Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.3 Bogotá jul./set. 2016
Clinical and Demographic Factors Associated with Survival Following Liver Transplantation in Patients over 14 Years of Age at the Hospital Universitario de San Vicente Fundación from 2002 to 2013
Juan Fernando Londoño U. MD. (1), Yuli Agudelo B. MD (1), Gonzalo Guevara C. MD (1), Doris Cardona A. MD (2)
(1) Hospital Universitario de San Vicente Fundación in Medellín, Colombia.
(2) Universidad CES in Medellín, Colombia.
This research was conducted entirely with the resources of the Hospital Universitario de San Vicente Fundación and Universidad CES.
Received: 19-05-15 Accepted: 25-07-16
Abstract
Terminal liver diseases have high rates of incidence and prevalence throughout the world and result in more than 800,000 deaths annually. (1) The treatment for advanced liver disease is transplantation. Advances in surgical technique, proper selection of donors and recipients and development of immunosuppression have transformed transplantation into the best option for patients with end-stage liver disease. (2)
Counting transplantation of organs of all types, Given all organs, in the Hospital Universitario de San Vicente Fundación (HUSVF) was the leading transplant center in Colombia. (3) This study was conducted to redress the absence of information on transplant patient survival. This is a quantitative study conducted through a cohort follow-up with analysis of survival. All liver transplants performed at the hospital between 2002 and 2013 were included. Data were collected to determine one and five year survival rates at and the factors that explained them.
The study included 391 transplants. The one year survival rate was 86.6% while the five year survival rate was 79.3%. One-year survival was explained by the CHILD classification, sodium levels prior to surgery, and time spent in the ICU. There were no statistically significant factors to explain the five year survival rate.
Keywords
Liver, survival, liver transplantation.
INTRODUCTION
The liver, the largest gland in the body, is essential for protein synthesis, intermediary metabolism and blood detoxification. (4) There are serious liver diseases in which case the transplant is the only solution. The most prevalent diseases and disorders that lead to transplantation include cirrhosis, liver cancer, cholangitis, cholangiocarcinoma, hepatitis and liver trauma. (5) Terminal liver diseases have high prevalence rates throughout the world, and cirrhosis alone causes more than 800,000 deaths annually. (1)
The measure used for success of treatment is survival time. The one-year survival rate, reported by the United Network for Organ Sharing (UNOS) in the USA, was 87.6%. (6) For patients in the European Union between 1988 and 2009, the one-year survival rate was 78%. (7) In Italy it was 81.5%. (8) Research in Catalonia has shown a rate of 85% (9) and in the UK, a rate of 82% was found. (10) Five-year survival rates found in follow-ups include 60.0% by Herraiz et al., 74.0% by Varma et al., and 91.4% by Iruzubieta et al. (11, 12, 13)
An article published by Oscar Santos et al. has reported the experience of a Colombian center with one-year and five-year survival rates of 82% and 72% respectively. (14). Hoyos et al. have presented research about patients with hepatocellular carcinoma in the city of Medellin, with a one year survival rate of 83.2% and a five-year survival rate of 73.2%. (15)
Survival is determined by various clinical and demographic factors. A study in Baltimore, Maryland in the USA combines the results of liver transplantation with variables such as graft quality, surgical technique, immunosuppressive therapy and selection of the recipient. (9) In China, Hu Zhenhua et al. have compared age, gender, vascular invasion and tumor size with survival of liver cancer patients. (16)
A report published by the European Liver Transplant Registry (ELRT) refers to factors such as age and sex of the donor; age, sex, underlying disease and blood type of the recipient, surgical technique and ischemia times. (7). A study by Lei Yu et al. of 63,679 transplants in the USA says that predictors of survival include age, donor's race and sex, and recipient's age, race, sex, body mass index, serum albumin, bilirubin, creatinine, underlying diseases and cold ischemia time. (17)
A publication by the Mercy Medical Center in the US indicates that transplant outcomes depend on the recipient's MELD score, ICU stay, and etiology and on the donor's cold ischemia time, ABO compatibility and graft quality. (9)
An investigation in China included variables such as age, sex, underlying disease, CHILD classification, MELD score, liver tumor characteristics, operative time, transfusion rate, length of stay and complications. (18) Also, a study conducted in Europe between 1968 and 2009 reports that the most frequent indication for liver transplantation was cirrhosis (57.7%), followed by malignant tumors (14.6%). (7)
An investigation conducted in Catalonia between 1984 and 2011 also showed that the most frequent indication for liver transplantation was cirrhosis (49.9%), followed by liver carcinomas (29.2%). (19) In the US, according to UNOS, the most common reason for liver transplantation is cirrhosis (45.1%), followed by hepatocellular carcinoma (20.9%). (6) In the West, 90% of all cases of cirrhosis are attributed to alcohol, fatty liver and viral hepatitis B and C. (20)
From 1968 to 2011, 21,611 liver transplants were performed in Latin America, 1,851 of them in Colombia. (21) According to the report of Donation and Transplant Network of the National Institute of Health, published in 2012, Medellin is the leading city for transplants (34.3%), and the HUSVF is the leading institution in Colombia (27.3%). (22)
The HUSVF has not quantified the survival of patients with liver transplantation. The objective of this research is to determine the clinical and demographic factors associated with survival of patients over the age of 14 years who underwent liver transplantation at the HUSVF from 2002 to 2013.
PATIENTS AND METHODS
A descriptive quantitative study was conducted through cohort tracking and survival analysis. Patients older than 14 years of age who had undergone transplantation at HUSVF between 2002 and 2013 were included. This was a census study that included all patients.
Between 2002 and 2013 a total of 391 transplantations were performed. Due to inconsistencies in demographic data, 36 (9.2%) were not registered in medical records and were not included in the study: 355 patients met the inclusion criteria. Since the objective was to measure patient survival during multidisciplinary treatment, the 54 patients who died during the first 30 days following transplantation for reasons attributable to the surgical procedure were withdrawn from the study. Finally, 301 patients (77%) from the initial base were included.
The dependent variable in this study was survival time measured from the date of transplantation to the date of the patient's death. The independent variables were age, sex, social security, date of transplant, etiology, history of diabetes, previous infections, donor age, preoperative sodium level, ischemia time, intraoperative transfusion, hepatorenal syndrome, days in ICU, renal failure after transplantation, retransplantation, rejection, infection, type of infection, germ isolated, immunosuppression therapy , death, and cause of death. The Child-Pugh Scoreand the MELD score are both international scales based on laboratory results and clinical conditions which are measured in the recipient prior to transplantation.
Study of secondary sources (medical records)
A pilot test was performed with 10 medical records to standardize data collection and adjust the data collection instrument. Telephone calls were made to verify the status of patients who did not have any reported follow-ups in the medical records for the year prior to the study. Within the medical records there were records for 107 living patients and 87 patients who had died. One hundred fifty-nine phone calls were made and data was collected for 36 patients, 21 living and 15 dead. A total of 123 patients were located, and data updated to the most recent last follow-up.
The filled out the data collection instruments were entered into SPSS version 21.0. Kaplan Meier analysis was used to calculate one and five year survival rates. Independent variables were categorized, and survival curves were compared using the Log Rank test with statistical significance at p <0.05. The Hosmer Lemeshow test was applied, and variables with p values <0.25 by Log Rank test were analyzed with a multivariate model. Hazard ratios (HR) and confidence intervals were calculated to identify variables that explain survival.
RESULTS
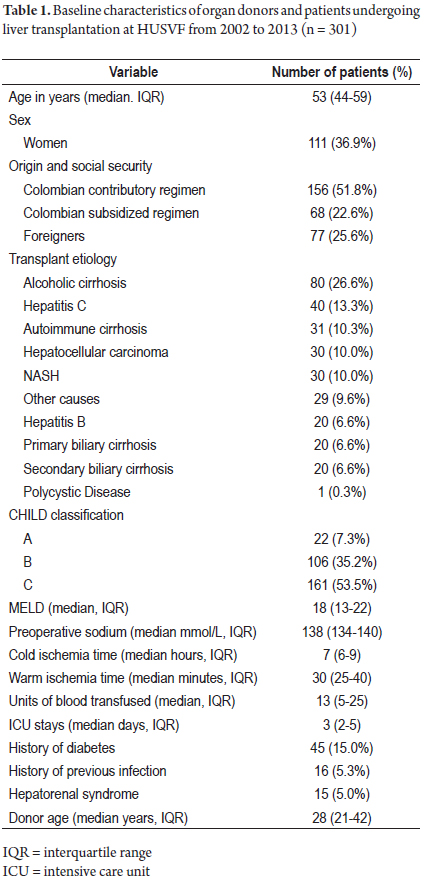
Of the patients who received transplants, 190 were men (63.1%) whose median was 53 years (Interquartile Range [IQR] 43-59). The median age of the women who received transplants was also 53 women (IQR 44-60). The median age of donors was 28 years (IQR 21 to 41.5). Of the total number of patients, 26.2% of patients were foreigners. Of the Colombian patients, 69.8% were affiliated to the contributory health care scheme and 30.2% were affiliated to the subsidized health care scheme. The median MELD score was 18 points (IQR 13-22). Half of the sodium levels recorded were less than or equal to 138 mmol/L (IQR 134-140) (Table 1).
Median cold ischemia time was 8 hours (IQR 6-9). Half of the recipients recorded warm ischemia times of 30 minutes (IQR = 25-40). 50% of patients required up to 14 units of blood (IQR = 5-25). The median ICU stay was 3 days (IQR = 2-5). The leading indication for transplantation was alcoholic cirrhosis with 80 patients (26.6%). 53.5% of patients were CHILD C in the CHILD classification. 45 patients had histories of diabetes (15.0%), fifteen were diagnosed with hepatorenal syndrome (5.0%), and 16 (5.3%) had had previous infections that were recorded in their medical histories (Table 1).
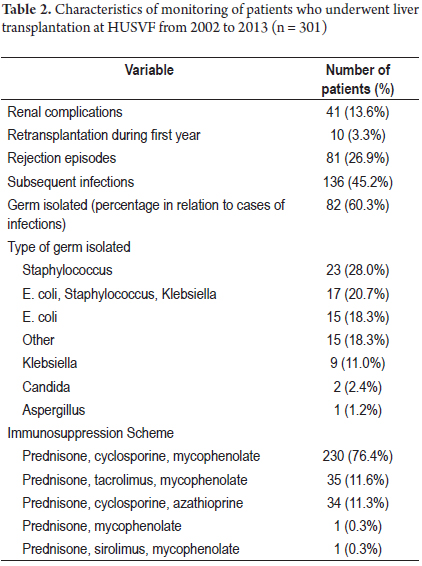
In addition, 41 patients developed subsequent renal complications (13.6%), ten patients (3.3%) required retransplantation before the end of the first year, 136 patients (45.2%) developed subsequent infections, and 81 patients (26.9%) had episodes of rejection. The most common immunosuppressants used were cyclosporine, mycophenolate and prednisone which were administered to 230 patients. Prednisone was common to all combinations of drugs administered (Table 2). Of the 50 patient deaths recorded, 32 were men (64.0%), and 18 were women (36.0%). Causes of death were sepsis (26.0%), liver failure (20.0%), and other causes (18.0%). Thirty percent of the deaths occurred outside the institution.
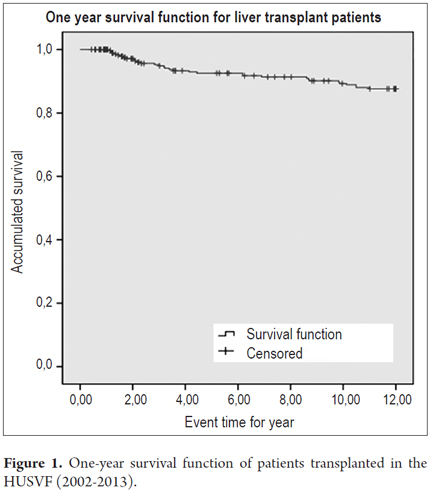
Survival data refer to patients who did not die from causes attributable to the immediate postoperative period. One-year survival was 87.6% with average survival time of 11.1 months (95% CI: 10.8 to 11.4) (Figure 1). Log Rank tests yielded statistical significance for donor age, presurgical sodium, number of days in ICU, renal complications, MELD score, infections, CHILD classification, previous infections, cold ischemia time, warm ischemia time , number of transfused units of blood and hepatorenal syndrome.
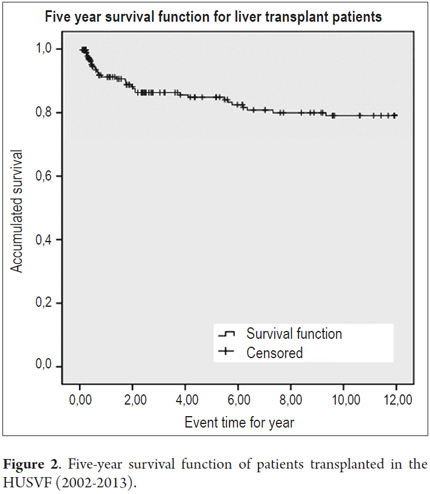
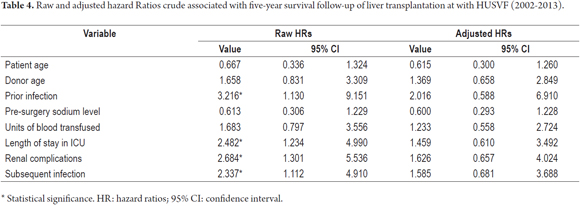
We consider that 218 patients (72.4%) were followed-up period for a five year period. Of these, 33 patients died (15.1%), the five-year survival rate was 79.3%, and the average survival time was 50.44 months (95% CI: 47.46 to 53.42) (Figure 2). The variables included on the basis of Log Rank tests at five years were previous infections, time in ICU, renal complications, subsequent infection, patient age, donor age, preoperative sodium level and units of blood transfused.
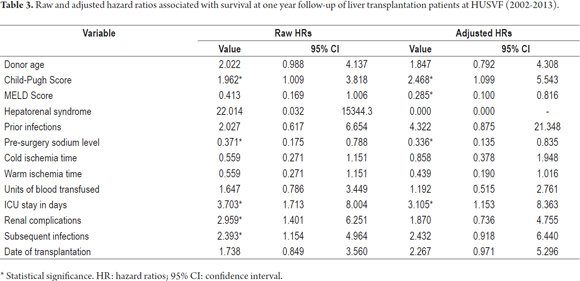
Table 3 shows the raw HR with confidence intervals, at one year of survival. Risk factors include CHILD C classification, stays in the ICU for more than three days, renal complications and subsequent infections. Low preoperative levels of sodium are a protective factor. Other variables did not affect survival at one year. Table 4 contains the raw HR with statistical significance for five-year survival. The presence of a previous infection, length of stay in the ICU, renal complications and subsequent infections are factors that hasten death. In the adjusted model, four variables explain one-year survival: CHILD classification, MELD score, preoperative sodium and time in ICU (Table 3). At five years, none of the variables entered into the adjusted model yield statistical significance (Table 4).
Logistic regression was used to determine factors that explain patient mortality. Child-Pugh Scores (OR = 0.299, 95% CI: 0.102 to 0.876) and length of ICU stay (OR = 0.319, 95% CI: 0.111 to 0.913) help explain one-year mortality. At the five-year follow-up none of the odds ratios calculated show statistical significance.
DISCUSSION
The median age of patients was below the median ages between 54 and 58 years reported by other studies. (23-26). Slattery et al. found that if the age of recipients increases survival decreases. (27) In our study 63.1% of the transplant patients were men which is similar to studies in which the prevalence of liver disease is highest in this group. (23,24,26)
The age of the transplant patients is identical to the results of a study which included 305 patients at another center in Medellin: median age was 52 years. (14) Another Colombian study of patients who received transplants because of liver cancer reported a median age of 58 years. (15) For patients who received transplants because of liver cancer, the average age of patients in this study was lower than that reported in the literature suggesting that hepatocellular carcinomas occur at older ages.
The main reason for transplantation was cirrhosis. Similarly, in Europe cirrhosis is the reason for 57.7% of liver transplants, in Germany it accounts for 52%, and in the US it accounts for 45.1%. (6, 7, 28) Liver tumors account for 14.6% in Europe, 20.9% in the USA, 20% in Germany and 10% in this study. (6,7,28)
The one year survival rate was 87.6%, and the five year survival rate was 79.3% which are similar to the 87.7% and 76.7% rates reported by UNOS. (6) The survival rates reported here were higher than the 84% and 71% rates reported in Europe. (29) Various five years survival rates have been reported: 48.5% by Zhenhua and his team, (16) 70.3% by Pascher, (28) and 80.0% by Kobori et al. (30) The one-year survival rates in this study are slightly more than the 82% (305 patients transplanted for all the causes) and the 81% (for liver cancer patients) obtained in a center of similar complexity located in the same city. (14, 15)
The MELD score is a fundamental variable registered for patients with terminal liver disease. (31). The Hazard Ratios calculated indicate that high MELD scores are a protective factor. In most studies reviewed, this score was associated with survival. This result is contrary to similar studies whose HRs have been presented as risk factors. (23,24,32,33) A study by Batista et al. that measures MELD scores in survival, concluded that the system is valid for measuring pretransplant mortality, but that it has low predictive power for survival. (25)
In this study, patients' ages did not affect survival. A study published by Parekh J. et al. showed an HR of 1.03 (95% CI: 1.00 to 1.06) and reported age as a risk factor. (24) In studies by Vitale et al. and Taioli, Marsh and Hong et al., patient age has no statistical significance that might help explain survival rates. (17,34,35) Ischemia times were not associated with survival. Publications that including ischemia times have obtained HRs between 0.999 and 1.04 but with inconclusive confidence intervals. (24,25,32)
This study included immunosuppression schemes applied, but did not differentiate possible side-effects or changes that frequently occur in these schemes. Iruzubieta et al. have concluded that adherence and the right combination of immunosuppressants influence long-term outcomes. (13) Studies by Pascher and others have pointed to advantages of tacrolimus and mycophenolic acid in terms of survival, although they did not quantify this effect. (28) Prednisone was common to all the immunosuppressant schemes applied and was reported in other studies of liver transplant survival. (27,36 - 38)
A Child-Pugh score of C increases the speed of the event: 53.5% of patients in this study were in this range. Vitale reported that 10.0% of the patients in that study were in the C range, Wan reported 17.7%, Batista reported 20.4%, Zhang reported 29.32% and Fonseca reported 30.7%. (25, 33, 35, 38) Batista and Zhang used the Child-Pugh Score in their survival analyses but obtained results for p of 0.36 and 0.96) which were not statistically significant. (25, 38)
Sodium levels prior to surgery that were above 138 mmol/L had an HR of 0.336. It is considered that sodium values below 130 mmol/L, leads to hyponatremia which is a disease characterized by reduced serum sodium and which complicates transplant outcomes. (39) Slattery and others compared serum sodium levels above 136 mmol/L and did not find any statistical significance. (27) Myers and his team introduced a serum sodium level of 137 mmol/L into the model and obtained an HR of 0.96 (95% CI: 0.95 to 0.97). (40)
ICU time was the factor that best explained short term survival. There are not many studies available that include ICU stay within survival analysis. In a study of 1,164 patients in Canada, Hong et al. found that ICU time increased mortality risk by 22% (HR = 1.22, 95% CI: 1.13 to 1.32). (17) Boin and his team's study, classified ICU stay as a risk factor (HR = 1.03; p = 0.032). (32) Patients who develop subsequent infections showed a crude HR of 2.337. A study by Pappas et al. analyzed the effects of post-transplant infections and showed that the three month survival rate three months decreased from 94% to 78% for patients who developed infections. (41).
Renal complications lead to increased risks. The work of Boin and others which focuses on post-transplant renal failure found a statistically significant HR of 0.98. (32) Laucena and colleagues measured survival's relation to kidney disease and found no associations. (36) This analysis was performed in an exploratory manner with regard to mortality, bearing in mind censoring constraints whose outcomes are unknown.
CONCLUSION
The one year survival rate was 87.6% and, the five year survival rate was 79.3%, with averages of 11.1 and 50.4 months respectively. Child-Pugh Scores, presurgical sodium and ICU stay time help to explain the one-year survival rate, but none of the variables showed statistical significance for the five-year survival rate.
STUDY LIMITATIONS
Although this analysis was based on the cohort of patients from a single center, care must be taken with the extrapolation of data. Not all patient follow-up examinations were recorded in patients' medical histories because insurers can arrange post-transplant treatments in other centers. Foreign patients accounted for 26.5% of all transplants, and these patients left the study before three years of follow-up. The exclusion of postoperative deaths may also result in variations of the results.
RECOMMENDATIONS
We recommend deepening clinical conditions associated with ICU stays that explain survival in detail, conducting additional studies with longer term clinical variables which are longitudinal measures such as diabetes, hypertension, obesity, kidney complications, number of infections suffered, intensity of infections suffered and graft rejection. Additional research that describes the dose, duration, and combinations of immunosuppressive effects on survival of patients is also necessary.
REFERENCES
1. Gómez Adela. Cirrosis Hepática - Actualización. Farm Prof. 2012;26(4):45-51. [ Links ]
2. Starzl TE. History of clinical transplantation. World J Surg. 2000;24:759-82. [ Links ]
3. Instituto nacional de salud. Informe final 2013: Red de donación y trasplantes. Vol Internet. citado 21 de octubre de 2014. Vol 3; 2003. Recuperado a partir de: http://www.ins.gov.co/lineas-de-accion/Red-Nacional. Laboratorios/Estadsticas/INFORME%20ANUAL%202013%20RED%20DE%20DONACION%20Y%20TRASPLANTES.%20Vol%2003.pdf [ Links ]
4. Gardner ED. Gardner-Gray-ORahilly. Anatomy: a regional study of human structure. 5th ed. Philadelphia: Saunders; 1986. 809. [ Links ]
5. Fermín P. Factores que influyen sobre la mortalidad en el trasplante hepático Doctorado. Madrid: Universidad Complutense de Madrid; 1996. [ Links ]
6. UNOS DONATE LIFE Internet. UNOS. 2013. Recuperado a partir de: https://www.unos.org/transplantation/ [ Links ]
7. Adam R, Karam V, Delvart V, OGrady J, Mirza D, Klempnauer J, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012;57(3):675-88. [ Links ]
8. Gruttadauria S, Marsh JW, Cintorino D, Biondo D, Luca A, Arcadipane A, et al. Adult to adult living-related liver transplant: Report on an initial experience in Italy. Dig Liver Dis. 2007;39(4):342-50. [ Links ]
9. Thuluvath P. Evaluation of Liver Transplant Recipients. J Clin Exp Hepatol. 1(3):199-203. [ Links ]
10. Prince MI, Hudson M. Liver transplantation for chronic liver disease: advances and controversies in an era of organ shortages. Posgrad Med J. 2002;78(917):135-41. [ Links ]
11. Moya Herráiz A, Torres-Quevedo R, Mir Pallardó J. Liver transplant in patients with hepatocellular carcinoma. Cir Esp. 2008;84(3):117-24. [ Links ]
12. Varma V, Webb K, Mirza DF. Liver transplantation for alcoholic liver disease. World J Gastroenterol WJG. 2010;16(35):4377-93. [ Links ]
13. Iruzubieta P, Crespo J, Fábrega E. Long-term survival after liver transplantation for alcoholic liver disease. World J Gastroenterol WJG. 2013;19(48):9198-208. [ Links ]
14. Santos O, Londoño M, Marín J. An experience of liver trasplantation in Latin America: a medical center in Colombia. Colomb Médica. 2015;46(1):8-13. [ Links ]
15. Hoyos S, Escobar J, Cardona D, Guzmán C, Mena Á, Osorio G, et al. Factors associated with recurrence and survival in liver transplant patients with HCC--a single center retrospective study. Ann Hepatol. 2015;14(1):58-63. [ Links ]
16. Hu Z, Zhou J, Wang H, Zhang M, Li S, Huang Y, et al. Survival in liver transplant recipients with hepatitis B- or hepatitis C-associated hepatocellular carcinoma: the Chinese experience from 1999 to 2010. PloS One. 2013;8(4):e61620. [ Links ]
17. Hong Z., Wu J., Smart G., Kaita K., Wen S. W., Paton S., et al. Survival Analysis of Liver Transplant Patients in Canada 1997–2002. Transplant Proc. 2006;38(9):2951-6. [ Links ]
18. Lei J-Y, Wang W-T, Yan L-N. «Metroticket» predictor for assessing liver transplantation to treat hepatocellular carcinoma: a single-center analysis in mainland China. World J Gastroenterol WJG. 28 de noviembre de 2013;19(44):8093-8. [ Links ]
19. Organización Catalana de Trasplantes. Registro de Trasplante Hepático de Cataluña. 1984-2011. Barcelona; 2011 p. 65. [ Links ]
20. García Buey L., González Mateos F., Moreno Otero R. Cirrosis hepática. Medicine (Baltimore). 2012;11(11):625-33. [ Links ]
21. Sociedad Latinoamericana y del Caribe de Trasplantes Internet. Latin America Trasplantation. Latin America beating together. Report STALYC. 2011. Recuperado a partir de: http://www.stalyc.net/images/stories/reporte_2011/LAT_repor2011.html [ Links ]
22. Instituto Nacional de Salud. Informe Anual Red de Donación y Trasplante. Bogotá; 2012. p. 75. [ Links ]
23. Ninomiya M, Shirabe K, Facciuto ME, Schwartz ME, Florman SS, Yoshizumi T, et al. Comparative study of living and deceased donor liver transplantation as a treatment for hepatocellular carcinoma. J Am Coll Surg. 2015;220(3):297-304.e3. [ Links ]
24. Parekh J, Corley DA, Feng S. Diabetes, hypertension and hyperlipidemia: prevalence over time and impact on long-term survival after liver transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2012;12(8):2181-7. [ Links ]
25. Batista TP, Sabat BD, Melo PSV de, Miranda LEC, Fonseca-Neto OCL da, Amorim AG, et al. Employment of MELD score for the prediction of survival after liver transplantation. Rev Colegio Bras Cir. 2012;39(2):105-11. [ Links ]
26. Kennedy C, Redden D, Gray S, Eckhoff D, Massoud O, McGuire B, et al. Equivalent survival following liver transplantation in patients with non-alcoholic steatohepatitis compared with patients with other liver diseases. HPB. 2012;14(9):625-34. [ Links ]
27. Slattery E, Hegarty JE, McCormick PA. Its a mans world: does orthotopic liver transplantation in the elderly male confer an additional risk on survival? Can J Gastroenterol J Can Gastroenterol. 2012;26(10):697-700. [ Links ]
28. Pascher A, Nebrig M, Neuhaus P. Irreversible liver failure: treatment by transplantation: part 3 of a series on liver cirrhosis. Dtsch Ärztebl Int. 2013;110(10):167-73. [ Links ]
29. European Liver Tranasplant Registry Internet. ELTR. 2013. Recuperado a partir de: http://www.eltr.org/spip.php?article152 [ Links ]
30. Kóbori L, Görög D, Fehérvári I, Nemes B, Fazakas J, Sárváry E, etal. Progress of the liver transplantation programme in Hungary. Orv Hetil. 2013;154(22):858-62. [ Links ]
31. Wiesner R, Edwards E, Freeman R, Harper A. Modelo para la enfermedad hepática terminal (MELD) y la asignación de hígados de donantes. Gastroenterology. 2003;124(1):91-6. [ Links ]
32. Boin IFSF, de Ataide EC, Dias EPO, Stucchi RSB, Seva-Pereira T, Calomeni G, et al. Can pre-liver transplantation renal insufficiency using a creatinine clearance calculator predict long-term survival? Transplant Proc. 2012;44(8):2452-4. [ Links ]
33. Wan P, Zhang J, Long X, Li Q, Xu N, Zhang M, et al. Serum levels of preoperative α-fetoprotein and CA19-9 predict survival of hepatic carcinoma patients after liver transplantation. Eur J Gastroenterol Hepatol. 2014;26(5):553-61. [ Links ]
34. Taioli E, Marsh W. Epidemiological study of survival after liver transplant from a living donor. J Eur Soc Organ Transplant. 2008;21(10):942-7. [ Links ]
35. Vitale A, Morales RR, Zanus G. Barcelona Clinic Liver Cancer staging and transplant survival benefi t for patients with hepatocellular carcinoma: a multicentre, cohort study. Oncology. 2011;12:654-62. [ Links ]
36. Fonseca-Neto OCL da, Miranda LEC, Batista TP, Sabat BD, Melo PSV de, Amorim AG, et al. Postoperative kidney injury does not decrease survival after liver transplantation. Acta Cirúrgica Bras Soc Bras Para Desenvolv Pesqui Em Cir. 2012;27(11):802-8. [ Links ]
37. Hibi T, Sageshima J, Molina E, Ciancio G, Nishida S, Chen L, et al. Predisposing factors of diminished survival in simultaneous liver/kidney transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2012;12(11):2966-73. [ Links ]
38. Zhang Q, Chen X, Zang Y, Zhang L, Chen H, Wang L, et al. The survival benefit of liver transplantation for hepatocellular carcinoma patients with hepatitis B virus infection and cirrhosis. PloS One. 2012;7(12):e50919. [ Links ]
39. Ginès P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatol Baltim Md. 2008;48(3):1002-10. [ Links ]
40. Myers RP, Shaheen AAM, Aspinall AI, Quinn RR, Burak KW. Gender, renal function, and outcomes on the liver transplant waiting list: assessment of revised MELD including estimated glomerular filtration rate. J Hepatol. 2011;54(3):462-70. [ Links ]
41. Pappas PG, Andes D, Schuster M, Hadley S, Rabkin J, Merion RM, et al. Invasive fungal infections in low-risk liver transplant recipients: a multi-center prospective observational study. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2006;6(2):386-91. [ Links ]











 texto em
texto em