Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.3 Bogotá July/Sept. 2016
Institutional Experience with Cyanoacrylate Treatment of Gastric Varices
Robin Prieto O. MD (1), Germán Carvajal P. MD (1), Eligio Álvarez MD (1), Diego Aponte M. MD (1), Luis Carlos Sabbagh MD (1)
(1) Clínica Universitaria Colombia. Bogotá, Colombia.
This paper was presented at the Colombian Congress of Digestive Diseases in Barranquilla, Colombia on September 4, 2015.
Received: 11-02-16 Accepted: 25-07-16
Abstract
The main causes of upper digestive tract bleeding are ulcers in the stomach and/or duodenum (peptic ulcer disease). With increasing frequency, patients are being seen who have bleeding gastric varices. This may be due to the increasing number of patients who have portal hypertension caused in turn by liver problems, especially cirrhosis. Current options for treatment of gastric varices range include preventive and prophylactic methods. These include therapy using drugs including vasopressin, somatostatin and their analogs, transjugular intrahepatic portosystemic shunts (TIPS) endoscopic methods and surgery. Endoscopic methods include the use of bands and injection sclerotherapy and sealants such as N-Butyl-2-cyanoacrylate (Histoacryl®). Recently, on the basis of literature with increasingly higher levels of evidence and recommendations, we have started using cyanoacrylate at the Clínica Universitaria Colombia. We present our cases and we review the issue.
Keywords
Gastrointestinal bleeding, gastric varices, cyanoacrylate.
QR code to view demonstration video (In Spanish without subtitles) https://youtu.be/aChG6YO_430
INTRODUCTION
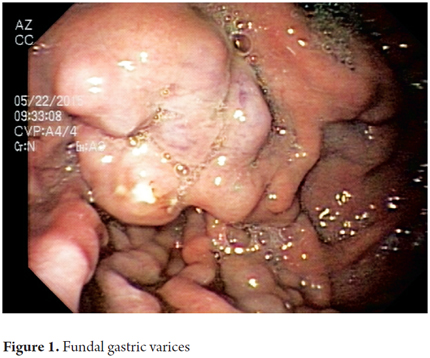
The junction of the superior mesenteric vein and splenic vein gives rise to the portal vein which subsequently divides into right and left branches. The main trunk and the two branches all have significant numbers of tributaries from many organs in the abdominal cavity. Normally, collateral veins connect portal circulation and systemic circulation. Under normal circumstances, the venous flow is directed into the portal circulation and collateral veins remain collapsed. When portal pressure increases because of intrahepatic conditions, especially cirrhosis, collateral veins open up and form varicose veins in various organs and body areas the clinically most important of which is the gastroesophageal junction (Figure 1). (1)
Portal hypertension is a hemodynamic abnormality associated with serious complications of cirrhosis, ascites, hepatic encephalopathy and gastroesophageal varices. It is present in up to 20% of cases and has a high risk of bleeding that can affect 50% to 80% of patients. Although gastric varices bleed less frequently than do esophageal varices, they generally bleed with greater intensity which results in greater rates of morbidity and mortality. Variceal bleeding is a medical emergency that, despite recent progress, has a 6 week mortality rate of approximately 10% -20%. (2, 3)
Suspicion of bleeding varices arises in a high percentage of cases during anamnesis and clinical examination. Generally, these patients have melena or hematochezia, and in most cases they have known histories of esophageal or gastric varices or of portal hypertension. The most important diagnostic and therapeutic tool for these patients is the upper digestive tract endoscopy (UDE) which can identify varices and their locations and whether or not they are bleeding. When there is suspicion of ectopic varices, an enteroscopy, video capsule or venography may be useful for diagnosis. (4)
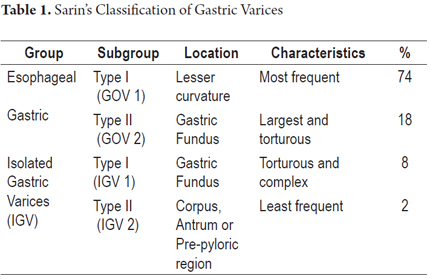
Sarin's classification of gastric varices has been the most widely accepted system and has been recommended by the Baveno V consensus. Sarin classifies gastric varices according to their relationship with esophageal varices and to their locations in the stomach (Table 1). Another system that is in use classifies varices according to their sizes: bigger than 10 mm are called large varices and are at increased risk of bleeding. If the size is between 5 and 10 mm, they are classified as medium and are called varicose veins. Those that are smaller than 5 mm are called small varices and have the lowest risk of bleeding. (5, 6) The risk of bleeding is directly related to the size of varices and increases above a size of 5 mm. Other risk factors red signals and a history of Child-Pugh C cirrhosis. Finally, rupture of a vessel, and therefore bleeding, occur as the result of increased transmural pressure, caused by small increases in portal pressure. (7)
Initial treatment is to achieve hemodynamic stabilization of the patient who may require transfusions or use of vasopressors. In the past, band ligation was considered to be the best treatment for gastric varices, but obturation with cyanoacrylate is being used more and more frequently throughout the world. (8)
Several studies have compared techniques including sclerosis with ethanolamine oleate, band ligation, N-Butyl-2-cyanoacrylate, isobutyl-2-cyanoacrylate and thrombin. These studies have concluded that the use of sclerosing materials or obturation agents is most effective both for initial control of bleeding and for long-term follow-up treatment. Other studies comparing the use of N-Butyl-2-cyanoacrylate with band ligation in patients with bleeding varices have concluded that although control of bleeding is achieved in a similar percentage of patients in both groups, fewer patients treated with N-Butyl-2 cyanoacrylate have recurrences of bleeding after more than a year of follow-up (23% versus 47%). Other studies recommend using cyanoacrylate for fundic gastric varices (IGV1 or GOV2) and consider it to be the therapy of choice for acute bleeding and for secondary prevention of bleeding (Grade of Recommendation 1b: A). (9-12 )
The technique for obliterating gastric varices was first described in Germany in 1986 by Nib Soehendra. Since then its use has increased in Europe, in Asia, and even in America. Currently several associations including the American Association for the Study of Liver Diseases (AASLD) and the American Society of Gastrointestinal Endoscopy (ASGE) recommend obliteration of varices with cyanoacrylate adhesives. This is the first option for patients with bleeding varices in the upper gastrointestinal tract. Vasopressin analogs and somatostatin (terlipressin and octreotide) must be used simultaneously in patients treated urgently for bleeding in order to reduce the pressure of the portal vein and its collateral veins. (3,12 to 14)
The most recent Baveno VI consensus says that since only one study has suggested that injection of cyanoacrylate is more effective than beta blockers for preventing first-time bleeding in patients with large GOV2 or IGV1 (1b; A), more studies are needed to assess the risks and benefits. (15)
Like any other procedure, the use of cyanoacrylate can have complications and there is even risk of systemic embolism and mortality from sepsis. Luckily the risk of complications is low. This technique is just beginning to be used in Colombia, and its use still generates some fear because it requires refined technique. In addition, there are worries about damaging a lens or video endoscope working channel either of which can occur with the use of cyanoacrylate. (12, 13)
TECHNICAL CONSIDERATION FOR CYANOACRYLATE GLUE INJECTION
We began using the cyanoacrylate obturation technique in patients with gastric varices in the gastroenterology unit at the Clínica Universitaria Colombia in 2013. N-butyl-2 cyanoacrylate (Histoacryl) is a monomer that solidifies into an acrylic through a polymerization reaction with hydroxyl ions from blood or water. This immediately causes a mechanical obstruction. The technique was first described more than 30 years ago. When cyanoacrylate is mixed with lipiodol the polymerization process is delayed by up to 20 seconds which prevents polymerization inside the syringe. Because lipiodol is also a contrast agent, its use allows verification imaging of the location of the injected material. This is an advantage that is especially useful in cases of suspected embolization.
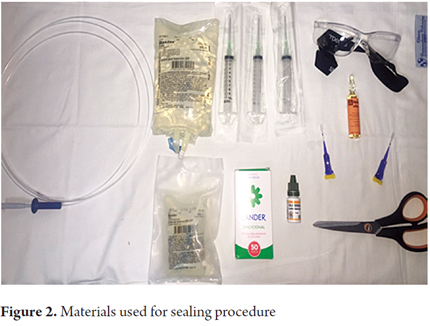
Materials used for application (Figure 2)
- 3 ampoules of Histoacryl®
- 1 ampoule of lipiodol
- 1 bottle glycerin
- Nail polish remover
- Needle and No. 21 sclerotherapy catheter
- 3 mL syringes
- Distilled water
- Front view videoendoscope with standard therapeutic channel
- Goggles, face mask, surgical gloves
Technique
- Conventional upper endoscopy must be performed initially to define the location and characteristics of varices to identifying to which varice(s) cyanoacrylate will be applied.
- Subsequently distilled water is instilled into the 0.8 and 1.5 cc catheter to identify the dead space within it.
- Either the catheter or the working channel and the tip of the working channel of the endoscope should be lubricated with glycerin.
- Next, prepare a one-to-one cyanoacrylate-lipiodol mixture. Then, advance the endoscope with the catheter already inside its channel. This reduces the time and facilitates the process.
- Puncture the varice and inject one to three mL of the mixture into it, followed by distilled water in the preset amount according to the measurement of dead space. You can infiltrate one or more varices (Figure 3).

- The puncture should be made close to the red point or bleeding point if there is one. How the varice distends when the mixture is injected and how it subsequently becomes firm to compression with the catheter should be noted.
RECOMMENDATIONS FOR PREVENTING ADVERSE EVENTS
- Wear protective eyewear.
- Keep suction turned off to prevent damage to equipment.
- Remove the endoscope after securing the needle but without securing the catheter.
- Once the equipment and catheter are outside, you should cut the catheter tip in order to remove it later. This will prevent equipment damage.
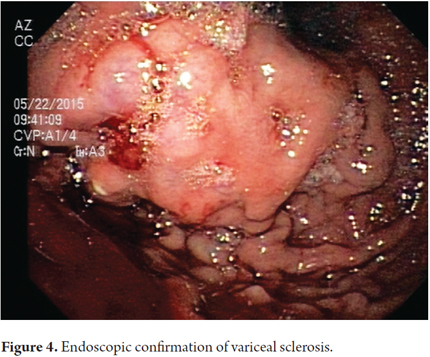
- Perform endoscopy to verify sealing of varices or to seal additional varices (Figure 4).
RESULTS
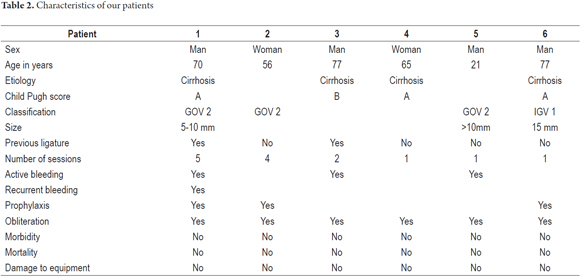
We have treated six patients in a total of 14 sessions of obturation. Table 2 shows the characteristics of these patients. Procedures were performed in four men and two women aged 21 to 77 years. The main cause of varices was Child Pugh A cirrhosis. The main indication for obliteration was prophylaxis of patients with GOV2 varices. In one patient, it was necessary to perform the procedure on two separate occasions due to rebleeding. In all cases adequate sealing of one or even two varices was achieved. Two patients had previously undergone ligation of esophageal varices with elastic bands.
It should be noted that obliteration was successful in all patients, that none of the patients had complications due to the procedure, and that none of the procedures damaged any endoscopy equipment.
DISCUSSION
Peptic ulcer disease is the leading cause of upper gastrointestinal bleeding, followed by gastroesophageal varices. Bleeding gastric varices occurs more and more frequently. Perhaps this is due to increasing frequency of hepatic pathologies that in turn produce increased pressure in the portal vein. Cirrhosis is the most frequent cause according to several studies in Latin America, although in Asian studies extrahepatic causes are considered to be the most frequent. (5,12). In the series presented here, cirrhosis was the main cause of gastric varices. Bleeding gastric varices, although less common than bleeding esophageal varices, usually cause more serious compromises in patients and have higher risks of rebleeding. As in a study by Castillo et al., patients in our series presented GOV2 and IGV1 type varices. We achieved adequate treatment of varices in five of our six patients. (12) It should be noted that one patient developed rebleeding, but this patient had multiple varices that were not obliterated in the first session due to the number of them, and it is likely that the bleeding occurred in another area of multiple varices. The superiority of the cyanoacrylate technique compared with sclerotherapy with ethanolamine oleate and endoscopic ligation has been demonstrated in two randomized studies in which the initial control of bleeding was demonstrated in up to 90% of cases with low recurrence rates (0% -30%) and rates of eradication of gastric varices of up to 75% of cases. (9,16 to 18)
CONCLUSION
We have presented a series of six patients with upper digestive bleeding from gastric varices in whom 14 obliteration procedures with cyanoacrylate were performed. Although, it is clear that the small number of patients and procedures prevent us from extrapolating our conclusions, our results are similar to those observed worldwide. These are our first experiences with this technique: we think that it is safe, that it should be used with caution, and that it should be evaluated prospectively.
REFERENCES
1. Cifuentes SP, Piña AC, Lizarazo JI. Várices ectópicas. Rev Col Gastroenterol. 2008;23(2). [ Links ]
2. De Franchis R. on behalf of the Baveno VI Faculty. Expanding consensus in portal hypertension Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. Journal of Hepatology 2015;63(3):743-52. [ Links ]
3. Mosca I, Ligorría R, Tufare F, Villaverde A, Baldoni F, Martínez H, Chopita N. 3. N-butil-2-cianoacrilato en el tratamiento de las várices gástricas. Acta Gastroenterol Latinoam. 2012;42:27-32. [ Links ]
4. Van Stiegmann G. Diagnosis and management of ectopic varices. Journal of Gastroenterology and Hepatology. 2004;19(Suppl 7):S168-S173. [ Links ]
5. Sarin SK, Lahoti D, Saxena SP, Murthy S, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16(3):1343-9. [ Links ]
6. De Franchis R. Revising consensus in portal hypertension: Report of the Baveno V consensus workshopon methodology of diagnosis and therapy in portal hypertension. Journal of Hepatology. 2010;30(60):1-7. [ Links ]
7. Kim T, Shijo H, Kokawa et al. Risk factors for hemorrhage from gastric fundal varices. Hepatology. 1997;25(2):307–12. [ Links ]
8. Young-suk L. Practical approach to endoscopic management for bleeding gastric varices. Korean J Radiol 2012;13(S1):S40-S44. [ Links ]
9. Huang YH, Yeh HZ, Chen GH, Chang CS, Wu CY, Poon SK, Lien HC, Yang SS. Endoscopic treatment for bleeding gastric varices by N-butyl-2-cyanoacrylate (Histoacryl) injection: long-term efficacy and safety. Gastrointest Endosc. 2000;52:160-167. [ Links ]
10. Augustin S, González A, Genescà J. Acute esophageal variceal bleeding: Current strategies and new perspectives. World J Hepatol. 2010;2(7):261-274. [ Links ]
11. Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33(5):1060-1064. [ Links ]
12. Castillo O, Palacios F, Yoza M, Contardo C, Soriano CC. Uso de Cianoacrilato en la Terapia Endoscópica de várices Gástricas: Experiencia en el Hospital Nacional Edgardo Rebagliati Martins del 2006 al 2010. Rev. Gastroenterol. Perú. 2011; 31(3)208-215. [ Links ]
13. Soehendra N, Nam VC, Grimm H, Kempeneers I. Endoscopic obliteration of large esophagogastric varices with bucrylate. Endoscopy. 1986;18(1):25–26. [ Links ]
14. García-Tsao G, Sanyal AJ, Grace ND, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-938. [ Links ]
15. De Franchis R. Expanding consensus in portal hypertension. Baveno VI. J Hepatol. 2015;63(3):743-52. [ Links ]
16. Wang YM, Cheng LF, Li N, Wu K, Zhai JS, Wang YW. Study of glue extrusion after endoscopic N-butyl-2- cyanoacrylate injection on gastric variceal bleeding. World J Gastroenterol. 2009;15(39):4945-4951. [ Links ]
17. Maluf F, Sakai P, Ishioka S, et al. Endoscopic sclerosis versus cyanoacrylate endoscopic injection for the fi rst episode of variceal bleeding: a prospective, controlled and randomized study in Child-Pugh class C patients. Endoscopy. 2001;33(5):421-7. [ Links ]
18. Mumtaz K, Majid S, Shah HA, et al. Prevalence of gastric varices and results of sclerotherapy with N-butyl 2 cyanoacrylate for controlling acute gastric variceal bleeding. World J Gastroenterol. 2007;13(8):1247-51. [ Links ]











 text in
text in