different degrees of severity and prognoses within the same stage of the disease (14, 15).
Albumin has been identified as one of the main predictors of progression to cirrhosis. It delimits a subpopulation of patients with more severe disease. Two studies have identified compensated subjects exclusively on the basis of albumin levels and the hepatic venous pressure gradient as the only two predictors of decompensation (16, 17). It is possible that the lower values of albumin in this cohort, subtly reflect the presence of more advanced liver disease that affects the physical ability to perform certain activities of daily life. A similar relationship was observed with the platelet count. Almost all scales had higher values when platelet counts were higher, although this reached statistical significance only for the PCS and RP scales. Thrombocytopenia is a common manifestation of portal hypertension syndrome that signals, as does a lower albumin level, the presence of more advanced liver disease in which HRQOL is deteriorating.
These results are consistent with the growing body of scientific information that has shown that subgroups of patients with compensated cirrhosis with different degrees of severity of clinical, histological and hemodynamic findings exist within the overall population of cirrhosis patients (15).
The increase in hepatic rigidity estimated by elastography is associated with higher grades of histological damage (18), with the presence of clinically significant portal hypertension (14-18), and with the risk of decompensation in compensated patients (19-21). Thus, it is possible that the quality of life decreases as histological damage as measured by elastography increases. This relationship seems to be important for RP which was one of the most bly affected areas in this cohort in the assessment of the impact of physical health on work activities and daily life. Some studies have shown that minimal hepatic encephalopathy decreases psychomotor performance and reduces work performance. A study in the Netherlands found that 50% of the patients with minimal hepatic encephalopathy (MHE) do not have permanent jobs, compared with only 15% of patients with cirrhosis who do not have this complication (22). Individuals performing manual tasks seem to be the most strongly affected. About 60% of them are not able to work while only 20% of those who perform managerial jobs are not able to work because verbal intelligence is preserved (23). Although MHE and its impact on HRQOL could not be evaluated, the estimated prevalence in the literature is between 22% and 74% (23). MHE may be one of the reasons that explains the decline in RP as elastography values increase.
Patients with cirrhosis of viral etiologies had lower levels on every scale of the survey than patients with other etiologies. Hepatotropic virus infections have been linked to decreased quality of life independent of the stage of liver disease. A systematic review of the literature identified emotional distress, fatigue, guilt, stigma, limitation of social relationships and work together with decreased sexual activity for fear of transmission of infection as the main determinants of HRQOL in patients with hepatitis C (24). Another study of almost 4,800 infected individuals in the United States observed a prevalence of depression and poor physical condition of 25% to 30%. Sex, race, educational status, employment status, little social support and comorbidities were identified as predictors of these two outcomes (25).
Treatment with pegylated interferon is part of all treatment regimens currently available in Colombia. Its use is associated with symptoms of depression. In fact, it is expected that approximately 53% of patients will develop depression during treatment (26). Patients with viral cirrhosis, especially those infected with hepatitis C, are exposed to other specifically viral factors that, independent of cirrhosis, can have a profound impact on the quality of life and that can explain the lower levels observed in all the scales of the survey for this group.
Belonging to the subsidized health care regimen decreased quality of life in every scale and subscale of SF 36V2. It is possible that this is related primarily to the socioeconomic conditions of this population of which a large proportion has unmet basic needs and not to greater severity of the disease.
MELD (Model for End Stage Liver Disease) was initially developed to identify predictors of short-term mortality after placement of an intrahepatic portosystemic shunt (27). Later it began to be used successfully to predict the prognoses of patients with cirrhosis in different clinical scenarios including prioritization of patients for the active transplant list (28). It is probably the most solidly based cirrhosis staging system in use today. However, no significant associations between any of the scales and MELD scores were observed. This finding is not surprising because variables such as creatinine, INR and bilirubin that relate to states of hemodynamic dysfunction and liver failure characteristic of the later stages of the disease are used in the calculation of MELD, but our cohort was composed primarily of individuals with compensated cirrhosis. Precisely this fact prevented other factors such as ascites, hyponatremia and hepatic encephalopathy that have identified as important determinants of quality of life in other studies from being evaluated. However, although one limitation of our study was its inability to assess HRQOL across the spectrum of the disease, the variations in the different scales and subscales of SF 36V2 in compensated patients suggests that there are significant differences in the areas evaluated in subjects classified at the same stage of the disease that are not being considered in the planning of comprehensive treatment of the disease.
Similarly, these results indicate an opportunity for improvement in the management protocols for compensated cirrhosis. These are currently limited to screening for varices and hepatocellular carcinoma with semiannual clinical and analytical monitoring. What may be needed is a comprehensive intervention strategy to improve physical fitness, mood and self-esteem during follow-up of these patients.
These strategies mainly benefit those patients with compensated cirrhosis who have good survival prognoses. They would increase quality of life adjusted years over those of decompensated subjects who have annual mortality rates of up to 30%.
HRQOL in patients with liver cirrhosis depends on multiple factors regardless of the severity of the disease. The implementation of comprehensive care programs for patients with chronic advanced liver disease can help reduce the impact of disease on the quality of life of these patients.
REFERENCES
1. Orr JG, Homer T, Ternent L, Newton J, McNeil CJ, Hudson M, Jones DE. Health related quality of life in people with advanced chronic liver disease. J Hepatol. 2014;61:1158-65. [ Links ]
2. Loria A, Escheik C, Gerber NL, Younossi ZM. Quality of life in cirrhosis. Curr Gastroenterol Rep. 2013;15:301. [ Links ]
3. Wigg AJ, McCormick R, Wundke R, Woodman RJ. Efficacy of a chronic disease management model for patients with chronic liver failure. Clin Gastroenterol Hepatol. 2013;11:850-858 e851-854. [ Links ]
4. Hyams KC. Risks of chronicity following acute hepatitis B virus infection: a review. Clin Infect Dis. 1995;20:992-1000. [ Links ]
5. Jepsen P, Vilstrup H, Andersen PK, Lash TL, Sorensen HT. Comorbidity and survival of Danish cirrhosis patients: a nationwide population-based cohort study. Hepatology. 2008;48:214-20. [ Links ]
6. Muhlberger N, Schwarzer R, Lettmeier B, Sroczynski G, Zeuzem S, Siebert U. HCV-related burden of disease in Europe: a systematic assessment of incidence, prevalence, morbidity and mortality. BMC Public Health. 2009;9:34. [ Links ]
7. D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-231. [ Links ]
8. D'Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-75. [ Links ]
9. Galant LH, Forgiarini Junior LA, Dias AS, Marroni CA. Functional status, respiratory muscle strength, and quality of life in patients with cirrhosis. Rev Bras Fisioter. 2012;16:30-34. [ Links ]
10. Alonso J, Ferrer M, Gandek B, Ware JE, Jr., Aaronson NK, Mosconi P, Rasmussen NK, et al. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13:283-298. [ Links ]
11. Afendy A, Kallman JB, Stepanova M, Younoszai Z, Aquino RD, Bianchi G, Marchesini G, et al. Predictors of health-related quality of life in patients with chronic liver disease. Aliment Pharmacol Ther. 2009;30:469-76. [ Links ]
12. Bao ZJ, Qiu DK, Ma X, Fan ZP, Zhang GS, Huang YQ, Yu XF, et al. Assessment of health- related quality of life in Chinese patients with minimal hepatic encephalopathy. World J Gastroenterol. 2007;13:3003-8. [ Links ]
13. Younossi ZM, Boparai N, Price LL, Kiwi ML, McCormick M, Guyatt G. Health-related quality of life in chronic liver disease: the impact of type and severity of disease. Am J Gastroenterol. 2001;96:2199-205. [ Links ]
14. Nagula S, Jain D, Groszmann RJ, Garcia-Tsao G. Histological-hemodynamic correlation in cirrhosis-a histological classification of the severity of cirrhosis. J Hepatol. 2006;44:111-7. [ Links ]
15. Garcia-Tsao G, Friedman S, Iredale J, Pinzani M. Now there are many (stages) where before there was one: In search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51:1445-9. [ Links ]
16. Rincon D, Lo Iacono O, Tejedor M, Hernando A, Ripoll C, Catalina MV, Salcedo M, et al. Prognostic value of hepatic venous pressure gradient in patients with compensated chronic hepatitis C-related cirrhosis. Scand J Gastroenterol. 2013;48:487-95. [ Links ]
17. Ripoll C, Groszmann R, Garcia-Tsao G, Grace N, Burroughs A, Planas R, Escorsell A, et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology. 2007;133:481-88. [ Links ]
18. Pavlov CS, Casazza G, Nikolova D, Tsochatzis E, Burroughs AK, Ivashkin VT, Gluud C. Transient elastography for diagnosis of stages of hepatic fibrosis and cirrhosis in people with alcoholic liver disease. Cochrane Database Syst Rev. 2015;1:CD010542. [ Links ]
19. Wang JH, Chuah SK, Lu SN, Hung CH, Kuo CM, Tai WC, Chiou SS. Baseline and serial liver stiffness measurement in prediction of portal hypertension progression for patients with compensated cirrhosis. Liver Int. 2014;34:1340-8. [ Links ]
20. Singh S, Fujii LL, Murad MH, Wang Z, Asrani SK, Ehman RL, Kamath PS, et al. Liver stiffness is associated with risk of decompensation, liver cancer, and death in patients with chronic liver diseases: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11:1573-84 e1571-1572; quiz e1588-1579. [ Links ]
21. Pang JX, Zimmer S, Niu S, Crotty P, Tracey J, Pradhan F, Shaheen AA, et al. Liver stiffness by transient elastography predicts liver-related complications and mortality in patients with chronic liver disease. PLoS One 2014;9:e95776. [ Links ]
22. Groeneweg M, Moerland W, Quero JC, Hop WC, Krabbe PF, Schalm SW. Screening of subclinical hepatic encephalopathy. J Hepatol. 2000;32:748-53. [ Links ]
23. Dhiman RK, Saraswat VA, Sharma BK, Sarin SK, Chawla YK, Butterworth R, Duseja A, et al. Minimal hepatic encephalopathy: consensus statement of a working party of the Indian National Association for Study of the Liver. J Gastroenterol Hepatol. 2010;25:1029-41. [ Links ]
24. Mhatre SK, Sansgiry SS. Development of a conceptual model of health-related quality of life among hepatitis C patients: A systematic review of qualitative studies. Hepatol Res. 2015. [ Links ]
25. Boscarino JA, Lu M, Moorman AC, Gordon SC, Rupp LB, Spradling PR, Teshale EH, et al. Predictors of poor mental and physical health status among patients with chronic hepatitis C infection: the Chronic Hepatitis Cohort Study (CHeCS). Hepatology. 2015;61:802-11. [ Links ]
26. Baranyi A, Meinitzer A, Stepan A, Putz-Bankuti C, Breitenecker RJ, Stauber R, Kapfhammer HP, et al. A biopsychosocial model of interferon-alpha-induced depression in patients with chronic hepatitis C infection. Psychother Psychosom. 2013;82:332-40. [ Links ]
27. Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-71. [ Links ]
28. Freeman RB, Jr., Wiesner RH, Harper A, McDiarmid SV, Lake J, Edwards E, Merion R, et al. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002;8:851-8. [ Links ]











 text in
text in