Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.2 Bogotá Apr./June 2016
Two Case Reports of Allergies to Amino Acid Based Formula in Patients with Short Bowel Syndrome
Mónica Contreras Ramírez MD (1), Catalina Ortiz-Piedrahita MD (1), Lina María Castaño Jaramillo MD (2), Ana Elvira Montero Carvajalino MD (3), Juan Camilo Pérez Cadavid MD (4)
(1) Pediatric gastroenterologist at the Hospital Pablo Tobon Uribe in Medellín, Colombia.
(2) Third year Pediatrics Resident at CES University in Medellín, Colombia.
(3) Pediatrician at the Universidad del Norte in Barranquilla, Colombia.
(4) Pathologist at the Hospital Pablo Tobon Uribe in Medellín, Colombia.
Received: 10-09-15 Accepted: 18-04-16
Abstract
Short bowel syndrome (SBS) is characterized by alterations in the absorption surface and in the functionality of the gastrointestinal system. Patients with SBS are more prone to allergies the protein in cow's milk and eggs. We report two cases of infants with SBS and allergic reactions to amino acid based formulas. In the first case, the patient's response was not IgE-mediated. It manifested clinically with eosinophilic colitis that improved with the use of systemic steroids and a change to another elemental formula. In the second case, the patient initially presented intolerance to breast milk and extensively hydrolyzed formula. After feeding with the first free amino acid formula, the patient developed gastrointestinal bleeding and skin manifestations. Another free amino acid formula was substituted. The patient had transient tolerance to the new formula. Later, in the context of an unspecified viral infection with respiratory and gastrointestinal involvement, the patient presented an anaphylactic reaction to the formula which had previously been tolerated. This necessitated a change to a modular diet which was adequately tolerated. We have presented this case report because no previous reports were found in the literature about allergic reactions to basic amino acid-based formulas. There is still no consensus on the ideal formula for preventing allergic sensitization in patients with SBS.
Keywords
Food allergy, short bowel syndrome, elemental formula, amino acids.
INTRODUCTION
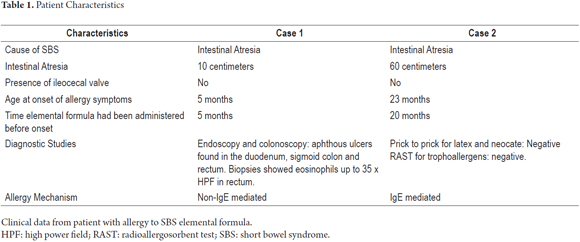
Short bowel syndrome (SBS) is a pathology that occurs secondary to intestinal resection which results in less surface area for absorption of nutrients and hence to metabolic and nutritional disorders. After resection, the a process of adaptation of remaining intestine begins in which multiple gradual structural and functional changes occur. Some studies have reported that this condition can predispose the patient to sensitization to various allergens in the intestinal tract and thus to increased risk of food allergies. (1, 2) We present the cases of two infants with SBS who had allergic reactions during the administration of amino acid based formulas (AABFs, also known as elemental formulas) through enteral feeding. The main characteristics of these patients are presented in Table 1.
PRESENTATION OF CLINICAL CASES
Case 1
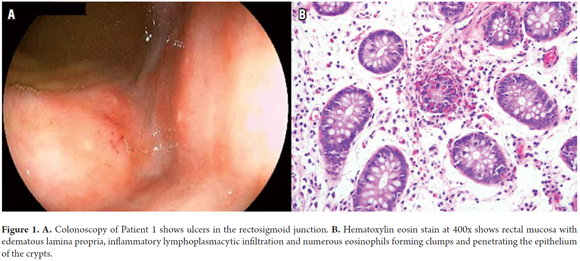
The patient was a six month old girl with intestinal atresia who had been born prematurely. From birth she had been fed with AABF (Puramino® Mead-Johnson and then with Neocate Nutricia). At 5 months, she stopped gaining weight and began having stools containing mucus and blood. A stool culture was negative for infections by rotavirus, adenovirus and parasites. The endoscopy and colonoscopy showed ulcers in the duodenum, sigmoid colon and rectum. At 35 x HPF, biopsies showed inflammatory changes with eosinophils in the rectum but no peripheral eosinophilia were found (Figure 1). The patient's symptoms resolved after allowing her bowel to rest and administering systemic steroids. AABF feeding (Puramino® Mead-Johnson) was subsequently restarted without recurrence of the earlier symptoms.
Case 2
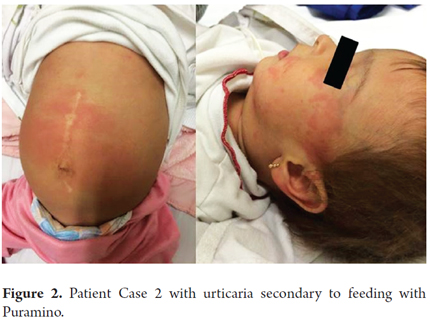
The patient was a 23 month old girl with intestinal atresia who had been born prematurely. In her first month of life, enteral with breast milk had begun. After she developed vomiting and rectal hematochezia, she was switched to and extensively hydrolyzed formula (EHF), Nutramigen® from Mead Johnson, and a maternal exclusion diet was begun. Her diet was subsequently changed to an AABF, (Neocate® from Nutricia, because of persistence of symptomatic evidence of eosinophils in her feces. After tolerating this diet for two months, she developed gastrointestinal symptoms including hematochezia and urticaria. She was switched to another AABF, Puramino® from Mead-Johnson, which she tolerated for 23 months. She returned to the clinic with a viral infection and gastrointestinal and respiratory compromise. She developed an anaphylactic reaction including urticaria, tachycardia, shortness of breath and wheezing after administration of Puramino (Figure 2). This was resolved with a single dose of intramuscular adrenaline. She was placed on an AABF exclusion diet with added modules of maltodextrins, olive oil and Farmal. There have been no recurrence of allergic symptoms.
DISCUSSION
SBS not only affects absorption, it also affects other functions. It leads to loss of lymphoid tissue associated with altered mucosa which facilitates bacterial overgrowth. Intestinal inflammation and increased permeability of the mucosa to dietary antigens have the consequence of allowing sensitization to these allergens. Other factors such as prematurity have also been associated with increased risk of food allergies. (1-3). Here, we have presented two cases of premature infants with SBS secondary to bowel resection for intestinal atresia who developed digestive and skin symptoms of food allergies. This was corroborated by evidence of eosinophil infiltration in one case and improvement after exclusion of amino acid based formula in both cases.
Hydrogen breath tests for diagnosing bacterial overgrowth are not available in our institution, so cycles of intraluminal antibiotics (metronidazole and/or rifaximin) are administered when there is clinical suspicion. This was done for both of these patients, but not concomitant with the appearance of clinical symptoms.
There is no consensus regarding the ideal time to start enteral feeding in patients with short bowel syndrome. Studies in animal models of SBS have reported improved tolerance when AABF are used. (4) Human studies have shown no differences in protein absorption, permeability and intestinal adaptation between EHF and whole protein formulas. (5, 6) However, some authors have proposed that hydrolyzed milk be given to patients under two years old who have SBS due to their increased susceptibility to inflammation of the mucosa that could trigger allergic sensitization and gastrointestinal disease. (7) In our hospital, children with short bowel syndrome are fed with EHF and only patients with signs of intolerance or allergy symptoms are switched to AABF.
Significantly, our two patients had been fed AABF for prolonged periods of time at the onset of symptoms. One patient presented an allergic episode after an acute viral infection. None of the aforementioned articles report the occurrence of food allergies among patients being fed with AABFs. Neither of our patients had any history of previous consumption of cow's milk protein (CMP) that could have given rise to sensitization, and only the second patient had a history of breast milk intake for a short time during the neonatal period.
Some authors suggest that prolonged use of AABF can lead to atrophy of the intestinal mucosa. When under stress, the mucosa increases its permeability and increases the risk of sensitization to food-borne macromolecules. (5) Although the endoscopy of Patient 1 did not document intestinal atrophy, patchy atrophic compromise is a possibility that cannot be excluded. No endoscopic studies were conducted to look for atrophy or intestinal tissue infiltration in Case 2 because the patient improved significantly when AABFs were excluded from her diet. Another possible explanation for her allergic reactions is exposure to traces of different proteins to CMP which may be present in the oil used in the composition of these formulas. (2)
Allergies to egg and to cow's milk protein in children with SBS have been described in the literature. Leechawengwongs and her colleagues reported the case of two patients with SBS who had clinical and paraclinical evidence of allergies to CMP and other allergens. (3). Masumoto describes two infants with ultrashort SBS who were allergic to the initial protein formula produced with whole cow's milk. (2) Mazon et al. reported a series of 14 children with SBS, 57% of whom were intolerant to cow's milk as demonstrated by allergy prick tests and ImmunoCAP® tests for specific immunoglobulin E (IgE). These patients had only been fed with EHF and had no family histories of allergy. (1) Diamanti describes the cases of three patients with SBS, all of whom tested posted for allergies to CMP after it had been introduced to their diets. (8) Patient 2's allergy tests were negative for IgE mediated for trophoallergens and one of the formulas of amino acids which made it difficult to diagnose an allergy. As described by Mazon et al., 43% of patients with food allergy tests had negative tests for IgE. The presentation of these clinical cases leaves open the discussion regarding what kinds of formulas should be used in patients with SBS in order to prevent sensitization to CMP in stress conditions such as those described above.
REFERENCES
1. Mazon A, Solera E, Alentado N, Oliver F, Pamies R, Caballero L, et al. Frequent IgE sensitization to latex, cow's milk, and egg in children with short bowel syndrome. Pediatr Allergy Immunol Off Publ Eur Soc Pediatr Allergy Immunol. 2008 Mar;19(2):180–3. [ Links ]
2. Masumoto K, Esumi G, Teshiba R, Nagata K, Hayashida M, Nakatsuji T, et al. Cow's milk allergy in extremely short bowel syndrome: Report of two infants. Eur E-J Clin Nutr Metab. 2008;3(5):e217-9. [ Links ]
3. Leechawengwongs E, Tison BE, Gopalakrishna GS, Reid BS, Bacino CA, Haws AL, et al. Does short bowel syndrome increase the risk of food allergy and eosinophilic gastrointestinal disease? Observations in Shah-Waardenburg syndrome. J Allergy Clin Immunol. 2013;131(1):251-5. [ Links ]
4. Hua Z, Turner JM, Mager DR, Sigalet DL, Wizzard PR, Nation PN, et al. Effects of polymeric formula vs elemental formula in neonatal piglets with short bowel syndrome. JPEN J Parenter Enteral Nutr. 2014;38(4):498-506. [ Links ]
5. Ksiazyk J, Piena M, Kierkus J, Lyszkowska M. Hydrolyzed versus nonhydrolyzed protein diet in short bowel syndrome in children. J Pediatr Gastroenterol Nutr. 2002;35(5):615-8. [ Links ]
6. Olieman JF, Penning C, Ijsselstijn H, Escher JC, Joosten KF, Hulst JM, et al. Enteral nutrition in children with short-bowel syndrome: current evidence and recommendations for the clinician. J Am Diet Assoc. 2010;110(3):420-6. [ Links ]
7. Vanderhoof JA, Young RJ. Hydrolyzed versus nonhydrolyzed protein diet in short bowel syndrome in children. J Pediatr Gastroenterol Nutr. 2004;38(1):107. [ Links ]
8. Diamanti A, Fiocchi AG, Capriati T, Panetta F, Pucci N, Bellucci F, et al. Cow's milk allergy and neonatal short bowel syndrome: comorbidity or true association? Eur J Clin Nutr. 2015;69(1):102-6. [ Links ]











 text in
text in