Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.4 Bogotá Oct./Dec. 2015
Case series: Management of difficult gallstones obstructing bile ducts
Martin Gómez Zuleta MD. (1), Oscar Gutiérrez MD. (2), Mario Jaramillo MD. (3)
(1) Gastroenterologist in the Gastroenterology Unit of the Faculty of Medicine at the National University of Colombia. Gastroenterologist Hospital El Tunal, UGEC. Bogotá, Colombia.
(2) Specialist Assigned to the Gastroenterology and Digestive Endoscopy in Colsanitas and the Clínica del Occidente, Professor (r) of the National University of Colombia in Bogotá, Colombia.
(3) Internist and Gastroenterology resident (final year) at the National University of Colombia in Bogotá, Colombia.
Received: 28-11-14 Accepted: 20-10-15
Abstract
Standard endoscopic techniques of sphincterotomy combined with Dormia basket and/or balloon catheterization can manage 85-90% of the gallstones found obstructing bile ducts. However, when there are several large calculi, when a stone is in an unusual location, or when there are anatomic abnormalities of the bile duct, they become refractory to standard management. Other therapeutic modalities become essential for management of these gallstones. Large or impacted calculi are generally handled with fragmentation techniques such as mechanical lithotripsy. When this fails, electrohydraulic lithotripsy (LEH) or laser lithotripsy (LL) guided by conventional cholangioscopy are usually resorted to. More recently, a system of direct cholangioscopy called Spyglass has been introduced. Endoscopic papillary dilation with a large balloon has also proven useful for management of large and multiple calculi. In cases with altered anatomy that makes access to the papilla difficult, the preferred technique is a transhepatic approach combined with percutaneous fragmentation. In elderly patients whose overall condition is poor, the placement of a biliary stent is the definite choice of technique because it can improve the patient's condition to make possible further endoscopic therapy.
Keywords
Choledocholithiasis, difficult calculi, lithotripsy, cholangioscopy, Spyglass.
INTRODUCTION
Calculi of the common bile duct are present in 7% to 12% of patients who undergo cholecystectomies because of symptomatic cholelithiasis (1). Currently, endoscopic sphincterotomy is the standard method for handling calculi of the bile duct. It is effective in 85% to 90% of cases (2), but for approximately 10% to 15% of patients it is not possible to remove the calculi using this method (3). Failure to remove stones from the bile duct causes biliary obstruction, cholangitis and pancreatitis with consequent increases in morbidity and mortality rates (4).
This paper presents a series of cases and then discusses endoscopic management options for treating difficult calculi in bile ducts.
PRESENTATION OF CASES
Case 1
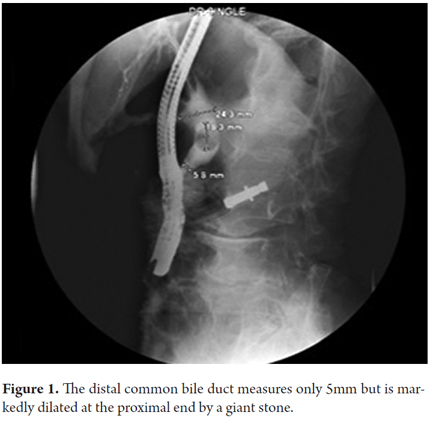
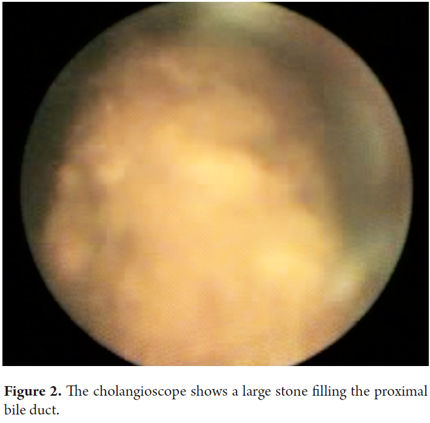
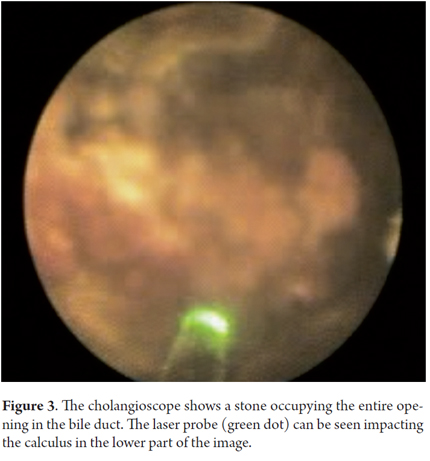
A 62 year old man was admitted to the hospital with abdominal cramping pain associated with jaundice, dark urine and acholia. He had had a major open cholecystectomy 25 years earlier. Laboratory test results showed cholestatic jaundice and normal blood counts, but ultrasound showed dilated intrahepatic bile ducts. An ERCP found that the distal common bile duct was normal, but the proximal bile duct was dilated by calculi ranging from 20 mm to 25mm. Figure 1 shows ERCP with large stones and bile duct measuring only 5mm. Given the disproportionate size of the calculi in relation to the diameter of the distal bile duct, basket extraction and mechanical lithotripsy were ruled out and Spyglass cholangioscopy was performed. Figure 2 shows an image of the calculi taken with the cholangioscope. Figure 3 shows the laser probe impacting the calculi. Complete resolution of the case was achieved.
Case 2
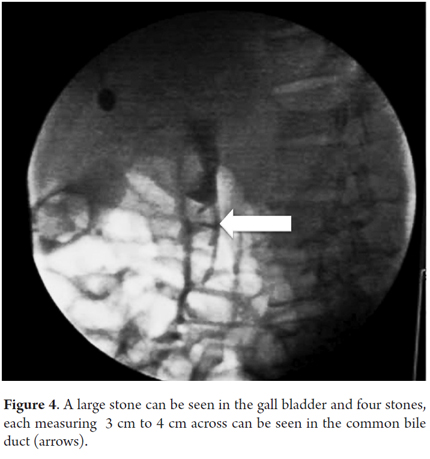
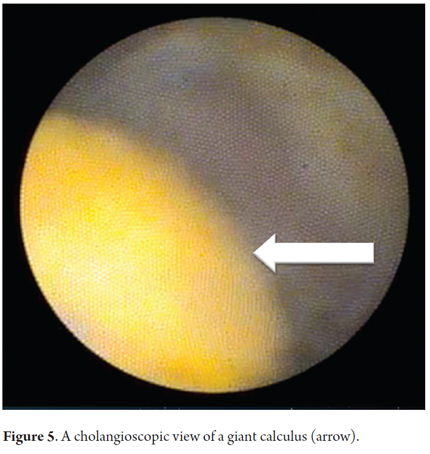
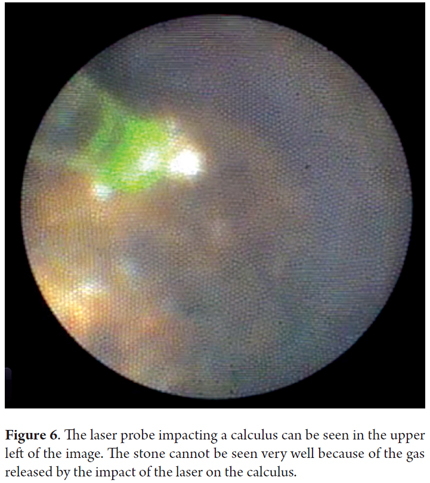
A 51 year old patient had suffered abdominal pain associated with jaundice, fever and chills for eight days. After the pain had intensified for 24 hours, the patient was diagnosed with cholangitis and subsequently underwent ERCP which found giant stones. Figure 4 shows calculi that measure more than 4 cm across and filled the entire bile duct. There was abundant purulent discharge which, combined with the patient's poor condition, required placement of a stent for drainage. Ten days later, a Spyglass cholangioscope was used to perform laser lithotripsy. Figure 5 shows calculi seen through the cholangioscope. Figure 6 shows the laser probe (green dot) which was placed one mm from the calculus and then activated.
Case 3
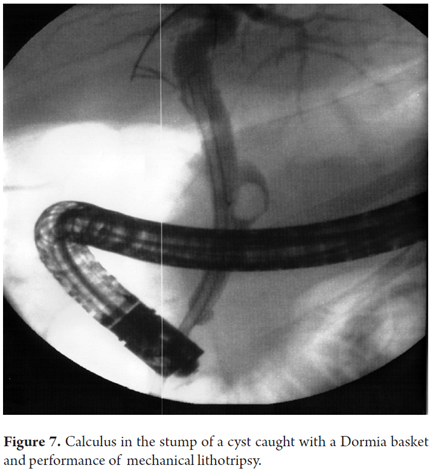
A 62 year old woman who had had a cholecystectomy four years earlier was admitted to the hospital with abdominal pain and fever. Laboratory tests showed leukocytosis and elevated liver function tests. Ultrasound showed dilatation of the proximal bile duct and the possibility of choledocholithiasis. An ERCP revealed evidence cholangitis and a large stone on the stump of a cyst. Several stones were removed from the bile duct, but it was not initially possible to remove the stone embedded in the cyst. Consequently, a stent was placed and a subsequent procedure removed it with a Dormia basket and fragmentation with a lithotripter (Figure 7).
DEFINITION OF DIFFICULT CALCULI OF THE BILE DUCT
Several factors can make it difficult to remove bile duct stones endoscopically. They can be classified into the following categories:
1. Anatomical difficulties accessing the bile duct. These include periampullary diverticula, sigmoid shaped bile ducts, thin distal bile ducts as in our first case, and difficulties resulting from Billroth II gastrectomies and Roux en Y gastrojejunostomies.
2. Multiple calculi
3. Large stone sizes (diameters more than 15 mm, as in Case 2)
4. Unusual shape of calculus, for example barrel-shaped
5. Difficult stone locations such as intrahepatic, cysts as in Case 3, and proximal to a stenosis (5)
6. Mirizzi syndrome in which stones in a cyst cause obstruction of the common bile duct (6)
A prospective study by Kim et al. has found that bile ducts that distances less than 36 mm from the distal branch of the common bile duct and distal bile duct angulation ≤ 135 degrees were the factors that contributed most to the difficulty of endoscopic removal of calculi from the common bile duct (7).
MANAGING DIFFICULT CALCULI IN THE BILE DUCT
Usually, calculi that are less than 10 mm in diameter can be removed by endoscopic sphincterotomy. However, the success rate decreases as the size of the calculi increases (8). Calculi that are more than 2 cm in diameter usually need to be fragmented before being removed to avoid becoming embedded (9). Among the techniques for fragmentation of calculi, mechanical lithotripsy (ML) is the most frequently used since it is simple, cost effective, and readily available. Success rates reported for clearing calculi with this technique range from 84% to 98% (10-13). Nevertheless, this technique may not work for stones larger than 3 cm (13). A prospective study by Garg et al. has concluded that the most important factor for predicting the success of ML is whether or not a calculus is impacted in the bile duct. The failure rate of ML for impacted calculi was 66.6% (P <0.001) (14). The complication rate reported for ML is 3.6% (15), the most frequently reported complications are impaction and broken Dormia cage wires.
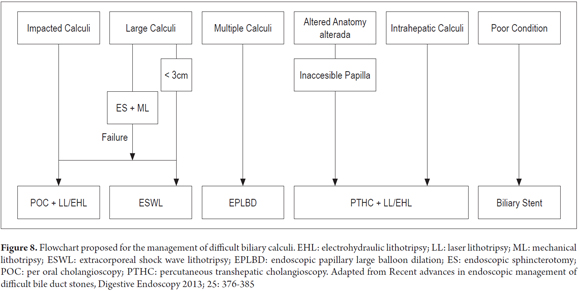
Various procedures can be used in cases that are refractory to ML (Figure 8). Extracorporeal shock wave lithotripsy (ESWL) can be used regardless of the size of the stone, and this technique can be helpful in patients with anatomical abnormalities such as those resulting from Billroth II gastrectomies and Roux en Y gastrojejunostomies. Studies using ESWL for handling difficult calculi report success rates of 73% to 96% for fragmentation and complete removal of calculi (16-23).
Electrohydraulic lithotripsy (EHL) is a technique that can be performed under fluoroscopic guidance or under direct cholangioscopic view (24). When fluoroscopic guidance is used, the two dimensional image hinders the correct positioning of the probe with the ensuing risks of perforating the wall of the bile duct. Consequently, direct visualization with mother-baby cholangioscopy is preferred (25). An ultra-slim cholangioscope (the baby) is inserted through the working channel of the duodenoscope (the mother). Success rates with this technique range from 85% to 98% with complication rates from 2% to 9%. Complications include mild hemobilia, cholangitis and pancreatitis. Perforation of the bile duct has been reported in less than 1% of patients (26-30). Studies of per oral cholangioscopy and laser lithotripsy (LL) have shown a 92% success rate for fragmenting biliary calculi. Hemobilia and cholangitis occurred in 7% of patients (31-33). A prospective randomized study by Neuhaus et al. compared ESWL and LL guided by per oral cholangioscopy in patients with difficult bile duct calculi. It found that laser lithotripsy was more effective than ESWL in terms of clearance of calculi (97% vs. 73%, P <0.05) and duration of treatment (0.9 ± 2.3 days vs. 3.9 ± 3.5 days P <0.001) (20). In the United States, most medical centers prefer to use laser lithotripsy or electrohydraulic lithotripsy guided by cholangioscopy to manage of biliary stones, so ESWL is rarely used there.
Recently, a new per oral cholangioscopy system called Spyglass has been developed. It overcomes some of the limitations of conventional mother-baby cholangioscopy system. The new system can be operated by a single endoscopist, allows 4-way directionality, and provides an independent irrigation channel that maintains a clear field for the cholangioscope during the procedure. Several studies have reported a ductal clearance with LL or EHL through Spyglass in 73% to 91% of patients with gallstones for whom conventional endoscopic therapy was unsuccessful (34-38).
Another option for treating difficult calculi is the technique called endoscopic papillary large balloon dilation. This technique involves dilating the biliary orifice using a larger diameter (12-20 mm) balloon and then removing the stones. Ersoz et al. used this technique in 58 patients for whom conventional endoscopic treatment had been unsuccessful (39). It was possible to remove stones in 88% of these patients. ML was required by 7% of the patients, and minor complications such as cholangitis, pancreatitis and mild bleeding that did not require surgery occurred in 16% of cases. Subsequent studies of combinations of endoscopic papillary large balloon dilation and standard endoscopic sphincterotomy have reported success rates between 94% and 100%, complication rates from 0% to 17%. ML was required in 0% to 33% of cases. This technique can reduce the need for ML and minimize adverse events associated with lithotripsy (39-51).
For older patients and patients who have multiple comorbidities, endoscopic and surgical procedures pose high risks. For these patients, a biliary stent can be used for interim management without removing the calculus until conditions improve (52). The use of stenting for biliary drainage is also mandatory if ERCP cannot clean the entire bile duct and when a second ERCP session is required. Some studies have also reported a reduction of 60% in the size of gallstones after a stent has been in place for one or two years (52).
A study of 28 elderly patients with biliary calculi refractory to conventional endoscopic management found that placement of a biliary stent combined with oral ursodeoxycholic acid for 6 months led to significant reductions in the sizes of stones (53). After this treatment, calculi were removed endoscopically from 26 of the 28 patients using an average of 1.7 ERCP procedures per patient. This combination therapy can be useful for patients with multiple comorbidities who are intolerant of long endoscopic treatments.
MANAGEMENT OF IMPACTED STONES INCLUDING IN MIRIZZI SYNDROME
Managing impacted stones with standard endoscopic technique is usually unsuccessful due to the difficulty of capturing the stone with the Dormia bucket and of advancing the guide through the site of impaction. Consequently, fragmentation techniques such as ESWL or LL, or EHL through per oral cholangioscopy can be very useful.
Binmoeller et al. reported 100% success using per oral cholangioscopy guided EHL to achieve complete clearance of the biliary tract in 14 patients who had Mirizzi syndrome (54). Benninger et al. used ESWL patients to achieve complete ductal clearance in 83% of six patients with Mirizzi Syndrome (55). In contrast, England and Martin reported a series of 25 patients with Mirizzi syndrome who were managed with endoscopic ML, stenting and/or ESWL (56). Endoscopic therapy was successful for full ductal clearance in only 56% of the patients. Of these, 48% required subsequent surgical treatment and 28% required management with long-term biliary stents.
Tsuyuguchi et al (57) used the EHL/LL technique guided by per oral cholangioscopy to treat 122 patients with difficult bile duct calculi. Of these, 53 patients had Mirizzi syndrome, 50 had impacted stones, and 19 had large stones. They reported 96% success in removal of stones from patients with Mirizzi syndrome, and 100% success in removal of impacted stones and large stones.
With these data we can conclude that a strategy management to manage these cases is to use ESWL for calculi that measure about 2 cm, but to use the LL/EHL technique guided by per oral cholangioscopy for patients with impacted stones, including those with Mirizzi syndrome, and for patients with larger calculi.
MANAGEMENT OF INTRAHEPATIC CALCULI
Transpapillary endoscopic removal of intrahepatic calculi poses a challenge because patients may have distal bile duct stenosis with impacted calculi or they may have angulation of the hilar or intrahepatic bile duct. Surgical resection of the affected hepatic segment has been the most widely used therapy because long-term intrahepatic stones may lead to intrahepatic cholangiocarcinoma and because calculi often recur after non-surgical treatment (58). The LL/EHL technique guided by percutaneous transhepatic cholangioscopy offers an alternative therapy when surgical resection is not possible because of the general condition of the patient or because of stones in multiple duct segments. Complete clearance rates of 80% to 85% have been reported in several studies with complication rates of 0% to 2.1%. Complications have included liver lacerations, intra-abdominal abscesses, and septic shock hemobilia. Calculi and/or cholangitis recurred in 35% to 63% of these patients (59-62). After the removal of calculi with this technique, you must leave a catheter to create a transhepatic percutaneous tract (63). Although this technique is the only alternative to surgery for the removal of intrahepatic stones, it is invasive, lengthy and painful.
MANAGEMENT OF PATIENTS WITH SURGICALLY ALTERED ANATOMY
Endoscopic access for ERCP in patients who have had gastrectomies is a challenge. Success depends on the type of reconstruction. In patients with Billroth I reconstruction, a conventional duodenoscope can reach the papilla which makes ERCP possible. For those with Billroth II reconstruction, the papilla must be reached through an afferent loop. The length of the afferent loop varies according to the type of gastrojejunostomy. The afferent loop is short after a retrocolic gastrojejunostomy, so the papilla can be reached with a conventional duodenoscope or a frontal view gastroscope. But after an antecolic gastrojejunostomy, the afferent loop is long and the papilla cannot be reached with conventional equipment. The same applies to Roux-en-Y anastomoses (64). For these patients, the management options are performance of percutaneous transhepatic or surgical intervention. Laser lithotripsy and electrohydraulic lithotripsy guided by percutaneous transhepatic cholangioscopy are alternatives to surgery (65-68), but they have the limitations mentioned above. In addition, this approach is technically impossible if the bile duct is not dilated. Another option is ERCP with enteroscopy, but in our country it is very difficult to obtain ERCP accessories for enteroscopes. The most frequently used option is the combination of a laparoscopic approach plus percutaneous passage of a duodenoscope through the stomach to allow access to the major duodenal papilla.
REFERENCES
1. Freitas M-L, Bell R-L, Duffy A-J. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol. 2006;12(20):3162-7. [ Links ]
2. Seitz U, Bapaye A, Bohnacker S, Navarrete C, Maydeo A, Soehendra N. Advances in therapeutic endoscopic treatment of common bile duct stones. World J Surg. 1998;22(11):1133-44. [ Links ]
3. McHenry L, Lehman G. Difficult bile duct stones. Curr Treat Options Gastroenterol. 2006;9(2):123-32. [ Links ]
4. Cairns SR, Dias L, Cotton PB, Salmon PR, Russell RC. Additional endoscopic procedures instead of urgent surgery for retained common bile duct stones. Gut. 1989;30(4):535-40. [ Links ]
5. Binmoeller KF, Brückner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy. 1993;25(3):201-6. [ Links ]
6. McHenry L, Lehman G. Difficult bile duct stones. Curr Treat Options Gastroenterol. abril de 2006;9(2):123-32. [ Links ]
7. Kim HJ, Choi HS, Park JH, Park DI, Cho YK, Sohn CI, et al. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007;66(6):1154-60. [ Links ]
8. Lauri A, Horton RC, Davidson BR, Burroughs AK, Dooley JS. Endoscopic extraction of bile duct stones: management related to stone size. Gut. diciembre de 1993;34(12):1718-21. [ Links ]
9. Riemann JF, Seuberth K, Demling L. Clinical application of a new mechanical lithotripter for smashing common bile duct stones. Endoscopy. 1982;14(6):226-30. [ Links ]
10. Siegel JH, Ben-Zvi JS, Pullano WE. Mechanical lithotripsy of common duct stones. Gastrointest Endosc. 1990;36(4):351-6. [ Links ]
11. Hintze RE, Adler A, Veltzke W. Outcome of mechanical lithotripsy of bile duct stones in an unselected series of 704 patients. Hepatogastroenterology. 1996;43(9):473-6. [ Links ]
12. Cipolletta L, Costamagna G, Bianco MA, Rotondano G, Piscopo R, Mutignani M, et al. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84(10):1407-9. [ Links ]
13. Chang W-H, Chu C-H, Wang T-E, Chen M-J, Lin C-C. Outcome of simple use of mechanical lithotripsy of difficult common bile duct stones. World J Gastroenterol. 28 de enero de 2005;11(4):593-6. [ Links ]
14. Garg PK, Tandon RK, Ahuja V, Makharia GK, Batra Y. Predictors of unsuccessful mechanical lithotripsy and endoscopic clearance of large bile duct stones. Gastrointest Endosc. 2004;59(6):601-5. [ Links ]
15. Thomas M, Howell DA, Carr-Locke D, Mel Wilcox C, Chak A, Raijman I, et al. Mechanical lithotripsy of pancreatic and biliary stones: complications and available treatment options collected from expert centers. Am J Gastroenterol. 2007;102(9):1896-902. [ Links ]
16. Harz C, Henkel TO, Köhrmann KU, Pimentel F, Alken P, Manegold BC. Extracorporeal shock-wave lithotripsy and endoscopy: combined therapy for problematic bile duct stones. Surg Endosc. 1991;5(4):196-9. [ Links ]
17. Lomanto D, Fiocca F, Nardovino M, Grasso E, Lezoche E, Zarba Meli E, et al. ESWL experience in the therapy of difficult bile duct stones. Dig Dis Sci. 1996;41(12):2397-403. [ Links ]
18. Kratzer W, Mason RA, Grammer S, Preclik G, Beckh K, Adler G. Difficult bile duct stone recurrence after endoscopy and extracorporeal shockwave lithotripsy. Hepatogastroenterology. 1998;45(22):910-6. [ Links ]
19. White DM, Correa RJ, Gibbons RP, Ball TJ, Kozarek RJ, Thirlby RC. Extracorporeal shock-wave lithotripsy for bile duct calculi. Am J Surg. 1998;175(1):10-3. [ Links ]
20. Neuhaus H, Zillinger C, Born P, Ott R, Allescher H, Rösch T, et al. Randomized study of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for difficult bile duct stones. Gastrointest Endosc. 1998;47(5):327-34. [ Links ]
21. Ellis RD, Jenkins AP, Thompson RP, Ede RJ. Clearance of refractory bile duct stones with extracorporeal shockwave lithotripsy. Gut. 2000;47(5):728-31. [ Links ]
22. Sackmann M, Holl J, Sauter GH, Pauletzki J, von Ritter C, Paumgartner G. Extracorporeal shock wave lithotripsy for clearance of bile duct stones resistant to endoscopic extraction. Gastrointest Endosc. 2001;53(1):27-32. [ Links ]
23. Muratori R, Azzaroli F, Buonfiglioli F, Alessandrelli F, Cecinato P, Mazzella G, et al. ESWL for difficult bile duct stones: a 15-year single centre experience. World J Gastroenterol. 2010;16(33):4159-63. [ Links ]
24. Seitz U, Bapaye A, Bohnacker S, Navarrete C, Maydeo A, Soehendra N. Advances in therapeutic endoscopic treatment of common bile duct stones. World J Surg. 1998;22(11):1133-44. [ Links ]
25. Yoo K-S, Lehman GA. Endoscopic management of biliary ductal stones. Gastroenterol Clin North Am. 2010;39(2):209-27, viii. [ Links ]
26. Leung JW, Chung SS. Electrohydraulic lithotripsy with peroral choledochoscopy. BMJ. 1989;299(6699):595-8. [ Links ]
27. Binmoeller KF, Brückner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy. 1993;25(3):201-6. [ Links ]
28. Adamek HE, Maier M, Jakobs R, Wessbecher FR, Neuhauser T, Riemann JF. Management of retained bile duct stones: a prospective open trial comparing extracorporeal and intracorporeal lithotripsy. Gastrointest Endosc. 1996;44(1):40-7. [ Links ]
29. Hui CK, Lai KC, Ng M, Wong WM, Yuen MF, Lam SK, et al. Retained common bile duct stones: a comparison between biliary stenting and complete clearance of stones by electrohydraulic lithotripsy. Aliment Pharmacol Ther. 2003;17(2):289-96. [ Links ]
30. Arya N, Nelles SE, Haber GB, Kim Y-I, Kortan PK. Electrohydraulic lithotripsy in 111 patients: a safe and effective therapy for difficult bile duct stones. Am J Gastroenterol. 2004;99(12):2330-4. [ Links ]
31. Neuhaus H, Hoffmann W, Gottlieb K, Classen M. Endoscopic lithotripsy of bile duct stones using a new laser with automatic stone recognition. Gastrointest Endosc. 1994;40(6):708-15. [ Links ]
32. Schreiber F, Gurakuqi GC, Trauner M. Endoscopic intracorporeal laser lithotripsy of difficult common bile duct stones with a stone-recognition pulsed dye laser system. Gastrointest Endosc. 1995;42(5):416-9. [ Links ]
33. Jakobs R, Adamek HE, Maier M, Krömer M, Benz C, Martin WR, et al. Fluoroscopically guided laser lithotripsy versus extracorporeal shock wave lithotripsy for retained bile duct stones: a prospective randomised study. Gut. 1997;40(5):678-82. [ Links ]
34. Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video). Gastrointest Endosc. 2007;65(6):832-41. [ Links ]
35. Fishman DS, Tarnasky PR, Patel SN, Raijman I. Management of pancreaticobiliary disease using a new intra-ductal endoscope: the Texas experience. World J Gastroenterol. 2009;15(11):1353-8. [ Links ]
36. Seelhoff A, Schumacher B, Neuhaus H. Single operator peroral cholangioscopic guided therapy of bile duct stones. J Hepatobiliary Pancreat Sci. 2011;18(3):346-9. [ Links ]
37. Maydeo A, Kwek BEA, Bhandari S, Bapat M, Dhir V. Single-operator cholangioscopy-guided laser lithotripsy in patients with difficult biliary and pancreatic ductal stones (with videos). Gastrointest Endosc. 2011;74(6):1308-14. [ Links ]
38. Kalaitzakis E, Webster GJ, Oppong KW, Kallis Y, Vlavianos P, Huggett M, et al. Diagnostic and therapeutic utility of single-operator peroral cholangioscopy for indeterminate biliary lesions and bile duct stones. Eur J Gastroenterol Hepatol. 2012;24(6):656-64. [ Links ]
39. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57(2):156-9. [ Links ]
40. Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39(11):958-61. [ Links ]
41. Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13(15):2179-82. [ Links ]
42. Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66(4):720-6; quiz 768, 771. [ Links ]
43. Lee DK, Lee BJ, Hwang SJ, Baik YH, Lee SJ. Endoscopic papillary large balloon dilation after endoscopic sphincterotomy for treatment of large common bile duct stone. Dig Endosc. 2007;19:S52–S6. [ Links ]
44. Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, et al. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67(7):1046-52. [ Links ]
45. Misra SP, Dwivedi M. Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy. 2008;40(3):209-13. [ Links ]
46. Kim HG, Cheon YK, Cho YD et al. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J. Gastroenterol. 2009;15:4298-304. [ Links ]
47. Draganov PV, Evans W, Fazel A, Forsmark CE. Large size balloon dilation of the ampulla after biliary sphincterotomy can facilitate endoscopic extraction of difficult bile duct stones. J. Clin. Gastroenterol. 2009;43:782-6. [ Links ]
48. Itoi T, Itokawa F, Sofuni A et al. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560-5. [ Links ]
49. Kim TH, Oh HJ, Lee JY, Sohn YW. Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg. Endosc. 2011;25:3330-7. [ Links ]
50. Stefanidis G, Viazis N, Pleskow D et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: A prospective randomized study. Am J Gastroenterol. 2011;106:278-85. [ Links ]
51. Rebelo A, Ribeiro PM, Correia AP, Cotter J. Endoscopic papillary large balloon dilation after limited sphincterotomy for difficult biliary stones. World J Gastrointest. Endosc. 2012;4:180-4. [ Links ]
52. Lee DK, Jahng JH. Alternative methods in the endoscopic management of difficult common bile duct stones. Dig Endosc. 2010;22(Suppl 1):S79-S84. [ Links ]
53. Han J, Moon JH, Koo HC, Kang JH, Choi JH, Jeong S, Lee DH, Lee MS, Kim HG. Effect of biliary protesising combined with ursodeoxycholic acid and terpene treatment on retained common bile duct stones in elderly patients: a multicenter study. Am J Gastroenterol. 2009;104:2418-21. [ Links ]
54. Binmoeller KF, Thonke F, Soehendra N. Endoscopic treatment of Mirizzi's syndrome. Gastrointest. Endosc. 1993;39:532-6. [ Links ]
55. Benninger J, Rabenstein T, Farnbacher M, Keppler J, Hahn EG, Schneider HT. Extracorporeal shockwave lithotripsy of gallstones in cystic duct remnants and Mirizzi syndrome. Gastrointest Endosc. 2004;60:454-9. [ Links ]
56. England RE, Martin DF. Endoscopic management of Mirizzi's syndrome. Gut. 1997;40:272-6. [ Links ]
57. Tsuyuguchi T, Sakai Y, Sugiyama H, Ishihara T, Yokosuka O. Long-term follow-up after peroral cholangioscopy-directed lithotripsy in patients with difficult bile duct stones, including Mirizzi syndrome: An analysis of risk factors predicting stone recurrence. Surg. Endosc. 2011;25:2179-85. [ Links ]
58. Mori T, Sugiyama M, Atomi Y. Gallstone disease: Management of intrahepatic stones. Best Pract Res Clin Gastroenterol. 2006;20:1117-37. [ Links ]
59. Jan YY, Chen MF. Percutaneous trans-hepatic cholangioscopic lithotomy for hepatolithiasis: Long-term results. Gastrointest Endosc. 1995;42:1-5. [ Links ]
60. Lee SK, Seo DW, Myung SJ et al. Percutaneous transhepatic cholangioscopic treatment for hepatolithiasis: An evaluation of long-term results and risk factors for recurrence. Gastrointest. Endosc. 2001;53:318-23. [ Links ]
61. Huang MH, Chen CH, Yang JC et al. Long-term outcome of percutaneous transhepatic cholangioscopic lithotomy for hepatolithiasis. Am J Gastroenterol. 2003;98:265-62. [ Links ]
62. Chen C, Huang M, Yang J et al. Reappraisal of percutaneous transhepatic cholangioscopic lithotomy for primary hepatolithiasis. Surg Endosc. 2005;19:505-9. [ Links ]
63. Neuhaus H. Endoscopic and percutaneous treatment of difficult bile duct stones. Endoscopy 2003;35:S31-4. [ Links ]
64. Soehendra N, Binmoeller KF, Seifert H, Schreiber HW (eds). Therapeutic Endoscopy. Stuttgart: Thieme, 1998. [ Links ]
65. Stage JG, Moesgaard F, Gronvall S, Stage P, Kehlet H. Percutaneous transhepatic cholelithotripsy for difficult common bile duct stones. Endoscopy. 1998;30:289-92. [ Links ]
66. van der Velden JJ, Berger MY, Bonjer HJ, Brakel K, Lameris JS. Percutaneous treatment of bile duct stones in patients treated unsuccessfully with endoscopic retrograde procedures. Gastrointest. Endosc. 2000;51:418-22. [ Links ]
67. Jeong EJ, Kang DH, Kim DU et al. Percutaneous transhepatic choledochoscopic lithotomy as a rescue therapy for removal of bile duct stones in Billroth II gastrectomy patients who are difficult to perform ERCP. Eur J Gastroenterol Hepatol. 2009;21:1358-62. [ Links ]
68. Rimon U, Kleinmann N, Bensaid P et al. Percutaneous transhepatic endoscopic holmium laser lithotripsy for intrahepatic and choledochal biliary stones. Cardiovasc Intervent Radiol. 2011;34:1262-6. [ Links ]











 text in
text in