Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.4 Bogotá Oct./Dec. 2015
Histopathological Evaluation of Liver Donors: An Approach to Intraoperative Consultation during Liver Transplantation
Rocío del Pilar López Panqueva MD (1)
(1) Pathologist in the Department of Pathology and Laboratory at the Hospital Universitario Fundación Santa Fe de Bogotá and the Universidad de Los Andes in Bogota, Colombia.
Received: 03-11-15 Accepted: 17-11-15
Abstract
The success of liver transplantation depends largely on the selection of the optimal donor and the best organ. In recent years significant work has been done to develop selection criteria and evidence-based organ assignments.
Histopathological evaluation of liver biopsies plays an important role both in pretransplant evaluation of possibly marginal organs and in the diagnosis and treatment of patients who receive transplants. The use of intraoperative biopsies to evaluate organs found to be marginal in the pretransplant evaluation is opposed by some groups and supported by others. On the other hand, in contrast to the debate about the use of liver biopsies to evaluate donor organs, liver biopsies are still considered to be the "gold standard" for diagnosis of morphological changes such as acute rejection and chronic rejection that occur following transplantation. Nevertheless, the accuracy of biopsies has been questioned due to the variability and subjectivity of these evaluations which is caused primarily by the diagnostic difficulties posed by this disease and by the experience of the pathologist (1). The most important and frequent topics in this area will be discussed in this review. In addition, issues that can cause problems for diagnosing pathologies of the donor organ will be discussed. The article emphasizes pathological features and differential diagnosis. It is organized into three installments. This installment, the first, is about issues relevant aspects to biopsies of the donor organ.
Keywords
Liver biopsy, frozen section, intraoperative consultation, donor liver, pretransplant evaluation, biopsy of donor liver, marginal donor
DONOR EVALUATION
Frozen section intraoperative liver biopsies performed during the evaluation of a potential donor have been very controversial. They are recommended as routine by some groups and disparaged by others.
Transplant centers use clinical and laboratory criteria to determine the usefulness of an organ. Typically an "ideal donor organ" is considered to be one that involves a very low risk of poor initial functioning and graft failure. Other factors that do not directly affect this result, such as technical problems during the procedure, surgical complications, and recurrent disease are not considered. An ideal donor is less than 40 years old, has already suffered brain death, is hemodynamically stable at the time of organ harvesting, has no underlying diseases, and especially has a liver without steatosis and no communicable diseases. Nevertheless, transplant teams now need to consider livers once were considered marginal and to expand the inclusion criteria for potential donors. This is due to declining rates of donation, a mortality rate of patients on the waiting list of close to 10%, and a growing demand from patients in need of orthotropic liver transplantation to treat liver disease. This has led to the use of allografts from older donors, donations after cardiac death, and donations of organs with positive serology for hepatitis B and hepatitis C. It has finally led to identification of the usefulness of each organ under consideration. For these reasons, it is important to identify factors that may lead to primary graft dysfunction, poor initial functioning and poor late graft survival. We must also differentiate between the ideal donor and the ideal donor graft. These reasons are sufficient to require us to be familiar with possible pathological findings, difficulties that may arise and their differential diagnoses. Thus each transplant group must evaluate the pros and cons of this approach and decide on the best course so that each graft minimizes the level of risk to the recipient (2, 3).
WHAT IS THE ROLE OF THE BIOPSY?
A frozen section allows the surgeon to clarify most issues that arise during the evaluation of the donor organ. An intraoperative biopsy is a quick assessment that usually takes less than 30 minutes. It can establish changes in liver architecture, the presence of steatosis, the extent and type of a fat vacuole in the liver to differentiate whether it is a macrovacuole or microvacuole, and it can determine if there is any inflammation or necrosis of hepatocytes. It is considered to be the best option because biopsies fixed in formalin and embedded in paraffin using the fastest processing require 3 to 4 hours which is unacceptably long given the cold ischemia time. A frozen section can usually demonstrate the characteristics of superimposed injuries that can contraindicate transplantation especially in the context of elderly donors, hemodynamically unstable donors and donors with histories requiring morphological clarification. This latter issue is important in cases in which the appearance of the liver is normal but there is a history of alcohol abuse, hepatitis C, or abnormal liver function tests, or when images have been inconclusive. It can also be useful for identifying unexpected findings such as intrahepatic or extrahepatic nodular lesions which absolutely contraindicate transplantation is identified (3).
Unfortunately, using frozen sections extends the selection process, increases cold ischemia time, and increases the cost of the procedure. If the study cannot be done in the same place where the organ is being harvested, there can be difficulties in interpretation generally attributed to overestimation of steatosis (particularly microsteatosis) due to technical artifacts produced by very small drops of water trapped in hepatocytes produced during transport to the pathology laboratory for the freezing process. The benefits of the biopsy should be carefully assessed and all risk factors for both the donor and the potential recipient should be taken into account together with ethical considerations based on justice, equity and the need for transplant using an organ considered marginal (4).
The criteria for acceptance or rejection of a marginal donor organ vary from country to country and transplant center to transplant center. There is neither consensus nor strict and well-defined algorithms. Some of the recommendations about the use of frozen sections are reviewed in this article.
GENERAL BIOPSY CONSIDERATIONS
Successful communication between the surgeon performing the procedure and the pathologist is indispensable. Knowledge of any doubt generated by the study must be reported to the pathologist as this facilitates the study and interpretation of the findings. This is especially true for the visual inspection and palpation of the liver during surgery, even though it is well known that this is a subjective evaluation which is dependent on the surgeon's experience (4, 5).
Ideal Tissue Sample
It is recommended that the size of the biopsy wedge be 1.5 cm x 1.5 cm. Alternately a 2.0 cm long, 0.2 cm in diameter trucut biopsy needle can be used with. Care must be taken to avoid subcapsular preventing scarring and biopsies that are too shallow.
Intraoperative biopsy samples should be taken at the time of vascular clamping from the lower rear margin of the liver and from at least two different sites on the right lobe and left lobe. Preferably from segments three and either 6 or 7. Biopsies taken in this way eliminate diagnostic problems related to subcapsular fibrosis because they get deeper parenchyma. When samples are taken from of a mass or lesion, they must be taken separately and the a biopsy should also be taken from parenchyma free of tumor to assess the possibility of associated chronic liver disease and any other findings that might contraindicate transplantation (6, 7).
Transportation of the sample
The sample must be transported immediately while fresh and kept cool in a dry environment with gauze or in empty jars and refrigerated in a sterile container. Do not use any medium or transport solution. Do not place the biopsy in a towel or wet gauze because it can cause fat to be released from hepatocytes resulting in an underestimation of the degree of steatosis. Also avoid using saline solution it produces artifacts of frozen water crystals in the tissue which hamper interpretation by the pathologist and cause fat percentage overestimation. Similarly, air drying rapidly decreases the amount of fat and compromises the accuracy of the interpretation. Another technique to prevent artifacts is relatively slow freezing at minus 20o C. Do not use liquid nitrogen (4, 8).
Biopsy Processing
The tissue sample must be dried gently. If possible, divide the sample into two. Place a fragment in Optimal Cutting Temperature compound (OCT) and freeze at -26 ° C in cryostat. Cut 4 micron thick slices and color with hematoxylin and eosin. After controlling freezing, fix in 10% neutral buffered formalin. Follow the same procedure with the other half of the tissue sample for routine processing and special histochemical studies if required. Definitive studies should be done in cuts paraffin (frozen control fragment and unfrozen) which is very important for subsequent correlation of findings previously noted.
Complementary methods
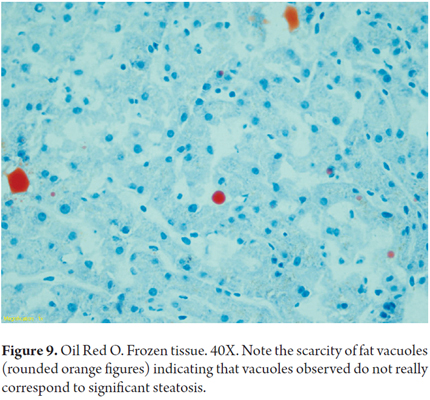
For the evaluation of lipids in frozen section biopsies, it can be useful to use Oil Red O stains for fat which is sensitive for detecting steatosis and increases the amount of fat observed. Nevertheless, artifacts are produced by staining sinusoids and the presence of extracellular vacuoles overstates the presence of fat. It is also highly dependent on the knowledge of histological laboratory technician, and this technique is not routinely available in pathology laboratories (4, 8, 9).
What factors influence the success of a transplant?
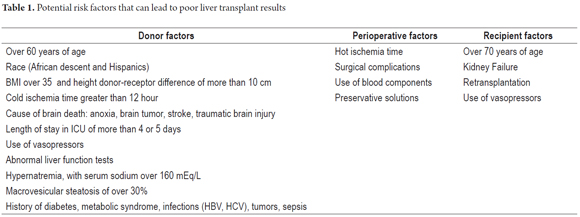
There are many factors that increase the risk of liver transplant failure. Some factors are donor dependent, some depend on the recipient, and others depend on the timing of donation and perioperative conditions. Some of these factors are listed in Table 1. When a donor organ has one or more of these factors, it should be considered marginal. When three or more are present, it should be considered marginal with expanded criteria. Some groups recommend using these organs only in low-risk recipients (with low MELD scores) and high levels of comorbidities. Other studies have shown that demographic characteristics such as age, race, weight and height of the donor as well as the characteristics of the donor's death are important for obtaining the best results (10).
Height, chest girth and weight
For every 10 cm that the donor is shorter than the recipient, the risk of graft loss increases. Similarly, higher BMI are linked to increased levels of steatosis. Anthropometric and imaging parameters are used to estimate the most appropriate volume and size of donors especially in cases of living-related donors (11).
Race
Livers donated by African Americans and Hispanics have approximately 21.5% to 30% more risk of graft failure at 1 year than do livers from white donors. In some studies this difference was not statistically significant (12).
Age
The age of the donor is one of the most widely studied factors, and in recent decades donor age has notably increased. Clearly, age affects the regenerative capacity of the liver. Nevertheless, it has been shown that by minimizing other factors such as cold ischemia time (ideally this should be less than 8 hours), hypernatremia and the presence of mild or minimal steatosis, the short and long term post-transplant prognoses are very similar to those of organs donated by people who are under 60. The majority of groups recommend that donors older than 70 not be used but that, if one is used, it must not have any other associated risk factors (13-15).
Chronic infections
Chronic hepatitis C infection is another factor that worsens the functioning of a marginal liver and that is related to age. When a recipient's blood has tested positive for hepatitis C, the donor's age again becomes a factor to consider because there is a relationship between the progression of fibrosis and advanced age that favors earlier and more serious recurrences. For this reason, it is recommended that elderly donors not be assigned to recipients who are infected by the hepatitis C virus.
Ischemia time
Cold ischemia time of more than 12 hours produces exponentially increasing incidences of graft dysfunction in elderly patients. Each additional hour of cold ischemia time increases the risk of graft loss by 1%. Finally, age alone can cause other associations and comorbidities such as macrovesicular steatosis that place graft survival at risk (3).
Cadaveric Organ Donation
Cadaveric organs can be used in a manner similar to that of livers from donors over the age of 70 when no other associated risk factors exist (10).
HISTOPATHOLOGICAL FEATURES OBSERVABLE IN AN INTRAOPERATIVE BIOPSY
Steatosis
Hepatic steatosis is an independent risk factor which is considered to be one of the most important criteria a surgeon faces in harvesting a donor organ. The organ must be macroscopically inspected by simply observing whether the liver has turned yellow. Nevertheless, there is a poor correlation between evaluation of surgeons and the degree of steatosis when it is over 35%. This is where intraoperative frozen section biopsy has shown to be of great value (3).
About 25% of donor livers have some degree of steatosis which is most frequently related to overweight donors, metabolic disorders, and donor use of alcohol or drugs. In addition, there is no agreement on the percentage of steatosis that is acceptable which varies from transplant unit to transplant unit, and this is related to the fact that the effect of steatosis after transplantation have not been well established (7, 8).
A recent systematic review has shown that steatosis is associated with worse clinical outcomes and increased morbidity of recipients and that it appears to be associated with increased susceptibility to ischemia. Fat accumulation in hepatocytes and increased cell volume cause a deterioration of liver microcirculation which is associated with decreased ATP production capacity and storage, increased lipid peroxidation and release of tumor necrosis factor (16).
One reason for decreased survival of grafts with significant percentages of steatosis is the increased number of complications during surgery related to intraoperative blood loss. This includes slower recovery of synthetic function and increased susceptibility to further injury. In addition ischemia/reperfusion damage probably occurs because of impairment of hepatic metabolism during cold ischemia, increased oxidative stress during reperfusion and poor tissue preservation.
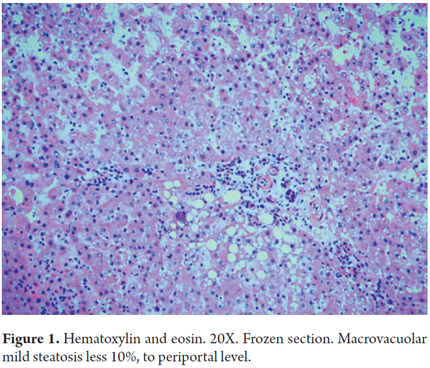
To use an organ tranquilly with minimal impact on the outcome after transplantation, most groups accept donor organs with mild macrovacuolar steatosis of less than 30% (16).
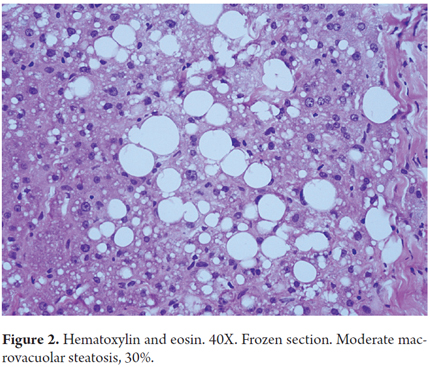
While the use of donor organs with moderate steatosis over 30% but less than 60% is discussed, the incidence of primary dysfunction after these transplants can reach 15% and the rate of delayed graft dysfunction approaches 35%. These organs are more susceptible to bleeding and fibrinolysis (3). They can be used by minimizing other risk factors as much as possible and in certain circumstances such as when cold ischemia time is short and the recipient has a low MELD score. Proper selection of the recipient and shorter cold ischemia time are critical to the successful use of allografts with moderately steatosis (3, 7-9, 16).
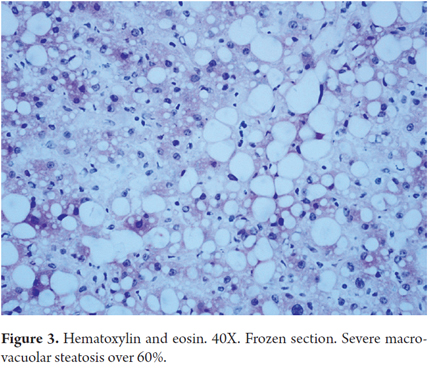
Very severe steatosis affecting more than 60% of the tissue volume carries such a high risk of primary graft dysfunction that the current consensus is to avoid their use. Very few groups accept them as donor organs and only under very specific conditions such as inclusion in research protocols using preservation solutions with very short cold ischemia times and very carefully selected recipients (3). Figures 1, 2, and 3 show various examples.
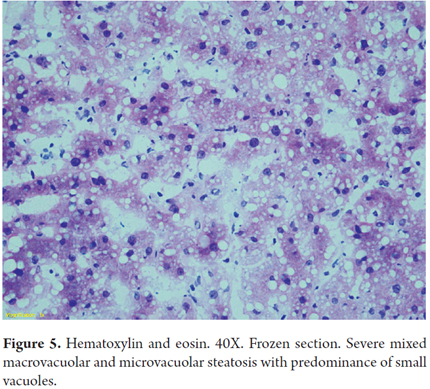
The literature is not clear about what happens when both macrovesicular and microvesicular steatosis are present nor does the literature propose allowable percentages in these cases. In many cases the two are added together to make a total percentage of steatosis with a specification that the percentage of macrovacuolar steatosis is what matters in making the final decision about whether to accept an organ (Figures 4 and 5).
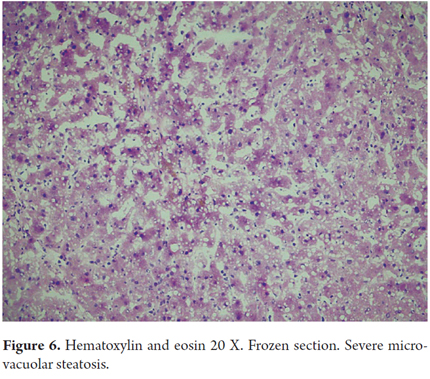
Small or microvacuolar steatosis rarely presents and is an unusual finding in livers considered "healthy," but it is not uncommon to find it in donor biopsies as an artifact or as the result of hot ischemia. It is accepted that regardless of the percentage of tissue affected, microvesicular steatosis does not affect graft survival or produce increased risk of primary graft dysfunction except in patients undergoing retransplantation (Figure 6) (17-19).
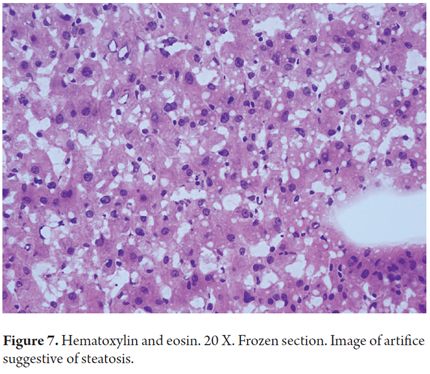
The most common error made by pathologists in interpretation of intraoperative biopsies is overestimation of macrovacuolar steatosis related to artifacts such as edema, swelling and vacuolization of tissue during transport and processing of the biopsy. This can have a significant impact in clinical centers where 30% of donor livers with steatosis are discarded. Also, the freezing process itself can produce microvacuole artifacts or give the appearance of severe sinusoidal dilation. To improve steatosis classification accuracy when the percentage of tissue affected is borderline, an auxiliary of Oil red O staining can be used (Figures 7, 8a, 8b and 9) (7).
Infection and Inflammation
A history of viral hepatitis is a relative contraindication. When there is a donor who is positive for hepatitis C, the donated liver cannot be used in a recipient who has tested negative for the disease. Nevertheless, if the recipient is infected with hepatitis C, a donor organ that has tested positive can be accepted. These patients have no more post-transplant recurrences than those who receive uninfected organs. The transplant recipient and her or his family should be informed of this situation (20).
Recipients with hepatitis B cirrhosis can receive livers from donors who are anti-HBc positive because they will receive antiviral prophylaxis.
If there is one clinical criterion that should raise suspicion of possible fibrosis in the donor organ, it is the determination of the degree of inflammation and architectural alterations in the frozen section. Inflammation caused by lymphocytes, especially portal and lobular inflammation, is frequently found when a donor has spent several days in an intensive care unit. If inflammation is not accompanied by other changes, and if the possibility of viral hepatitis has already been ruled out, inflammation does not contraindicate organ donation. Mild or minimal swelling and mild fibrosis with fibrous portal expansion is accepted (21).
It is well established that brain death predisposes the donor to infection due to deterioration of the immune system and onset of hemodynamic instability that promote bacterial translocation.
Bacterial infection in a donors is another risk factor for graft failure. The possibility of transmission of a bacterial infection in cases of bacteremia in a donor is very low. Even when the culture from the donor has bacteria levels as high as 50%, the transmission rate remains as low as 4%. Careful microbiological monitoring of graft recipients and appropriate antibiotic therapy is recommended to minimize the risk. The only significant predictor of infection in the donor is an ICU stay of three or more days. The role of frozen sections is limited. Probably in the not too distant future objective evidence of an infection in the donor may be more readily determined by genotyping. Unfortunately, these techniques are not yet widely available in pathology laboratories nor is their use as fast or economic as would be required for routine use (21, 22).
Necrosis
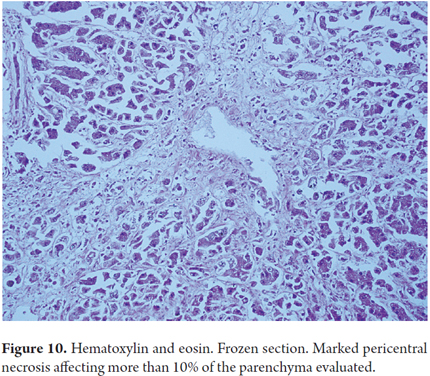
Many events can cause necrosis in a potential donor, but those related to ischemic events such as hypovolemia and hypovolemic shock are especially important. Necrosis in the pericentral area (zone 3) due to ischemia may be evident in the frozen section. However, a when the tissue was immersed in saline solution underestimation of the necrosis is common because of distortion of morphology including clumping and cytoplasmic edema. This can also occur at the time of transplantation as the result of longer cold ischemia time, especially in organs donated after cardiac death. Pericentral necrosis is predictive of graft failure. There is no consensus on permitted percentage, but one cut-off point that is acceptable is 10% of confluent necrosis (Figure 10) (12, 23).
Tumors and tumor-like lesions
Liver allograft recipients have high risks of de novo tumors from lymphoproliferative syndromes including skin cancer and tumors of the upper respiratory tract and intestines. This is especially true for patients with alcoholic cirrhosis and hepatitis C. Risk of disease transmitted by the donor is very low, less than 0.03%, and can be reduced by careful donor selection even if it cannot be excluded altogether.
Most published studies about tumors in donor livers focus on those identified after transplantation that were due to metastases misinterpreted prior to donation as a brain hemorrhage or stroke. These reports include cases of transmission of colon cancer, pancreatic cancer, melanoma and choriocarcinoma, and they all have poor results including death and a need for retransplantation. If the donor has a known history of cancer, the risk depends on the type of tumor, the treatment received, and the amount of time that has passed between diagnosis and the time of organ donation. Nevertheless, for the vast majority of transplant teams, a history of a tumor in a donor contraindicates the donation. The exception to this rule is tumors of the central nervous system (CNS) where the blood-brain barrier has not been altered as occurs in patients who have had cerebrospinal fluid shunts, craniotomies, systemic chemotherapy and radiation therapy. In these circumstances, transplantation of a donated organ increases the likelihood of extra-cranial metastases. When CNS tumors classified as grade III or IV by the World Health Organization (WHO), the transmission rate increases 10%. However, not all studies have replicated these results. A subset of these donors could be a valuable source of organs when a transplant is needed urgently provided the risks and benefits are evaluated very judiciously. An important recommendation for the surgeon harvesting the organ is that a complete examination of the thoracic and abdominal cavities should be made to search for hidden cancer. An autopsy should be considered for those donors with a history of cancer (24-26).
Other findings such as focal nodular hyperplasia, bile duct microhamartomas (Von Meyenburg complexes), and inactive granulomas are found incidentally as small, white, firm subcapsular lesions. Whether only a single cell is found or many cells are found, they contraindicate transplantation. Pathologists sometimes mistake nodular hyperplasia for cirrhosis especially if the pathologist does not know the macroscopic appearance of the tumor that the surgeon has observed. Multiple microhamartomas and granulomas suggest that it has metastasized (2).
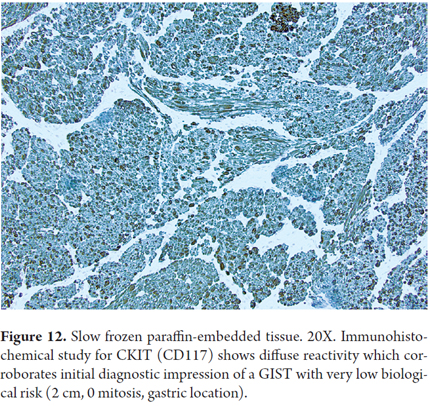
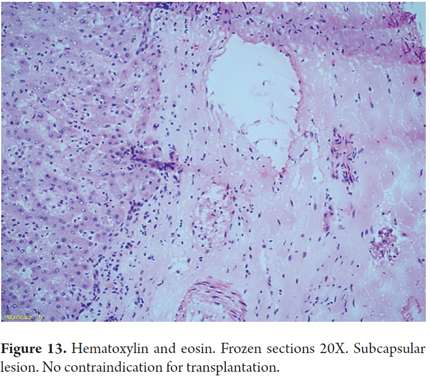
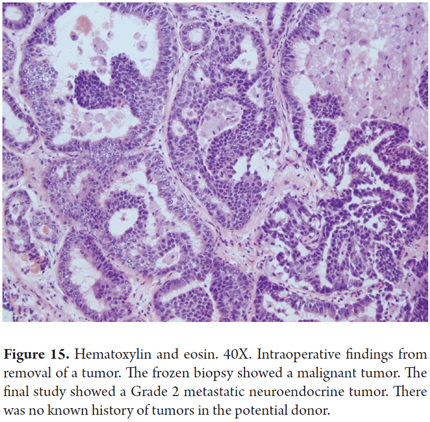
The role of the pathologist in the intraoperative study is especially useful when a liver mass or other body is found during salvage surgery. The pathologist can identify benign lesions, scarring and old inactive granulomas which are considered to be without risk to determine whether or not transplantation is contraindicated (Figures 11, 12 and 13). Hematopoietic neoplasms can be very difficult to diagnose in frozen biopsies, so any doubt of malignancy by the pathologist should be considered a contraindication for donation. The use of donors with primary malignant tumors or tumors that have metastasized is not recommended (Figures 14 and 15 and Table 2) (26).
Pigment Deposits
Liposfuscin is a fine pigment located in the pericentral area (zone 3) that is usually associated with aging. It does not have adverse implications.
Iron is a brown pigment that can look like either fine or coarse coffee grounds. If it is located in Kupffer cells, it is called secondary siderosis which is common following transfusions and which is not a contraindication to donation. Other conditions that cause iron deposits are alcohol, hepatitis B, and hepatitis C. When it is associated with hepatitis, siderosis is a dark brown pigment in the periportal area. In iron overload occurring in hereditary hemochromatosis, the pigment is severe and has a dense portal-central or panlobular gradient. It can even be located in endothelial cells and bile ducts. When it is mild, it can only be detected by Prussian blue staining and definitive paraffin cuts. There is not a lot of data in the literature about what might happen following transplantation since iron is metabolized very quickly and fills up Kupffer cells and portal macrophages. However, susceptibility of the recipient to opportunistic infections has been demonstrated. These can include invasive aspergillosis, cryptococcosis, zygomycosis, bacterial infections such as staphylococcus aureus and cytomegalovirus. Presentation can be fulminant or disseminated and is apparently related to iron overload disease or abnormal iron homeostasis. For these reasons it is recommended that only organs with mild to moderate siderosis be accepted and that organs with hemochromatosis be rejected (2, 27, 28).
Bile can be confused with liposfuscin or iron when it is located in a perivenular area. If it is accompanied by canalicular bile formations, rosette-like hepatocellular structures can help differentiate among these pigments.
CONCLUSIONS
Finding the right balance between an effective clinical evaluation and an objective clinical evaluation of the variables and risk factors related to a donor organ requires, at the minimum, an elevation of age, cold ischemia time, steatosis, and rational use of the donor organ. This must include specific information from an intraoperative biopsy for histological evaluation of the liver of the potential donor which can rapidly provide the transplant team with appropriate and useful information with high predictive value. This information should be reflected in better results for the transplant recipient and perhaps even lower costs for the patient and for the health system.
REFERENCES
1. Naini BV, Lassman CR. Liver Transplant Pathology. Surgical Pathology Clinics. 2013;6(2):277-93. [ Links ]
2. Melin C, Miick R, Young NA, Ortiz J, Balasubramanian M. Approach to intraoperative consultation for donor liver biopsies. Arch Pathol Lab Med. 2013;137(2):270-4. [ Links ]
3. Durand F, Renz JF, Alkofer B, Burra P, Clavien P-A, Porte RJ, et al. Report of the Paris consensus meeting on expanded criteria donors in liver transplantation. Liver Transpl. 2008;14(12):1694-707. [ Links ]
4. Fiorentino M, Vasuri F, Ravaioli M, et al. Predictive value of frozen-section analysis in the histological assessment of steatosis before liver transplantation.Liver Transpl. 2009;15(12):1821-5. [ Links ]
5. Rey JW, Wirges U, Dienes HP, Fries JW. Hepatic steatosis in organ donors: disparity between surgery and histology? Transplant Proc. 2009;41(6):2557-60. [ Links ]
6. Frankel WL, Tranovich JG, Salter L, Bumgardner G, Baker P. The optimal number of donor biopsy sites to evaluate liver histology for transplantation. Liver Transpl. 2002;8(11):1044-50. [ Links ]
7. D'Alessandro E, Calabrese F, Gringeri E, Valente M. Frozen-section diagnosis in donor livers: error rate estimation of steatosis degree. Transplant Proc. 2010;42(6):2226-8. [ Links ]
8. Heller B, Peters S. Assessment of liver transplant donor biopsies for steatosis using frozen section: accuracy and possible impact on transplantation. J Clin Med Res. 2011;3(4):191-4. [ Links ]
9. Marsman H, Matsushita T, Dierkhising R, Kremers W, Rosen C, Burgart L, et al. Assessment of donor liver steatosis: pathologist or automated software? Hum Pathol. 2004;35(4):430-5. [ Links ]
10. Spitzer AL, Lao OB, Dick AAS, Bakthavatsalam R, Halldorson JB, Yeh MM, et al. The biopsied donor liver: incorporating macrosteatosis into high-risk donor assessment. Liver Transpl. 2010;16(7):874-84. [ Links ]
11. Kokudo T, Hasegawa K, Uldry E, Matsuyama Y, Kaneko J, Akamatsu N, et al. A new formula for calculating standard liver volume for living donor liver transplantation without using body weight. J Hepatol. 2015;63(4):848-54. [ Links ]
12. Nobel YR, Forde KA, Wood L, Cartiera K, Munoz-Abraham AS, Yoo PS, et al. Racial and ethnic disparities in access to and utilization of living donor liver transplants. Liver Transpl. 2015;21(7):904-13. [ Links ]
13. Ravaioli M, Grazi GL, Cescon M, Cucchetti A, Ercolani G, Fiorentino M, et al. Liver transplantations with donors aged 60 years and above: the low liver damage strategy. Transpl Int. 2009;22(4):423-33. [ Links ]
14. Busuttil RW, Tanaka K. The utility of marginal donors in liver transplantation. Liver Transpl. 2003;9(7):651-63. [ Links ]
15. Taub R. Liver regeneration: from myth to mechanism. Nat Rev Mol Cell Biol. 2004;5(10):836-47. [ Links ]
16. Chu MJJ, Dare AJ, Phillips ARJ, Bartlett ASJR. Donor Hepatic Steatosis and Outcome After Liver Transplantation: a Systematic Review. J Gastrointest Surg. 2015;19(9):1713-24. [ Links ]
17. Adani GL, Baccarani U, Sainz-Barriga M, Lorenzin D, Bresadola V, Risaliti A, et al. The role of hepatic biopsy to detect macrovacuolar steatosis during liver procurement. Transplant Proc. 2006;38(5):1404-6. [ Links ]
18. Crowley H, Lewis WD, Gordon F, Jenkins R, Khettry U. Steatosis in donor and transplant liver biopsies. Hum Pathol. 2000;31(10):1209-13. [ Links ]
19. Doyle MBM, Vachharajani N, Wellen JR, Anderson CD, Lowell JA, Shenoy S, et al. Short- and long-term outcomes after steatotic liver transplantation. Arch Surg. 2010;145(7):653-60. [ Links ]
20. Velidedeoglu E, Desai NM, Campos L, Olthoff KM, Shaked A, Nunes F, et al. The outcome of liver grafts procured from hepatitis C-positive donors. Transplantation. 2002;73(4):582-7. [ Links ]
21. Cerutti E, Stratta C, Romagnoli R, Serra R, Lepore M, Fop F, et al. Bacterial- and fungal-positive cultures in organ donors: clinical impact in liver transplantation. Liver Transpl. 2006;12(8):1253-9. [ Links ]
22. Lumbreras C, Sanz F, González A, Pérez G, Ramos MJ, Aguado JM, et al. Clinical significance of donor-unrecognized bacteremia in the outcome of solid-organ transplant recipients. Clin Infect Dis. 2001;33(5):722-6. [ Links ]
23. Abraham S, Furth EE. Quantitative evaluation of histological features in «time-zero» liver allograft biopsies as predictors of rejection or graft failure: receiver-operating characteristic analysis application. Hum Pathol. 1996;27(10):1077-84. [ Links ]
24. Detry O. Liver graft procurement in donors with central nervous system cancers. Liver Transpl. 2010;16(7):914-5. [ Links ]
25. Desai R, Neuberger J. Donor transmitted and de novo cancer after liver transplantation. World J Gastroenterol. 2014;20(20):6170-9. [ Links ]
26. Nalesnik MA, Woodle ES, Dimaio JM, Vasudev B, Teperman LW, Covington S, et al. Donor-transmitted malignancies in organ transplantation: assessment of clinical risk. Am J Transplant. 2011;11(6):1140-7. [ Links ]
27. Singh N, Sun H-Y. Iron overload and unique susceptibility of liver transplant recipients to disseminated disease due to opportunistic pathogens. Liver Transpl. 2008;14(9):1249-55. [ Links ]
28. Singh N, Wannstedt C, Keyes L, Mayher D, Tickerhoof L, Akoad M, et al. Hepatic iron content and the risk of Staphylococcus aureus bacteremia in liver transplant recipients. Prog Transplant. 2007;17(4):332-6. [ Links ]











 text in
text in