Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.1 Bogotá jan./mar. 2016
Hirschsprungs Disease in an Adult Patient
Ramón Estopiñan Rebollar MD (1), Ramón Estopiñan Cánovas MD (1), Rafael Pila Peláez MD (1)
(1) Manuel Ascunse Domenech Provincial Clinical and Surgical Hospital in Camagüey, Cuba.
Received: 09-12-14 Accepted: 26-01-16
Abstract
Objective: This study presents a rare case of Hirschsprungs disease in an adult. Case Report: The patient was a 32 year old man with severe intellectual and mental retardation from a poorly educated family. Since childhood, he had had a history of episodes of constipation which was relieved with laxatives and for which he had been admitted on many occasions to the Childrens Hospital of his province. Hirschsprungs disease was diagnosed with a barium enema and rectal manometry. Surgery was recommended, but his family did not give their permission. When he arrived at the hospital, he told doctors that he had not had a bowel movement for 83 days. Physical examination showed a globular, asymmetrical abdomen with a 30x 15cm palpable tumor in the right abdomen. Digital rectal examination showed normal sphincter muscle tone and an empty rectal ampulla. Bowel sounds were minimal. The analytical study was normal. Standing and prone abdominal radiography showed x-ray opacity compatible with fecal matter. Hartmanns procedure was performed to resolve the acute situation. Surgery revealed aganglionic megacolon which was confirmed by histopathology. The patient was asymptomatic while awaiting definitive surgical treatment. Conclusions: Hirschsprungs disease is rare in adults, and must be distinguished from other causes of megacolon. Its etiology is unknown, although it is considered multifactorial. The first and most important symptom is constipation. Diagnosis requires imaging and rectal manometry and confirmation by histopathology. Treatment is always surgical.
Keyword
Adult Hirschsprungs disease.
INTRODUCTION
Hirschsprungs disease (HD) was first described by Harald Hirschsprung, a pediatrician in Copenhagen, Denmark in 1888. He described two cases in two infants. Although rare, it occurs in only one of every 5,000 births, it is one of the most common causes of intestinal obstruction in newborns. (1)
HD is also often called congenital aganglionic megacolon. It is considered to be one of the disorders known as dysganglionoses along with adult hypogaganglionosis and intestinal neuronal dysplasia. (1)
It has been described as a congenital absence of ganglions in the part of the plexus of the enteric nervous system which determines the affected segment. (2) It is a relatively common genetic disorder, but because its transmission is complex, Mendelism is not always apparent. Currently, there are pathogenic bases and genetic aspects of the disease, including descriptions of the involvement of about 13 genes in morphogenesis and differentiation of the enteric nervous system. (3) So far the most important mutations identified occur in the RET proto-oncogene which encodes a receptor tyrosine kinase. It is located on the long arm of chromosome 10. These mutations have been detected in up to 50% of familial cases of HD and in up to 20% of sporadic cases. They are most closely related to long segment disorders. (3)
CASE REPORT
The patient was a 32 year old man with severe intellectual and mental retardation. The patients family consisted of agricultural workers with low educational levels from the province of Las Tunas. Since childhood, the patient had suffered from episodes of constipation that had been treated with laxatives. He had been admitted to the Childrens Hospital of Las Tunas on numerous occasions because of constipation that did not respond positively to the use of laxatives or bulking enemas. A barium enema and rectal colon manometry were used to diagnose Hirschsprungs disease, but relatives opposed surgery to treat the condition. On this occasion, he came to the emergency room of the hospital after 83 days without a bowel movement accompanied by diffuse abdominal pain, cramping and a serious constitutional syndrome.
A complete and local physical examination and laboratory tests had normal results except for moderate malnutrition. The patients blood pressure was 110/70 mmHg and his central heart rate was 112 beats per minute. His abdomen was distended and asymmetrical following respiratory movements. Bowel sounds were minimal,. The patient had a diffuse pain upon palpation of a 30cm long, 15cm wide tumor on the right side of the abdomen. It had smooth, regular edges and soft a surface. There was an abundant and visible venous network. Digital rectal examination showed tonic contraction of the sphincter and an empty rectal vault. The tumor was not palpated and there was no pain during the examination. Blood tests were normal for blood chemistry, enzymes, ions, renal function and pancreatic function. Chest x-rays were taken of both hemidiaphragms. An ECG showed sinus tachycardia. Plain abdominal anteroposterior and lateral x-rays were taken with the patient standing and lying. They showed a soft abdomen, radiopacity that gave the impression of fecal material with dilated bowel loops toward the hypochondrium and the right flank.
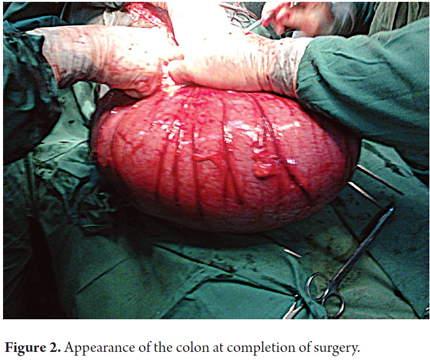
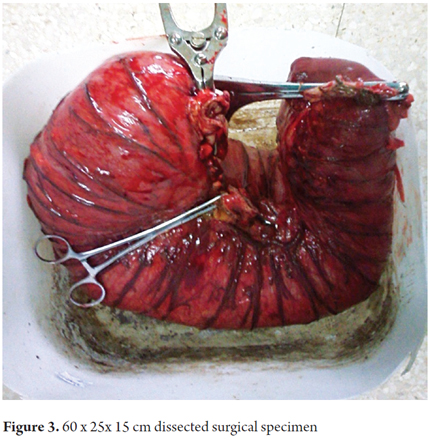
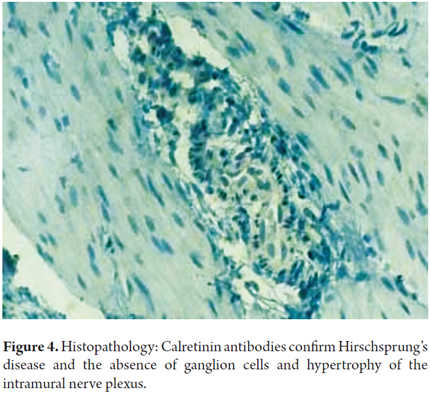
Surgery had been recommended because of the diagnosis of HD, but the patients family had opposed the procedure. At this point, an emergency Hartman sigmoid colostomy was performed (Figures 1 and 2) in order to resolve the acute distention of the colon due to stool which occupied the upper third of the rectum. An area of stenosis that prevented the passage of fecal content was found. The surgical specimen was analyzed by histopathology. It was a 60 x 25 x 15 cm overly distended intestinal segment which was entirely filled with compacted stool which had caused severe bloating. The folds of the intestinal walls had been completely effaced (Figure 3). The histological diagnosis was compatible with aganglionic megacolon. (Figures 4)
The patient is currently undergoing continued treatment as an outpatient in the coloproctology department. He is asymptomatic at this time.
DISCUSSION
The lower limit of aganglionosis, the internal anal sphincter, is constant, but the upper limit is variable and serves to classify the disease. The most common form is HD which is short segment aganglionosis in which the condition does not extend beyond the sigmoid colon. This accounts for 80% of cases. A small number of these cases have ultrashort segments which occupy only the distal rectum below the floor of the pelvis. In long segment aganglionosis, the condition is proximal to the sigmoid colon. This condition accounts for 20% of cases. Among a minority of these patients, the condition affects the entire colon (Colonic HD) or the entire intestine (HD). (4) the case reported here was short segment HD. This occurs in isolation in 70% of cases. In 30% it appears together with other congenital abnormalities. (2) In 12% of the cases, there is a chromosomal abnormality, usually Down syndrome. The other 18% have syndromic alterations or other isolated alterations. (2) In the case we treated, the patient was mentally retarded and had not been treated because of family opposition.
Although the etiology of HD is not known, it is considered to be multifactorial. (1) Symptoms vary according to age, the extent of the area affected, and the presence of complications. The length of the affected segment is not related to age of onset or severity of symptoms. (3) The main symptom is early onset constipation in full term infants. (3) Newborns and small infants almost always have clinical bowel obstruction. (3) Intermittent constipation occurs in 66% of patients beginning in the neonatal period. Abdominal distension and vomiting may occur. If constipation does not have a mechanical cause such as intestinal atresia, meconium ileus, malrotation or imperforate anus, the attending physician should suspect HD. (5)
It was suspected in this patient because of the severe abdominal distension, visible venous network, bloating, anorexia, vomiting, and stunted growth. (4)
Diagnosis of this case in adulthood is probably due to previously undetected congenital causes (5%) or misdiagnosis. Patients with chronic constipation are usually diagnosed after complications such as intestinal volvulus. (3, 4) The simple and proven technique of anteroposterior and lateral x-rays can support the diagnosis when there is an aganglionic segment. This is found in the rectum or sigmoid colon in 80% to 85% of cases. (6). Most authors, (5) but not all, (6) suggest that, prior to corrective surgery, certainty of a positive diagnosis should be established with a biopsy of the rectal wall. This has sensitivity and specificity of close to 100%. (6) Histologically HD is characterized by the absence of parasympathetic ganglion cells and is accompanied by hypertrophy of nerve trunks in 69% of the cases. (7) These were both observed in this patient.
With the advent of immunohistochemistry and histopathological diagnoses, various antibodies have been proposed for identification of certainty ganglion cells. The marker that has proven to be most useful are antibodies to calretinin which has sensitivity and specificity of 100%, (6, 7) but this test is not available in our environment. A barium enema provides more information than plain radiography especially in non-acute patients. Although its sensitivity (70%) and specificity (83%) are lower than those of other diagnostic tests, it is usually the first test conducted. (7)
Rectal manometry, which was used to diagnose this patient, has high sensitivity (91%) and specificity (94%) and is very useful in cases of ultrashort aganglionic segments. (2) Nevertheless, diagnostic certainty requires histological study. The gold standard of diagnosis is a standard surgical biopsy including the muscle layer which has both sensitivity and specificity of 100%. The biopsy sample is usually taken by suction which reduces complications such as infections, bleeding, and perforations and avoids the need for general anesthesia and sutures. (6)
Diagnoses which must be considered in cases of megacolon in adults include HD, intestinal neuronal dysplasia, acquired megacolon, Chagas disease secondary to constipation, chronic intestinal pseudo-obstruction, toxic megacolon due to an infection, and inflammation. (3, 5)
Once the diagnosis has been confirmed, treatment is always surgical. (8) Surgical resection of the affected segment achieves favorable results in the improvement of patients. (8) After the emergency Hartman sigmoid colostomy, our department is currently preparing for definitive treatment of our patient.
CONCLUSIONS
Adult HD or aganglionic megacolon is an intestinal disorder that results from congenital aganglionosis of the colon that is normally diagnosed in childhood. It eventually produces functional intestinal occlusion. Diagnosis in adults is rare, but this condition can cause multiple complications and result in misdiagnosis if a patients family and medical history are not taken into account.
Conflict of interests
The authors have no potential conflicts of interest related to this study.
REFERENCES
1. Menchaca Cervantes C, Rodriguez Velazco A, Ramón García G, Rendom Macías ME. Enfermedad de Hirschsprung. La inmunohistoquímica como apoyo para el diagnóstico. Rev Med Inst Mex Seguro SOE. 2013;51(6):610- 3. [ Links ]
2. Hart J, Wilcox R, Weber C. The gastrointestinal tract. Ed: Stockes JT, Dehner LP, editors. Pediatric pathology. Third edition. USA: wolters kluwer/Lippincott Williams and wilkins; 2011 p 592- 96. [ Links ]
3. Yuksel I, Ataseven I, Ertugrul L, Basar O, Sasmaz N. Adult segmental Hirschprung´s disease. South Med J. 2009;102:184- 5. [ Links ]
4. Fortea C, Martinez D, Rivadulla I, Daroca J, Paira Gitol. Hirschsprung´s disease in adults. Rev Esp Enferm Dig. 2001;3:150-151. [ Links ]
5. Haricharan RN, Georgeson KE. Hirschsprung´s disease. Senein Pediatr Surg. 2008;17:266-75. [ Links ]
6. Kapur RP, Reed RC, Tinn LS, Patterson K, Joanson J, Rothedge JC. Calretinin inmunohistochemestry in the evaluation of suction rectal biopsies for Hirschsprung´s disease. Pediatr Dev Pathol. 2009;12(1):6-15. [ Links ]
7. Memarzadeh M, Talebi A, Edalaty M, Hosseinpoor M, Vattidi N. Hirschsprung´s disease diagnosis: Comparison of inmunohistochimical, hematoxilin and eosin staining. J Indian Assoc Pediatr Surg. 2009;14(2):59-62. [ Links ]
8. Dasgupta R, Langer J. Evaluation and management of persistent problems after surgery for Hirschsprung´s disease in a child. J Pediatr Gastrointernal. 2008;46:13-19. [ Links ]











 texto em
texto em