Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.3 Bogotá July/Sept. 2016
Cuban Normality Tables for Psychometric Tests Used for Diagnosis of Minimal Hepatic Encephalopathy
Maykel Alain Padilla Ruiz, MD, MSc (1)
(1) First Degree Specialist in Gastroenterology, Master's in Diagnostic Procedures. Hospital Universitario "Arnaldo Milián Castro" in Santa Clara, Villa Clara, Cuba. padillagastrohepatol@gmail.com
Received: 14-01-16 Accepted: 25-07-16
Abstract
Objectives: Minimal hepatic encephalopathy (MHE) is the subclinical stage prior to the development of clinical hepatic encephalopathy in cirrhotic patients. For these patients, it is associated with impaired quality of life, increased risk of accidents, and incapacity for driving vehicles. The Psychometric Hepatic Encephalopathy Score (PHES) is currently considered to be the diagnostic method of choice for diagnosis of MHE. The aim of this work was to design PHES normality tables for the Cuban population. Population and Methods: The study sample consisted of 520 healthy people from the provinces of Villa Clara, Sancti Spiritus and Cienfuegos who all took the 5 tests included in the PHES. Variables of age, sex, years of schooling, place of origin, and daily alcohol consumption were analyzed. Univariate analysis with the Student's t test, ANOVA and Pearson correlation coefficient was performed. Multivariable linear regression for each test was performed and normality tables were constructed. Results: Multivariate analysis used multiple linear regression with age and years of schooling as the independent variables related to performance for each of the 5 tests. Conclusions: The availability of normality tables provides a diagnostic reference method for PHES which is applicable to Cuban patients with liver cirrhosis without requiring control groups for age and regional education level.
Keywords
Cirrhosis, minimal hepatic encephalopathy, neuropsychological test, numerical connection test, test symbols and numbers.
INTRODUCTION
Minimal hepatic encephalopathy (MHE) and covert hepatic encephalopathy are defined as alterations detected through specific tests or the presence of clinical signs of brain dysfunction in patients with chronic showing liver disease who do not present disorientation or asterixis. The term "covert" encompasses MHE and Hepatic Encephalopathy Grade 1. (1)
MHE can be defined as the presence of measurable cognitive defects or portosystemic shunts (in patients with liver disease) that are not identified through a detailed medical history and a full neurological examination that includes an interview with close relatives, but that are detected due to abnormalities in neuropsychological or neurophysiological tests that can be performed at the bedside and in on an outpatient basis in the absence of other known causes of abnormalities in cognitive tests. Between 60% and 80% of patients with cirrhosis have evidence of MHE. (2-5)
MHE diagnosis is based on:
1. The presence of a disease that can cause MHE (e.g. cirrhosis), the presence of a portosystemic shunt, or both.
2. Normal mental status during clinical examination.
3. Demonstration of the anomalies of cognitive status, neurophysiological variables, or both.
4. The exclusion of concomitant neurological disorders.
Diagnostic tests for MHE have been divided into two main categories: neuropsychological tests and neurophysiological tests. They include the critical flicker frequency test, continuous reaction times measurement, the inhibitory control test, electroencephalograms and the Scan test. (6-15)
The portosystemic encephalopathy syndrome (PSE) test, better known as the psychometric test for hepatic encephalopathy (PHES) evaluates cognitive and psychomotor areas as well as speed and visual and motor coordination. The test is easy to administer and has good external validity. (1)
Although most clinicians agree that MHE is a significant problem that requires an outpatient diagnosis, there are many factors that make routine application of tests difficult including duration, absence of parameters of normal populations for reference, interpretation of results, and the cost of implementation.
In 2001, Weissenborn and colleagues reported the usefulness of a series of 5 psychometric tests for diagnosis of MHE: a digit symbol substitution test (DSST), number connection test A (NCTA), number connection test B (NCTB), a Circle Dotting Test (CDT), and a Line Drawing Test (LDT). They compared the results obtained in cirrhotic patients without encephalopathy with a group of cirrhotic patients with hepatic encephalopathy grade I-II as well as against healthy controls and patients with liver diseases. (16)
There have been large geographical variations in psychometric tests that have been conducted, so that normal values in Germany are different from those of other countries that have conducted research such as Spain, Italy, Mexico, Poland, Korea and China. Because performance on these psychometric tests is influenced by age and educational level, data from a healthy control group matched for age and education are necessary to verify the existence of alterations in the execution of these tests. (16-21)
For these reasons, and given the usefulness of Psychometric Hepatic Encephalopathy Score (PHES) for diagnosis of MHE, we conducted this study to design normal tables for the population of Cuba for the battery of five PHES tests. In the future, they will permit accurate diagnosis of MHE in patients with liver cirrhosis in this population.
MATERIALS AND METHODS
Five hundred twenty "apparently healthy" people over 18 years of age and under 80 years of age were included in the study. Study participants were drawn from people accompanying patients at the Hospital Universitario "Dr. Celestino Hernández Robau" and were from the provinces of Villa Clara, Sancti Spiritus and Cienfuegos. People were included if they had not had the following conditions: impaired liver or kidney function, neurological or psychiatric diseases, other conditions that could affect cognitive function, abuse of alcohol consumption in the last three months (More than 60 g/day for men and more than 30 g/day for women) or consumption of psychotropic drugs.
The subjects selected were stratified by age and education. Written informed consent was obtained and age, and sex, years of schooling, province of origin and province of residence were recorded. Daily alcohol consumption was also recorded. Tests were conducted following the recommendations of their author, using paper and pencil.
NEUROPSYCHOLOGICAL TESTS
The Spanish translation of the battery of five neuropsychological tests was the same one that had been used to perform similar studies in Spain and Mexico which had been generously provided by one of the authors of those studies, Dr. Juan Cordoba, whom I wish to thank once again. The five neuropsychological tests that make up the PHES (DSST, NCTA, NCTB, CDT and LDT) were completed by all patients in a similar sequence. Instructions for conducting the tests are briefly summarized below. (16, 18)
Digit symbol substitution test (DSST)
Each square shows a number at the top and a symbol at the bottom. Each symbol is connected with a number. In exercises below, symbols belonging to the numbers are already filled into the first 5 squares. The test consists of filling in the empty squares with symbols and completing as many symbols as possible in 90 seconds without making mistakes or skipping any squares.
Number Connection Test A (NCTA)
Twenty-five circles numbered from one to 25 are scattered randomly on a sheet of paper. The subject must connect the numbers in order in the shortest time possible without mistakes. If a mistake is made, the subject must stop, correct the error, and then continue without stopping the clock. The time (in seconds) required to complete the test is evaluated.
Number Connection Test B (NCTB)
In this version the 25 circles contain 13 numbers (1 to 13) and 12 letters (A through L). The task is to connect alternating numbers and letters in the shortest time possible without mistakes. As in the NCTA, the subject must stop, correct the error, and then continue without stopping the clock. The time (in seconds) required to complete the test is evaluated.
Circle Dotting Test (CDT)
The subject has to mark the center of each of 100 circles on a sheet of paper with 10 rows of circles in the shortest possible time. The time (in seconds) required to complete the test is evaluated.
Line Drawing Test (LDT)
In this test, the subject has to draw a continuous line between two more or less parallel lines in the form of a maze. The subject's line must not touch or cross the lines of the maze. The number of errors and the time required (in seconds) to complete the test are measured.
The LDT has two results: test taking time and number of errors. These results tend to be complementary, so that subjects who perform the test quickly make many mistakes, while careful subjects make fewer mistakes but take a long time. For this reason, we decided to use the parameter used by Romero in his study which is the sum of the two results. (16)
This new parameter is related to age and years of schooling and also avoids, for example, that a patient presents three standard deviations (SD) in time and one SD in the number of errors.
STATISTICAL ANALYSIS
The number of patients required to determine the "normal reference values" of PHES were determined by age groups and educational levels. Age groups were under 29, 30-39, 40-49, 50-59 and over 60 years of age, and educational levels were six or less years of schooling, nine or less years of schooling, 12 or less years of schooling and more than 12 years of education.
A five by four table was constructed from these parameters with the intention of including at least 20 people in each of the twenty cells. This required at least 400 volunteers: in fact, 520 people were included. It should be noted that we could not complete the cells for people under 39 years of age and with less than six years of schooling due to high general level of education of our population especially among younger age groups. Also, the distribution of the variables was studied by analyzing distribution graphs so that it could be determined if the results of the five tests were normally distributed for the number of cases included. In addition, we analyzed the influence of age, sex, alcohol consumption (higher or lower than 10 g/day), province of origin, province of residence, and years of schooling on performance in each of the five tests. ANOVA tests, Student's t-test and Pearson's correlation coefficient were used.
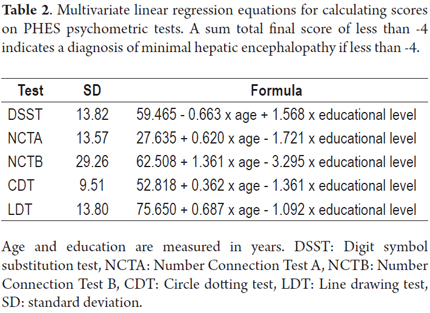
The initial step was identification of the variables that affected each PHES test. Then bivariate analysis was performed for the effects of age, sex, education, province of residence, province of origin, and consumption of alcohol. Variables that affected outcomes of PHES tests were included in a multiple linear regression model. Variables were analyzed to determine the magnitude of their effects, and those with the greatest effects were included in the analysis done by the multiple linear regression model. The results of multiple linear regression were used to construct distribution equations for each test according to the independent variables detected in relation to each of the tests and to age and years of schooling. Finally, we calculated the SD for each test. This allowed us to construct normality tables for each psychometric test based on age and years of schooling. The non-standardized beta coefficient was used in this analysis in the final formula for the correction of these factors.
The value of p was considered to be statistically significant for p <0.05. Statistical analysis was performed using SPSS version 19.0; (Chicago, IL USA). Test results ranged from -2 to +5 points in a group of 200 cases chosen at random indicating that none of the controls suffered from MHE.
RESULTS
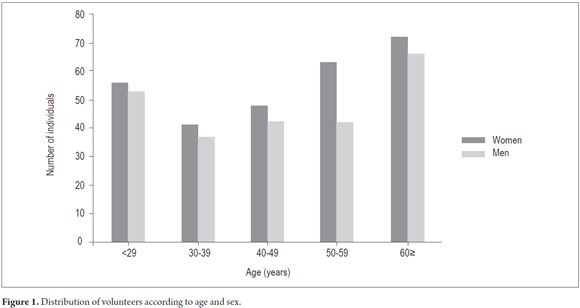
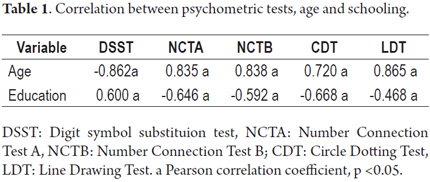
Five hundred twenty volunteers were finally included because 20 of the initial 540 were unable to complete the NCTB. Their average age was 46.83 years ± 16.1 (range 18-73) and their average educational level was and 11.2 years ± 3.9 (range 6-17). Two hundred forty (46.1%) of the participants were men (Figure 1). The distribution of subjects according to age is shown in Figure 2. The results of the five tests showed significant relationships with only two of the variables: age and schooling. Pearson's correlation coefficient for these variables is shown in Table 1.
The results of the tests were not significantly related to sex, province of origin or province of residence. Drinking alcohol only influenced the outcomes of DSST and CDT. Multivariate analysis using multiple linear regression found that the independent variables that influenced the results of all tests were age and schooling. The results of the five tests were the dependent variables. As shown in Figures three and four, younger ages and higher levels of education were associated with better outcomes for DSST. We proceeded to extract the equations that allowed calculation of expected outcomes for each age and level of schooling to achieve the final formulas (Table 2).
DISCUSSION
Activities of daily life are affected by MHE due to cognitive impairment in ways that can have a detrimental effect on the quality of life. MHE primarily affects complex activities related to attention, information processing and psychomotor skills such as driving a car, planning a trip, and shopping. Some studies have shown that patients with MHE have significantly greater impairment of daily functioning in areas such as social interactions, alertness, emotional behavior, sleep, work, home management, recreational pastimes and significantly increased risk of car accidents related to impaired cognitive function than do cirrhotic patients without MHE. Treatment with lactulose improves the functions affected. (22 ,23)
Frequency of MHE increases as severity of liver disease increases. The high frequency of MHE in patients with liver disease should be understood in terms of its impact on the appearance of clinically manifest HE, and it should be understood treatment of MHE may lead to improvements in these results. (5, 7, 24- 26)
Administration of the PHES test battery requires about 15 minutes per patient. There has been a debate about whether all cirrhotic patients who are candidates for liver transplantation, or only those who have risk factors such as data indicative of cognitive impairment, dangerous work tasks or significant loss of work performance should take the PHES tests.
The clinical practice guidelines of the International Society for Hepatic Encephalopathy and Nitrogen Metabolism (Ishen) recommend PHES because it can be administered cross-culturally and requires minimal translation for administration although normal values must be established independently for each country. (27)
DIAGNOSTIC STRATEGIES
Despite advances in diagnosis of MHE, the questions remain: Which patients should be tested for MHE) and How often should they be tested?
Patients with liver cirrhosis, even when they are able to maintain independent lives, are those most frequently affected by MHE. If MHE is suspected neuropsychological tests (PHES) or other tests such as the critical flicker frequency test or the inhibitory control test should be administered. Although there is no consensus on the frequency of application of these tests, some studies suggest they be administered every six months in the absence of acute events. Nevertheless, several authors recommend repetition every one to three months after initiation of treatment. (1, 28)
Additional studies and consensus documents to define methods for diagnosing MHE and patients who should be suspected of MHE are still needed. Meanwhile, liver cirrhosis and its associated complications are currently among the top 10 causes of death in Cuba, and mortality rates from this disease have been increasing in recent years. Hepatic encephalopathy is one of the most frequent and serious complications of cirrhosis, so early diagnosis and timely treatment are important, This study already has provided a new tool for proper assessment of the presence of MHE by making the PHES series for patients with liver cirrhosis applicable to our population. (28)
Conflicts of Interest
The author declares that he has no potential financial, professional or personal conflicts of interest related to this article.
REFERENCES
1. Hendrik Vilstrup, Piero Amodio, Jasmohan Bajaj, Juan Cordoba, Peter Ferenci, Kevin D. Mullen, Karin Weissenborn and Philip Wong. Hepatic Encephalopathy in Chronic Liver Disease: Practice Guideline by AASLD and EASL. The American Association for the Study of Liver Diseases. 2014:12-14. [ Links ]
2. Guerit JM, Amantini A, Fischer C, Kaplan PW, Mecarelli O, Schnitzler A, et al. Neurophysiological investigations of hepatic encephalopathy: ISHEN practice guidelines. Liver Int. 2009;29(6):789-796. [ Links ]
3. Randolph C, Hilsabeck R, Kato A, Kharbanda P, Li YY, Mapelli D, et al. Neuropsychological assessment of hepatic encephalopathy: ISHEN practice guidelines. Liver Int. 2009;29(5):629-635. [ Links ]
4. Bajaj JS, Wade JB, Sanyal AJ. Spectrum of neurocognitive impairment in cirrhosis: implications for the assessment of hepatic encephalopathy. Hepatology. 2009;50(6):2014-21. [ Links ]
5. Sharma P, Sharma BC, Puri V, Sarin SK. Natural history of minimal hepatic encephalopathy in patients with extrahepatic portal vein obstruction. Am J Gastroenterol. 2009;104(4):885-90. [ Links ]
6. Aguilar J, Serrano P. Tratamiento de las enfermedades hepáticas y biliares. CD-ROOM. España: Asociación española para estudio del hígado; 2007. [ Links ]
7. Radha K, Dhiman RK, Chawla YK. Minimal hepatic encephalopathy. Indian J Gastroenterol. 2009;28(1):5-16. [ Links ]
8. Bajaj JS, Hafeezullah M, Franco J. Inhibitory control test for the diagnosis of minimal hepatic encephalopathy. Gastroenterology. 2008;135(5):1591-600. [ Links ]
9. J.S. Bajaj. The Modern Management of Hepatic Encephalopathy: Review Article. Aliment Pharmacol Ther. 2010;31(5):537-547. [ Links ]
10. Kircheis G, Wettstein M, Timmermann L, Schnitzler A, Haussinger D. Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology. 2002;35(2):357-366. [ Links ]
11. Romero-Gómez M, Córdoba J, Jover R, del Olmo JA, Ramírez M, Rey R, et al. Value of the critical flicker frequency in patients with minimal hepatic encephalopathy. Hepatology. 2007;45(4):879-885. [ Links ]
12. Lauridsen MM, Thiele M, Kimer N, Vilstrup H. The continuous reaction times method for diagnosing, grading, and monitoring minimal/ covert hepatic encephalopathy. Metab Brain Dis 2013;28(2):231-234. [ Links ]
13. Bajaj JS, Thacker LR, Heumann DM, Fuchs M, Sterling RK, Sanyal AJ, et al. The Stroop smartphone application is a short and valid method to screen for minimal hepatic encephalopathy. Hepatology 2013;58(3):1122-1132. [ Links ]
14. Amodio P, Del Piccolo F, Marchetti P, Angeli P, Lemmolo R, Caregaro L, et al. Clinical features and survivial of cirrhotic patients with subclinical cognitive alterations detected by the number connection test and computerized psychometric tests. Hepatology 1999;29(6):1662-1667. [ Links ]
15. Weissenborn K, Ennen JC, Schomerus H, Ruckert N, Hecker H. Neuropsychological characterization of hepatic encephalopathy. J Hepatol 2001;34(5):768-773. [ Links ]
16. Romero Gómez M, Córdoba J, Jover R, del Olmo J, Fernández A, Flavià M, Compañy L, Poveda MJ, Felipo V. Tablas de normalidad de la población española para los tests psicométricos utilizados en el diagnóstico de la encefalopatía hepática mínima. Med Clin (Barc). 2006;127(7):246-9. [ Links ]
17. Amodio P, Campagna F, Olianas S et al. Detection of minimal hepatic encephalopathy: normalization and optimization of the Psychometric Hepatic Encephalopathy Score. A neuropsychological and quantified EEG study. J. Hepatol. 2008;49(3):346–53. [ Links ]
18. Duarte-Rojo A, Estradas R ,Hernández-Ramos R , Ponce de León S, Córdoba J, Torre A. Validation of the Psychometric Hepatic Encephalopathy Score (PHES) for Identifying Patients with Minimal Hepatic Encephalopathy. Dig Dis Sci. (2011);56:3014–3023. [ Links ]
19. Ewa Wunsch, Dorota Koziarska, Katarzyna Kotarska, Przemysław Nowacki, Piotr Milkiewicz. Normalization of the psychometric hepatic encephalopathy score in Polish population. A prospective, quantified electroencephalography study. Liver Int. 2013;33(9):1332–1340. [ Links ]
20. Yeon Seok Seo, Sun Young Yim, Jin Yong Jung, Chang Ha Kim, Jin Dong Kim, Bora Keum, et al. Psychometric Hepatic Encephalopathy Score for the detection of minimal hepatic encephalopathy in Korean patients with liver cirrosis. Journal of Gastroenterology and Hepatology. 2012;27(11)1695–1704. [ Links ]
21. Su-Wen Li, Kai Wang, Yong-Qiang Yu, Hai-Bao Wang, Yuan-Hai Li, Jian-Ming Xu. Psychometric hepatic encephalopathy score for diagnosis of minimal hepatic encephalopathy in China. World J Gastroenterol 2013 December 14;19(46): 8745-8751. [ Links ]
22. Zhou YQ, Chen SY, Jiang LD. Development and evaluation of the quality of life instrument in chronic liver disease patients with minimal hepatic encephalopathy. J Gastroenterol Hepatol. 2009;24(3):408-15. [ Links ]
23. Kim Y, Park G, Lee M, Lee JH. Impairment of driving ability and neuropsychological function in patients with MHE disease. Cyberpsychol Behav. 2009;12(4):433-6. [ Links ]
24. Sharma P, Sharma BC, Puri V, Sarin SK. An open-label randomized controlled trial of lactulose and probiotics in the treatment of minimal hepatic encephalopathy. Eur J Gastroenterol Hepatol. 2008;20(6):506-11. [ Links ]
25. Mittal VV, Sharma P, Sharma BC, Sarin S. Treatment of minimal hepatic encephalopathy: A randomised controlled trial comparing lactulose, probiotics and l-ornithine l-aspartate with placebo. Hepatology. 2009;50(Suppl.):4-7. [ Links ]
26. Sharma BC, Sharma P, Agrawal A, Sarin SK. Secondary prophylaxis of hepatic encephalopathy: an open-label randomized controlled trial of lactulose versus placebo. Gastroenterology. 2009;137(3):885-91. [ Links ]
27. Montgomery JY, Bajaj JS. Advances in the Evaluation and Management of Minimal Hepatic Encephalopathy. Curr Gastroenterol Rep. 2011;13(1):26-33. [ Links ]
28. Anuario Estadístico de Salud 2014. Dirección de Registros Médicos y Estadísticas de Salud. Ministerio de Salud Pública de Cuba: 30-32. [ Links ]











 text in
text in