Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.2 Bogotá Apr./June 2016
Risk Factors Associated with Nonalcoholic Fatty Liver Disease in a Colombian Caribbean Population
Lina Lambis A. (1), José Belisario Solana T. MD (2), Bertha Gastelbondo P. (1), Daniel Romero S. (1), Daniela Garrido C. (1), Walter Puello R. MD (3), María C. García E. (1), Amileth Suarez C. (4)
(1) Grupo Prometeus and biomedicine applied to clinical sciences in the Biochemistry Laboratory of the Faculty of Medicine of the University of Cartagena in Cartagena, Colombia.
(2) Physician in the Liver and Biliary Tract Unit of the Hospital Universitario del Caribe in Cartagena, Colombia.
(3) Surgery Resident in the Faculty of Medicine of the University of Cartagena in Cartagena, Colombia.
(4) Director of Grupo Prometeus and biomedicine applied to clinical sciences, Professor of Biochemistry (PhD) in the Faculty of Medicine of the University of Cartagena in Cartagena, Colombia. Mail: asuarezc1@unicartagena.edu.co
Received: 28-05-15 Accepted: 18-04-16
Abstract
Nonalcoholic fatty liver disease (NAFLD) is a health problem that has been demonstrated by research from everywhere around the world where the disease's prevalence appears to be high. The aim of this pilot study was to describe the relationship of risk factors associated with NAFLD in terms of demographic, epidemiological and biochemical variables. Patients included in the study were drawn from people who came to the liver and biliary tract section of the Hospital Universitario del Caribe in Cartagena, Colombia. This was a prospective and descriptive pilot study that reviewed medical records for analysis of epidemiological and demographic variables. It assessed spectrophotometric measurement of transaminases for determination of De Ritis ratios (AST/ALT), and relationship to levels of cholesterol and triglycerides. The results suggest that risks of developing NAFLD were higher among women, among patients who were obese, among patients who had diabetes mellitus, among patients who had hypertension and obesity, and among patients who had diabetes combined with obesity. Patients at risk merit biochemical molecular study and a definitive diagnosis.
Keywords
Fatty liver, NAFLD, gastroenterology.
INTRODUCTION
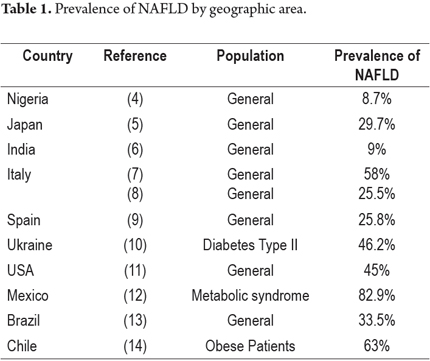
Nonalcoholic fatty liver disease (NAFLD), also known as hepatic steatosis, is a clinicopathological condition characterized by infiltration of fat in hepatocytes of the liver parenchyma at a rate that exceeds 5% to 10% of its weight. Patients have persistently abnormal levels of liver enzymes but do not consume significant amounts of alcohol. It is also considered to be the hepatic manifestation of metabolic syndrome. (1, 2) The prevalence of NAFLD is related to insulin resistance and obesity and varies from country to country (Table 1). Nevertheless, the ranges is estimated to be between 20% and 30% worldwide especially in industrialized Western countries. (3)
Clinically, NAFLD has a broad spectrum of presentations from simple macrovesicular steatosis, to fatty liver accompanied by inflammation, on to fibrogenesis and hepatocellular necrosis . The latter increases the risk of liver failure and in some cases leads to the development of hepatocellular carcinoma. (15-20) Among the risk factors associated with NAFLD are lifestyle factors such as diet and exercise, insulin resistance, type II diabetes, dyslipidemia, age, gender and genetic factors. (21) It is worth noting that obesity and insulin resistance are considered risk to be the factors most frequently associated with NAFLD and that the degree of steatosis can be correlated with body mass index (BMI). Diabetes may be an independent predictor of NAFLD and of liver damage.
NAFLD's complex biochemical mechanism involves accumulation of triglycerides, insulin resistance, dysregulation of lipid metabolism, oxidative stress, lipid peroxidation, mitochondrial dysfunction, and innate immune response dysfunction. (22, 23) Genetics can be a determinant of risk and severity the development NAFLD since these processes are associated with multiple polymorphisms. (24) Biochemical tests for diagnosis include those for transaminases, triglycerides and cholesterol which are sensitive tests for simple steatosis, but confirmation requires histological images or imaging including ultrasound, computed tomography, MRI and Fibroscan (transient elastography).
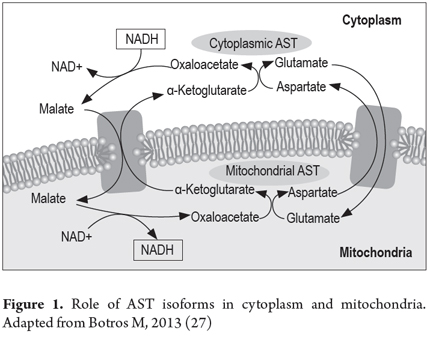
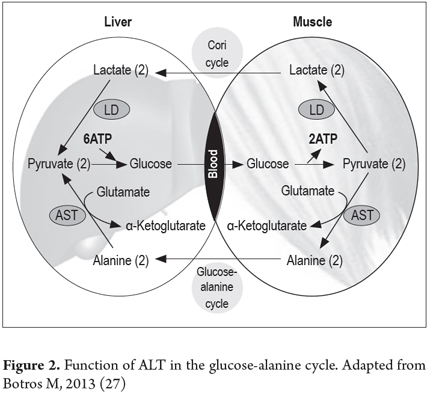
One parameter, AST/ALT (aspartate aminotransferase/alanine aminotransferase) whose usefulness was demonstrated in 1957 by Fernando De Ritis, (25) has been almost forgotten, but it predicts hepatocellular damage. ALT is present only in the cytoplasm, while AST has two isoforms, cytoplasmic (CAST) and mitochondrial (MAST). These are immunologically distinct, the isoenzyme is much more prevalent in mitochondria and MAST accounts for about 80% of total activity in the human liver. (26) The activity of these transaminases reflects the metabolic activity in the tissues where they are expressed and represents the important relationship between carbohydrate metabolism and proteins (Figures 1 and 2). The AST/ALT (De Ritis ratio) ratio is a useful supporting indicator for predicting the likeliness of that liver damage will develop into cirrhosis. This is because when serum levels of hepatocellular death increase, levels of AST increase more than levels of ALT. Consequently, whenever AST ratio is much higher than ALT it reflects cellular damage. When the relationship is more than two to one it indicates intracellular enzyme release (both MAST and CAST) and thus indicates hepatocellular damage.
The objective of this first part of the pilot study was to assess the relationship of demographic, epidemiological and biochemical factors to risk factors associated with the development of NAFLD among patients who came to the liver and biliary tract section of the Hospital Universitario del Caribe in Cartagena.
METHODOLOGY
This prospective descriptive pilot study included 105 adult patients with risk factors associated with NAFLD who were seen in liver and bile duct surgery unit at the Hospital Universitario del Caribe from September 2014 to April 2015. The study's exclusion criteria were alcohol consumption of 20 g/day for men and 10 g/day for women, viral hepatitis, hepatotoxic drugs, hemochromatosis and Wilson's disease. Demographic characteristics, reason for patient referral patient, medical history, physical examination data and laboratory test results were all recorded. Descriptive statistics including measures of central tendency, percentages and absolute frequencies were calculated with a 5% margin of error. Graphpad Prism was used for data analysis. All data in this study were collected and used in accordance with the principles stated in the Eighteenth World Medical Assembly (Helsinki, 1964).
Biochemical Analysis
Blood samples obtained by venipuncture were collected into tubes containing ethylenediaminetetraacetic acid (used as an anticoagulant). Plasma was obtained by centrifuging samples for 10 minutes at 2500 rpm at 4 ° C. Tests were conducted at the Biochemistry Research Laboratory of the Faculty of Medicine. Determination of enzymatic activity of transaminases, triglycerides and cholesterol was performed according to manufacturer (Biosystems). The reference values established for evaluating enzyme activity of AST and ALT, cholesterol and triglycerides were 40 U/L, 41 U/L, 200 mg/dL, 150 mg/dL respectively. Enzyme activity (U) was defined as the concentration of enzyme which catalyzes the conversion of 1 µmol of substrate in one minute. All determinations were performed in triplicate in Tecan infinite M200®.
RESULTS
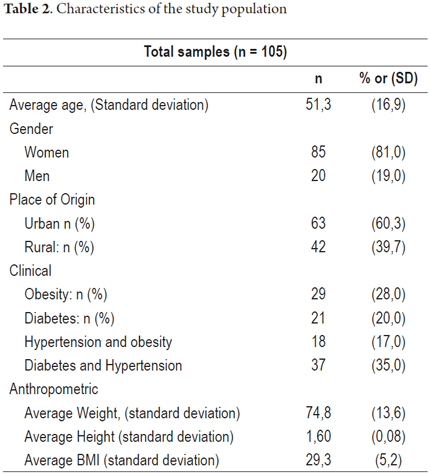
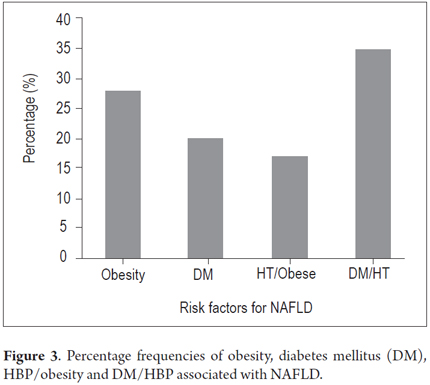
This study is based on the medical records of 105 patients seen in the liver and biliary tract unit of the Hospital Universitario del Caribe. They were used for descriptive analysis of risk factors for NAFLD, corresponding to patients admitted to the Unit of Caribbean University Hospital. The age range of the patients included in the study were young (18-23 years), adults (24-59 years) and elderly (over 60 years). Preliminary results show that the majority of this population (52%) consists of adults. Nevertheless, it is worrying that 18% of the study are young people and Of the study population, 85% were women and 82% live in urban areas (Table 2). Risk factors associated with NAFLD included type II diabetes mellitus (28%), obesity (20%) and HBP (38%). Absolute values were taken without accounting for overlapping pathologies. Figure 3 shows the percentages and groups associated with combinations of two diseases. The distribution is as follows: 28% obese; 20% DM; 17% HBP and obesity; and 35% DM and HBP.
Biochemical markers
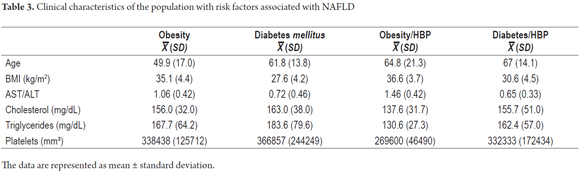
The De Ritis ratio (AST/ALT) was significantly greater than 1.0 (p <0.05), triglycerides were above 160 mg/dL and cholesterol was less than 200 mg/dL. As shown in Table 3, in the study sample of patients those who were characterized as both being obese and having high blood pressure had the highest De Ritis ratios and an average BMI of 36.6.
DISCUSSION
NAFLD is a major public health problem which has been extensively studied worldwide. Its incidence has been estimated at one in three adults in developed countries, and it can affect individuals at any age. NAFLD was found to have 46% prevelance in a prospective cohort study that used ultrasound (US) and liver biopsies of asymptomatic adult patients. (28, 29) Ethnicity also influences NAFLD's prevalence. (30) Accordingly, the population of South America has the greatest number of individuals recorded with this disease of any place worldwide. (31, 32) According to our results, the main risk factors associated with NAFLD in the population studied are obesity, DM, HBP, De Ritis ratio > 1.0 index and dyslipidemia. This accords well with data presented in clinical practice guidelines for NAFLD (Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis) and warrants a comprehensive biochemical-molecular study that includes diagnosis of NAFLD in order to improve our understanding of this disease. (33)
While a linear relationship among age, frequency of associated factors and confirmation of cases of NAFLD has been reported, this was not found in our study. Two possible reasons could be early death from liver disease and low level of health care coverage of this population. Moreover, the fact that 18% of the patients in this study with NAFLD were young individuals is a disturbing fact because of the likely long/term impact on the pathology considering that the livers of these patients will be exposed for long periods of time to metabolic changes which ultimately can cause increased risk of progression and complications.
The results show the highest frequency of this disease among women who live in urban areas, which is similar to data reported by other studies in Colombia. (34) These findings could be associated with high levels of stress, decreased quality of life and inadequate eating habits. These factors also need to be evaluated as possible explanations of the high levels of cardiovascular risks of women in the same region. (35) In addition, to observe these characteristics associated with NAFLD mostly in urban areas is an indirect indication of a liver disorder that has always been linked to stress and to developed countries, rather than to geographical location. This is due to lifestyle and diet of the population. (1) The study population was characterized by diseases such as diabetes mellitus, obesity, hypertension and combinations of these. Other researchers have reported diseases associated with NAFLD and these have been included in this pilot study. (2)
The relative frequency of these pathologies associated with NAFLD was similar for all groups, but obesity had the highest incidence. This factor is one of the most influential. A fact that is highlighted by a report from Japan which found a prevalence of obesity approximately 25% in patients with NAFLD. (15) Obviously, this varies in different regions and according to culture and lifestyles. Still, other researchers believe that not all obese people develop NAFLD, but highlight the importance of the presence of additional factors such as diabetes. (18) For Latin America, it is worth noting that the World Health Organization reported that more than 15% of the populations of Argentina, Colombia, Peru, Paraguay and Uruguay are obese. Other studies have also highlighted that Latin America is more susceptible to obesity and type II diabetes because of the tendency to a sedentary lifestyle combined with consumption of foods that are high in fat. (17) It should also be noted that obesity is correlated with the prevalence and severity of NAFLD as has been demonstrated by recent American studies in which the prevalence of obesity combined with severe NAFLD was 23.5% among men and 29.7% among women. (16)
Another risk factor related to the development of chronic liver disease is diabetes mellitus. The prevalence of NAFLD is between 60% and 76% among patients with this condition. This highlights the study population NAFLD because insulin resistance and oxidative stress play an important role in the development and progression of NAFLD because high concentrations of insulin can cause failure to suppress the flow of fatty acids. All these factors associated with NAFLD confirm the strict pathophysiological association between imbalances of lipid metabolism and biochemically established glucose. (19, 21)
In our study 20% of the population with high risks of NAFLD had DM. It is indubitable that metabolic imbalances of lipids and carbohydrates have a strong influence on development of NAFLD which makes it necessary to confirm this diagnosis. Our results showed that the various groups did not have significantly high scores for liver fibrosis (data not shown). This finding is consistent with the levels of triglycerides and cholesterol. Triglycerides are considered to be hepatoprotective in the context of NAFLD. They protect against lipotoxicity by providing a buffering mechanism for the accumulation of free fatty acids, but this is not harmless since steatosis has been associated with obesity, dyslipidemia, insulin resistance and hypertension. Unlike triglycerides, cholesterol is associated with NASH. An in-vitro study in Caenorhabditis elegans showed that free cholesterol, more than the accumulation of triglycerides and free fatty acids, sensitizes the liver to steatosis through tumor necrosis factor alpha (TNF-α) and Fas. There is also evidence from mouse models of hyperlipidemia in which free cholesterol is a major risk factor for the transition from steatosis to NASH. (36-40)
Finally, De Ritis ratios greater than 1.0 indicate progression of liver fibrosis. These ratios probably derived from the production and release of mitochondrial AST. (24) It has been suggested that these changes in transaminase levels precede NAFLD and tend to be associated with insulin resistance. (4) While De Ritis ratios greater than 1.0 may indicate the development of cirrhosis, elevated transaminase levels in NAFLD is not always evidence of the degree of a hepatocellular condition. (5) Therefore, it is important that biochemical results be followed up with a comprehensive study of NAFLD through imaging, histology and biochemical and molecular markers to elucidate the molecular mechanisms underlying NAFLD and provide new bases for the treatment of liver inflammation.
CONCLUSION
In summary, the preliminary results of this pilot study suggest that there is a population with factors that put them at high risk of developing NAFLD. Risk factors include demographic characteristics, AST/ALT greater than 1.0 and other biochemical variables. This highlights the need for a more comprehensive biochemical-molecular study.
Acknowledgements
We wish to thank the Faculty of Medicine of the University of Cartagena, Hospital Universitario del Caribe, the Semillero de Investigación del Grupo Prometeus, and the Surgery Residents of the University of Cartagena (Dr. Pedro Vides De la Cruz, Dr. Adolfo Roldan Chica, Dr. Luis Gerardo Villota Gonzalez, and Dr. Ruben Agresott Marsiglia).
Conflict of Interests
The authors declare that they have no conflicts of interest.
Funding
The authors declare that this study was partially funded by the Strengthening the Biochemistry Master's Degree program and by autonomous financing from the Prometeus & Biomedicina aplicada a las Ciencias clínicas group which is recognized by Colciencias.
REFERENCES
1. Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology (Baltimore, Md). 2003;37(4):917-23. [ Links ]
2. Adams LA, Waters OR, Knuiman MW, Elliott RR, Olynyk JK. NAFLD as a Risk Factor for the Development of Diabetes and the Metabolic Syndrome: An Eleven-Year Follow-up Study. Am J Gastroenterol. 2009;104(4):861-7. [ Links ]
3. Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol. 2006;40 Suppl 1:S5-10. [ Links ]
4. Onyekwere CA, Ogbera AO, Balogun BO. Non-alcoholic fatty liver disease and the metabolic syndrome in an urban hospital serving an African community. Ann Hepatol. 2011;10(2):119-24. [ Links ]
5. Eguchi Y, Hyogo H, Ono M, Mizuta T, Ono N, Fujimoto K, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol. 2012;47(5):586-95. [ Links ]
6. Amarapurkar D, Kamani P, Patel N, Gupte P, Kumar P, Agal S, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol. 2007;6(3):161-3. [ Links ]
7. Bellentani S, Saccoccio G, Masutti F, Croce LS, Brandi G, Sasso F, et al. Prevalence of and risk factors for hepatic steatosis in Northern Italy. Ann Intern Med. 2000;132(2):112-7. [ Links ]
8. Bellentani S, Bedogni G, Miglioli L, Tiribelli C. The epidemiology of fatty liver. Eur J Gastroenterol Hepatol. 2004;16(11):1087-93. [ Links ]
9. Caballeria L, Pera G, Auladell MA, Toran P, Munoz L, Miranda D, et al. Prevalence and factors associated with the presence of nonalcoholic fatty liver disease in an adult population in Spain. Eur J Gastroenterol Hepatol. 2010;22(1):24-32. [ Links ]
10. Williamson RM, Price JF, Glancy S, Perry E, Nee LD, Hayes PC, et al. Prevalence of and risk factors for hepatic steatosis and nonalcoholic Fatty liver disease in people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes Care. 2011;34(5):1139-44. [ Links ]
11. Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology (Baltimore, Md). 2004;40(6):1387-95. [ Links ]
12. Castro-Martinez MG, Banderas-Lares DZ, Ramirez-Martinez JC, Escobedo-de la Pena J. Prevalence of nonalcoholic fatty liver disease in subjects with metabolic syndrome. Cir Cir. 2012;80(2):128-33. [ Links ]
13. Araujo LM, De Oliveira DA, Nunes DS. Liver and biliary ultrasonography in diabetic and non-diabetic obese women. Diabetes Metab. 1998;24(5):458-62. [ Links ]
14. Boza C, Riquelme A, Ibanez L, Duarte I, Norero E, Viviani P, et al. Predictors of nonalcoholic steatohepatitis (NASH) in obese patients undergoing gastric bypass. Obes Surg. 2005;15(8):1148-53. [ Links ]
15. Chavez-Tapia NC, Sanchez-Avila F, Vasquez-Fernandez F, Torres-Machorro A, Tellez-Avila FI, Uribe M. Non-alcoholic fatty-liver disease in pediatric populations. Journal of pediatric endocrinology & metabolism. JPEM. 2007;20(10):1059-73. [ Links ]
16. Feng RN, Du SS, Wang C, Li YC, Liu LY, Guo FC, et al. Lean-non-alcoholic fatty liver disease increases risk for metabolic disorders in a normal weight Chinese population. World journal of gastroenterology. 2014;20(47):17932-40. [ Links ]
17. Seo HI, Cho YK, Lee WY, Rhee EJ, Sung KC, Kim BS, et al. Which metabolic syndrome criteria best predict the presence of non-alcoholic fatty liver disease? Diabetes Res Clin Pract. 2012;95(1):19-24. [ Links ]
18. Sun L, Lu SZ. Association between non-alcoholic fatty liver disease and coronary artery disease severity. Chin Med J (Engl). 2011;124(6):867-72. [ Links ]
19. De Alwis NM, Day CP. Non-alcoholic fatty liver disease: the mist gradually clears. Journal of hepatology. 2008;48(Suppl 1):S104-12. [ Links ]
20. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet (London, England). 2006;368(9548):1681-8. [ Links ]
21. Otgonsuren M, Stepanova M, Gerber L, Younossi ZM. Anthropometric and clinical factors associated with mortality in subjects with nonalcoholic fatty liver disease. Dig Dis Sci. 2013;58(4):1132-40. [ Links ]
22. Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nature genetics. 2008;40(12):1461-5. [ Links ]
23. Kawaguchi T, Sumida Y, Umemura A, Matsuo K, Takahashi M, Takamura T, et al. Genetic polymorphisms of the human PNPLA3 gene are strongly associated with severity of non-alcoholic fatty liver disease in Japanese. PloS one. 2012;7(6):e38322. [ Links ]
24. Daliri MR. A hybrid automatic system for the diagnosis of lung cancer based on genetic algorithm and fuzzy extreme learning machines. J Med Syst. 2012;36(2):1001-5. [ Links ]
25. Kleine FD. The diagnostic significance of the De-Ritis quotient. Deutsche Zeitschrift fur Verdauungs- und Stoffwechselkrankheiten. 1966;25(6):355-62. [ Links ]
26. Rej R. Aspartate aminotransferase activity and isoenzyme proportions in human liver tissues. Clin Chem. 1978;24(11):1971-9. [ Links ]
27. Botros M, Sikaris KA. The de ritis ratio: the test of time. The Clinical biochemist Reviews / Australian Association of Clinical Biochemists. 2013;34(3):117-30. [ Links ]
28. Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140(1):124-31. [ Links ]
29. Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34(3):274-85. [ Links ]
30. Lonardo A, Bellentani S, Argo CK, Ballestri S, Byrne CD, Caldwell SH, et al. Epidemiological modifiers of non-alcoholic fatty liver disease: Focus on high-risk groups. Digestive and liver disease: official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. 2015. [ Links ]
31. Weston SR, Leyden W, Murphy R, Bass NM, Bell BP, Manos MM, et al. Racial and ethnic distribution of nonalcoholic fatty liver in persons with newly diagnosed chronic liver disease. Hepatology (Baltimore, Md). 2005;41(2):372-9. [ Links ]
32. Caldwell SH, Harris DM, Patrie JT, Hespenheide EE. Is NASH underdiagnosed among African Americans? Am J Gastroenterol. 2002;97(6):1496-500. [ Links ]
33. Watanabe S, Hashimoto E, Ikejima K, Uto H, Ono M, Sumida Y, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. J Gastroenterol. 2015;50(4):364-77. [ Links ]
34. Vanegas R CM, Restrepo R C, Vargas G N, Marín C AE, Martínez S LM, Yepes D CE, et al. Characterization of Patients with Non-Alcoholic fatty Liver Disease in a Highly Complex Colombian Hospital in 2013. Rev Col Gastroenterol. 2014;29(4):342-6. [ Links ]
35. Cabarcas-Barboza O, Pulgar-Emiliani MI, Alvear-Sedan C. Cardiovascular risk factors in young adult people of cartagena de indias. Colombia. Revista Ciencias Biomedicas. 2014;5(2):211-9. [ Links ]
36. Puri P, Baillie RA, Wiest MM, Mirshahi F, Choudhury J, Cheung O, et al. A lipidomic analysis of nonalcoholic fatty liver disease. Hepatology (Baltimore, Md). 2007;46(4):1081-90. [ Links ]
37. Yamaguchi K, Yang L, McCall S, Huang J, Yu XX, Pandey SK, et al. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology (Baltimore, Md). 2007;45(6):1366-74. [ Links ]
38. Asrih M, Jornayvaz FR. Inflammation as a potential link between nonalcoholic fatty liver disease and insulin resistance. The Journal of endocrinology. 2013;218(3):R25-36. [ Links ]
39. Caballero F, Fernandez A, De Lacy AM, Fernandez-Checa JC, Caballeria J, Garcia-Ruiz C. Enhanced free cholesterol, SREBP-2 and StAR expression in human NASH. Journal of hepatology. 2009;50(4):789-96. [ Links ]
40. Walenbergh SM, Shiri-Sverdlov R. Cholesterol is a significant risk factor for non-alcoholic steatohepatitis. Expert review of gastroenterology & hepatology. 2015;9(11):1343-6. [ Links ]











 text in
text in