Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.4 Bogotá out./dez. 2015
Clinical case presentation: Diagnosis and treatment of idiopathic intussusception in adults
Carlos Alberto Castro Medina MD (1), Héctor Conrado Jiménez S. MD (1), Sandra Marcela Cardona M. MD (2)
(1) Clinical Saludcoop in Neiva, Colombia.
(2) Clinical Tolima in Ibagué, Colombia.
Received: 11-03-15 Accepted: 20-10-15
Abstract
Intestinal intussusception is an uncommon condition in adults which causes 1% to 5% of intestinal obstructions. Although it is frequently associated with neoplastic pathologies or structural abnormalities of the gastrointestinal tract, up to 10% of cases are idiopathic. In most cases the diagnosis is made after surgery, but with the development of imaging techniques, a diagnosis is possible prior to intervention. This article presents a case in which the diagnosis was made preoperatively by CT scan and presents a review of the relevant literature.
Keywords
Intussusception, adult, intestinal obstruction, idiopathic.
INTRODUCTION
Abdominal pain is one of the most common reasons patients are seen in emergency departments around the world. Causes range from heart diseases to abdominal issues one of which is intestinal obstruction (1). Intestinal intussusception in adults accounts for 1% to 5% of the cases of intestinal obstruction (2). In adults it is most often associated with neoplasms, post-surgical scars and Meckel's diverticulum, but in about 20% of these cases the cause is unknown. We present a case and a review of the relevant literature.
CLINICAL CASE
A 24 year old woman with no relevant medical history came to the emergency room of Clinica Saludcoop in Neiva following approximately four days of burning epigastric abdominal that measured 6/10 on an analog scale of pain. It radiated to her back and was associated with multiple episodes of vomiting. The patient said that she had had no fever, gastrointestinal bleeding or other symptoms. Intravenous analgesia and antiemetics were administered and her symptoms completely resolved. The patient was discharged with an order for outpatient abdominal ultrasound. Two days later she returned to the emergency room because of persistent symptoms. Her abdominal ultrasound report showed a 106 x 49 mm abdominal mass in the epigastric area that appeared to be organ dependent.
Upon admission the patient was in pain, and had tachycardia and second degree signs of dehydration but was hemodynamically stable. Her blood pressure was 115/85 mmHg, her heart rate was 105 bpm, her temperature was 37.2°C, and her respiratory rate was 19 cycles per minute. Her abdomen was soft and depressible and moderately tender in the epigastrium. She was negative for Blumberg's sign and showed no signs of peritoneal irritation. She had very low levels of bowel sounds and no other apparent abnormalities that could be observed in her physical examination.
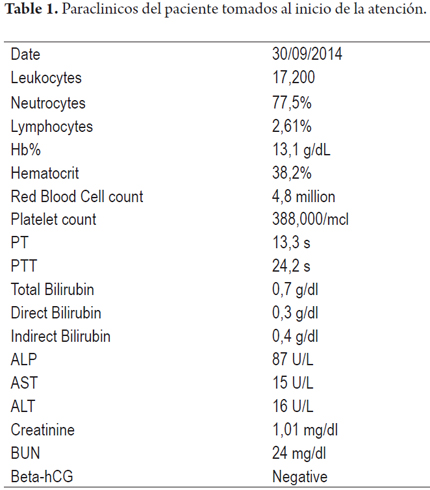
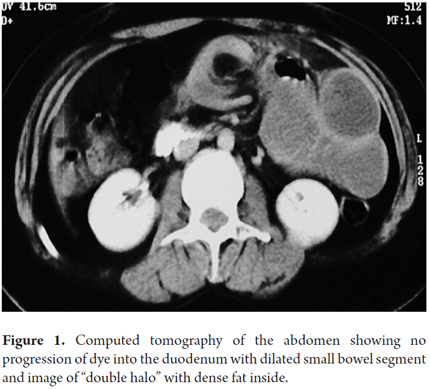
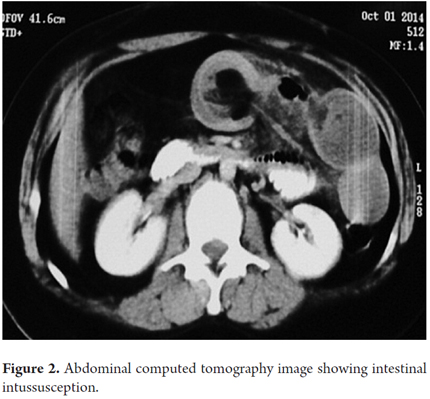
The patient remained hospitalized for medical management of her symptoms, observation, and paraclinical tests (Table 1). She was evaluated by a general surgeon who suggested that she had an intestinal obstruction. An abdominal CT scan (Figure 1) showed no progression of dye into the duodenum, a dilated small bowel segment and a "double halo" image with dense fat inside (Figure 2).
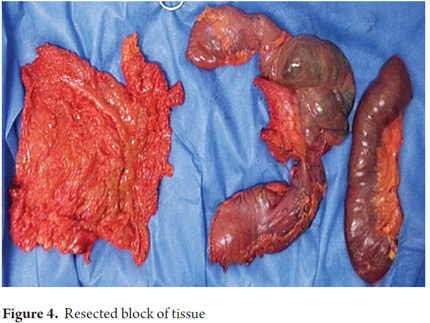
Given the findings from tests and the patient's clinical picture which was highly suggestive of intestinal intussusception, we decided to perform an exploratory laparotomy. We found intussusception of the small intestine 30 cm from the ligament of Treitz (Figure 3) with approximately 70cm of necrosis in the affected jejunum (Figure 4). This was associated with a fluid from the peritoneal reaction and mesenteric lymph nodes. The compromised segment of the jejunum with was resected and a latero-lateral anastomosis of the small intestine was created without complications.
The patient's subsequent clinical evolution was favorable, and she recovered to the point that she was discharged from the hospital. At her follow-up appointment the pathology report (Study No. 14-8078) was received. It ruled out malignancy and showed evidence of small bowel segment with transmural coagulation necrosis, interstitial hemorrhaging, fibrinopurulent peritonitis, and resection margins with acute peritonitis but without ischemia. The report indicated that she had no signs of neoplasia.
DISCUSSION
Intussusception involves invagination of a segment of the intestine and the mesentery, called an "intussusceptum", into the lumen of an adjacent intestinal segment, called an "intussuscipiens". This is a common condition in children who have the classic triad of abdominal pain, bloody stools and palpable abdominal mass (3), but it is a rare condition in adults. Intussusception in adults accounts for only 5% of all cases of intussusception and 1% of the causes of intestinal obstruction (4-6). While it is considered a primary and benign condition in children, in 90% of adult cases it is secondary to a pathological condition or structural trigger. It is frequently diagnosed intraoperatively. Due to the high risk of associated malignancy (65%) in adults, preoperative decompression is not indicated although surgery is required in 70% to 90% of these cases.
Primary idiopathic intussusception accounts for 10% of adult cases while secondary intussusception accounts for the remaining 70% to 90%. Secondary cases are due to structural lesions. These can be benign or malignant and include carcinoma, polyps, colonic diverticula, Meckel's diverticulum, adenomatous polyps, melanomas, adhesions, and iatrogenic damage (1). Their locations can be intraluminal, mural or extramural, but in places where they disrupt normal peristaltic activity and serve as a trigger point capable of initiating invagination of one intestinal segment within another (7). Intraluminal tumors are driven by peristalsis and drag in the tissue upon which they are fixed. Lesions in the intestinal wall prevent proper contract of one segment of the intestine, so that peristaltic force causes the segment to rotate in on itself. Subsequently, this causes intussusception. The most common extraluminal lesions involved are adhesions which pull in an intestinal segment causing the intestine to crease. Then, intestinal movement invaginates the segment that produced the impulse in the first place (19). This causes obstruction of the intestinal contents, vascular compression, edema and eventual ischemic necrosis of the compromised intestinal wall if it does not receive appropriate treatment in time (1).
Generally, intussusceptions are located at the junction between freely moving intestinal segments and retroperitoneal or fixed segments. Intussusceptions have been classified into four categories according to their locations within the intestines (1): Entero-enteral intussusceptions (75%) are located in the small intestine. The case presented here was enteric (2). Colo-colic intussusceptions (14%) are located in the large intestine (3). Ileocolic intussusceptions (5%) involve prolapse of the terminal ileum into the ascending colon (4). Ileocecal intussusceptions (8%) occur when the ileocecal valve is the trigger point of intussusception (3).
Unlike the classical clinical presentation of intussusception in children, the signs and symptoms in adults are nonspecific and the clinical picture can be bizarre (8). A study by Lindor and colleagues at the Mayo Clinic described symptoms in the order of frequency of occurrence as follows: abdominal pain (94%), nausea (76%), vomiting (65%), diarrhea (14%) and bloody stools, most often associated malignant diseases (7%). One percent of the intussusception cases they included were asymptomatic (10). Elsewhere, there have been reports of chronic presentation in which symptoms are consistent with partial bowel obstruction (1).
Preoperative diagnosis is difficult, but advances in the field of radiology have optimized timely diagnosis of this disorder. Simple abdominal radiography can show signs of intestinal obstruction and can provide information about its location (11). The sign of stacked coins, the presence of fluid- gas mixtures and the sign of the ladder are pathognomonic of intestinal obstruction (2). The "target sign" with concentric rings in abdominal ultrasound is a b indication in a transverse view. This changes to the "pseudokidney sign" in the longitudinal view. Diagnostic accuracy is 78.5% (12). Among its drawbacks are the facts that it is operator dependent and it losses sensitivity when there is gas in the intestinal loops (11).
Today abdominal computed tomography (CT) is the most useful technique for preoperative diagnosis of intestinal intussusception in adults. Its accuracy ranges from 58% to 100%, and it can provide information on location, possible causes and signs that suggest that the intestine is not viable (13, 14). It also provides valuable information about any presence of metastases, regional lymphadenopathy and underlying abdominal pathology (11). Three different CT scan images suggestive of intussusception have been described. The "target sign" appears in the earliest stage and corresponds to the image of intussusceptum in the center and edematous intussuscipiens in external rings (2). A "sausage-shaped" image appears in later stages. It represents fat, mesenteric vessels and the intestinal wall. Finally a bilobular, kidney-shaped mass develops due to edema, thickening of the intestinal wall and vascular compromise (12). Magnetic resonance imaging (MRI) shows the same characteristics described in CT scans, but due to advances in the multiplanar capabilities of MRI it has achieved better definition of fat and mesenteric vessels and the layers involved in the intestinal wall (15). Flexible colonoscopy plays a key role in diagnosis in cases of chronic lower GI or subacute bowel obstruction as it not only allows diagnosis of intussusception but also makes it possible to detect the presence of polyps or masses that can cause the phenomenon. Endoscopic reduction of intussusception is not recommended due to the high risk of perforation after resection and also must not be considered when there are signs of ischemia or infection in the intestinal lumen (2).
Management of intestinal intussusception depends on the patient's age group. Reduction of intestinal intussusception in children is most often accomplished with nonsurgical pneumatic or hydrostatic enemas using, but for adults the treatment of choice is surgical resection by laparotomy or laparoscopy. This is because of the frequent discovery of triggering structural anomalies and the high incidence of malignancies (2, 10).
Nevertheless, surgical options for primary reduction and resection of the intestinal segment remain controversial. Many authors recommend primary resection when it is possible but suggest that you should not carry out reduction when there are signs of intestinal ischemia or inflammation (16). The theoretical risks of manipulating the intussuscepted segment include seeding and tumor spread, and perforation and bacteremia. For these reasons resection requires appropriate oncologic edges especially in cases in which the underlying etiology of the segment is known and there is high probability of malignancy (11, 16, 17).
When intussusception occurs in the small intestine, 57% of the tumors are benign and 30% are malignant. The most frequent malignancy is metastasis of melanoma, so primary reduction of the compromised segment can be attempted in these cases. Nevertheless, when the location is in the large intestine the most common cause is malignant neoplasia, adenocarcinomas are most common, followed by leiomyosarcomas and reticulum cell sarcomas. In these cases, surgical resection of the segment for the pathological study is recommended (11, 18, 19). Laparoscopic management of this condition is limited by several factors including the surgeon's experience, the clinical condition of the patient and the degree and type of compromise of the intussuscepted intestinal segment.
CONCLUSIONS
Intestinal intussusception is a rare pathology in adults. Symptoms and signs are nonspecific and suggestive of bowel obstruction. Intestinal intussusception can even present as a chronic condition. Although preoperative diagnosis is uncommon today, imaging techniques such as CT scans and MRI make diagnosis possible as in the case reported here. Due to the high rate of underlying malignancy, the treatment of choice is surgical resection of the intussuscepted segment.
REFERENCES
1. Napora TE, Henry KE, Lovett TJ, Beeson MS. Transient adult jejunal intussusception. J Emerg Med. 2003;24(4):395-400. [ Links ]
2. Poveda G, Polania H, Canal F, Montoya K, Jiménez H. Intususcepción idiopática en el adulto: Reporte de caso y Revisión de la Literatura. Rev Col Gastroenterol. 2013;28:235e9. [ Links ]
3. Amr MA, Polites SF, Alzghari M, Onkendi EO, Grotz TE, Zielinski MD. Intussusception in adults and the role of evolving computed tomography technology. Am J Surg. 2015;209(3):580-3. [ Links ]
4. Briggs DF, Carpathios J, Zollinger AW. Intussusception in adults. Am J Surg. 1961;101:109-13. [ Links ]
5. Donhauser JL, Kelly EC. Intussusception in the adult. Am J Surg. 1950;79(5):673-7. [ Links ]
6. Agha FP. Intussusception in adults. AJR Am J Roentgenol. 1986;146(3):527-31. [ Links ]
7. Vigorita V, Ausania F, Bertucci Zoccali M, Alvarez CF, Nadal BDU, Nuñez JEC. Small bowel intussusception secondary to metastatic melanoma 15 years after complete excision of the primary tumor. Int J Surg Case Rep. 2015;6C:26-8. [ Links ]
8. Zumarán O, Robles C, Villarreal P. Intususcepción en el adulto. An Med Mex. 2006;51(4):188e92. [ Links ]
9. Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226(2):134-8. [ Links ]
10. Lindor RA, Bellolio MF, Sadosty AT, Earnest F, Cabrera D. Adult intussusception: presentation, management, and outcomes of 148 patients. J Emerg Med. 2012;43(1):1-6. [ Links ]
11. Gupta RK, Agrawal CS, Yadav R, Bajracharya A, Sah PL. Intussusception in adults: institutional review. Int J Surg. 2011;9(1):91-5. [ Links ]
12. Byrne AT, Geoghegan T, Goeghegan T, Govender P, Lyburn ID, Colhoun E, et al. The imaging of intussusception. Clin Radiol. 2005;60(1):39-46. [ Links ]
13. Boudiaf M, Soyer P, Terem C, Pelage JP, Maissiat E, Rymer R. Ct evaluation of small bowel obstruction. Radiographics. 2001;21(3):613-24. [ Links ]
14. Beattie GC, Peters RT, Guy S, Mendelson RM. Computed tomography in the assessment of suspected large bowel obstruction. ANZ J Surg. 2007;77(3):160-5. [ Links ]
15. Park SB, Ha HK, Kim AY, Lee SS, Kim HJ, Park BJ, et al. The diagnostic role of abdominal CT imaging findings in adults intussusception: focused on the vascular compromise. Eur J Radiol. 2007;62(3):406-15. [ Links ]
16. Ghaderi H, Jafarian A, Aminian A, Mirjafari Daryasari SA. Clinical presentations, diagnosis and treatment of adult intussusception, a 20 years survey. Int J Surg. 2010;8(4):318-20. [ Links ]
17. McKay R. Ileocecal intussusception in an adult: the laparoscopic approach. JSLS. 2006;10(2):250-3. [ Links ]
18. Behara S, Ahmed N, Attar BM, Hussein R. Primary intussusception in adult. Am J Gastroenterol 2001; 96:180. [ Links ]
19. Warshauer DM, Lee JK. Adult intussusception detected at CT or MR imaging: clinical-imaging correlation. Radiology. 1999;212(3):853-60. [ Links ]











 texto em
texto em