Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.3 Bogotá jul./set. 2016
Case Studies of Acute Diarrhea in ICU Patients on Enteral Nutrition
Robin Germán Prieto O., MD (1), Ángela María Navas C., MD (2), Fredy Orlando Mendivelso D., MD, MSc (3)
(1) General surgery specialist. Resident in Gastroenterology and Endoscopy. Fundación Universitaria Sanitas, Clínica Colombia in Bogotá, Colombia.
(2) General surgery specialist. Specialist physician in the Nutritional support group. Clínica Reina Sofía in Bogotá, Colombia.
(3) Surgeon, Epidemiologist, Msc Public health, Msc Clinical Epidemiology, Msc Biostatistics. Research Director. Clínica Colsanitas in Bogotá, Colombia.
Received: 10-02-16 Accepted: 25-07-16
Abstract
The administration of enteral nutrition (EN) is frequently mentioned as a cause of diarrhea in patients in Intensive Care Units (ICUs). Because of this, there is a tendency to reduce the use of EN or to even suspend it which often delays patients' nutritional recovery and incurs risks of associated infections.
This is a descriptive study of seven patients that was conducted in the ICU of the Clínica Reina Sofía from July to October 2015. The main criterion for inclusion was the occurrence of diarrhea in patients had been started on EN in the ICU. Statistical analyses used distributions of absolute and relative frequencies expressed in percentages. Measures of central tendency (mean and median) and measures of dispersion (range and standard deviation) were used for quantitative variables. The Shapiro-Wilk test was used to analyze normality.
During the study period seven patients receiving EN who had episodes of diarrhea were identified. The average age of the patients was 73 years. No direct relationships between episodes of of diarrhea and administration of enteral nutrition could be established.
Keywords
Enteral nutrition, acute diarrhea, Intensive Care Unit.
INTRODUCTION
Diarrhea is one of the most common gastrointestinal complications that does not involve bleeding in patients treated in an ICU. According to various studies, its incidence varies between 5% and 64%. Complications of diarrhea can be serious and include skin infections, electrolyte imbalances, dehydration, malnutrition, and hypoalbuminemia. All these changes lead to increased lengths of hospital stays and higher rates of morbidity and mortality.
Diarrhea in ICUs has numerous causes. Because enteral nutrition has been blown out of proportion as a cause of diarrhea, there is a tendency to administer it less frequency and even to suspend its use. This delays the nutritional recovery of patients and increases risks of associated infections through structural alterations in the intestinal mucosa and deterioration of the nutritional status of the patient.
Other causes of diarrhea that have been identified include a variety of drugs, particularly antibiotics, and infectious causes, especially Clostridium difficile. In Colombia, we have not studied the characteristics of patients receiving enteral nutrition during ICU stays who develop diarrhea.
MATERIALS AND METHODS
This is a descriptive case series of adult patients admitted to the ICU at the Clínica Reina Sofía (a high complex institution in Bogotá, Colombia) between July and October 2015. The main criterion was Enteral Nutrition (EN) in ICU patients. Patients who had episodes of acute diarrhea (AD) 48 hours prior to ICU admission were excluded. Statistical analysis used distributions of absolute and relative frequencies expressed in percentages. Measures of central tendency (mean and median) and measures of dispersion (range and standard deviation) were also used for quantitative variables. Normality was analyzed with the Shapiro-Wilks test.
RESULTS
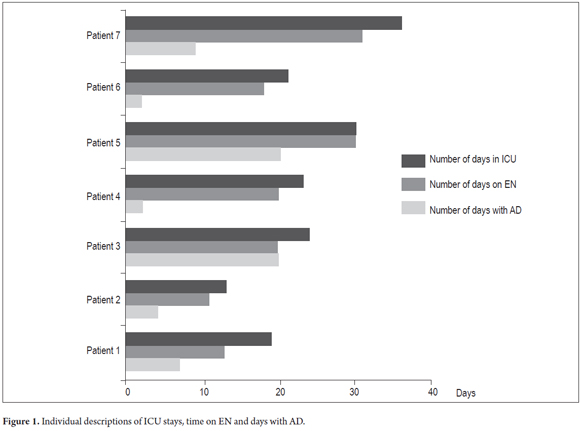
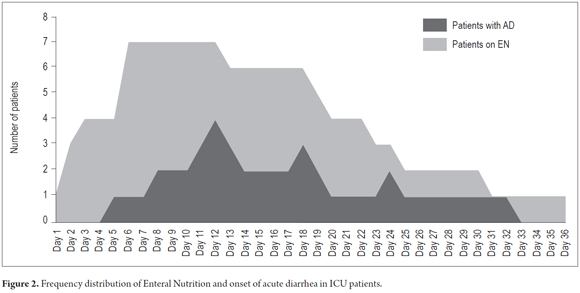
During the study period seven patients who received EN had AD episodes that were identified. The average age of patients was 73 (SD ± 13) years. Most patients were male (71.4%) (Table 1). ICU stays ranged from 13 to 36 days, and administration of EN lasted 11 and 32 days (Figure 1). AD appeared between the fourth and seventeenth day after the start of EN, and its duration ranged from two to twenty (Figure 2). As is to be expected in ICU patients, all patients had polypharmacy due to the severity of their diseases and comorbidities.
Four of the seven patients received sodium picosulfate in the days before onset of AD, and two of them also received evacuation enemas. Both medications were administered because of absence of defecations for more than four days. Another patient received lactulose, before onset of AD. All patients had elevated levels of C-reactive protein and most had elevated levels of procalcitonin. Only one patient was suspected of having a Clostridium difficile infection, but it was ruled by a stool culture and study of toxins.
No direct relationships were established between episodes of AD and EN. Two of the five male patients (40%) died, but no female patients died. Overall mortality was 28.5%, and mortality was not correlated with AD or EN, but rather was due to patients' underlying disease and complex comorbidities.
DISCUSSION
The word "diarrhea" comes from the Latin "diarrhea". The Royal Spanish Language Academy defines diarrhea as a, "morbid symptom or phenomenon consisting of frequent liquid bowel movements." The World Health Organization defines diarrhea, "as having three or more loose or liquid stools per day, or as having more stools than is normal for that person." In the medical literature more than 30 definitions can be found. (1) This indicates the lack of a global consensus that would facilitate study and conclusions regarding this alteration in patients treated in any Intensive Care Unit (ICU ) and that frequently correlates with the administration of enteral nutrition (EN) even though it is not always the cause. (2)
Enteral nutrition is the nutritional pathway used for 46% to 77% of ICU patients, regardless of their underlying diseases. It has been shown that if administered early, it contributes to the preservation of the intestinal mucosa and immune barrier, reduces the risk of sepsis and multiple organ failure (MOF), and promotes healing processes. (3, 4) Nevertheless, EN has been associated with diarrhea, which is one of the most common gastrointestinal complications that does not involve bleeding in patients treated ICUs. Its incidence ranges from 5% to 64%, (5) and it can be as high as 95%. (6) This variation is due to the multitude of definitions of diarrhea, including differences in frequency of bowel movements (over 3 or 4 times a day), consistency (semiliquid, liquid), weight (more than 300 grams per day ) and combinations of these characteristics. Several scales have been designed and various studies have classified stools. Perhaps the most commonly used is the Bristol scale that grades stools on a scale of 0-7. Scores of six and seven indicate diarrheal stools. (7) The Royal College of London scale that classifies stools according to their shape, weight and consistency is also used frequently. (8)
Few studies have evaluated diarrhea in patients treated in ICUs or diarrhea as a complication of EN. In 2008, Borges et al. published a prospective observational study conducted in Brazil with 457 patients. They defined diarrhea as more than two daily liquid defecations over a period greater than 48 hours and found an incidence of diarrhea associated with enteral nutrition of 29.5%. (9) In 2011 Izaguirre and colleagues conducted a study of similar characteristics in 25 ICUs of Spain and found an incidence of 6.4%. They defined diarrhea as three or more loose stools in a 24 hour period. (10)
ETIOLOGY
Since enteral nutrition began to be used, nutritional formulas have been considered to be potential causes of diarrhea in ICU patients. This initial general concept has been disproved now thanks to many studies that have shown various causes of diarrhea (Table 2) in patients treated in ICUs who receive EN. (11-13). It should be noted that many authors believe that the main cause of diarrhea is the drugs received by patients. Antibiotics, particularly broad spectrum antibiotics, can decrease enteral microbial flora and causing alterations of the carbohydrate and amino acid metabolisms resulting in decreased formation of short chain fatty acids which are important for water absorption and electrolytes in the intestine. Although several studies have mentioned the use of laxatives, prokinetics and neuromuscular blockers as causes of diarrhea, a retrospective study in Australia showed no such correlation. (14) A prospective study of 180 patients treated in ICUs in the same country found and a low correlation between the uses of metoclopramide and erythromycin used as prokinetics, but greater correlation when the two were used together. (15) Many drugs such as acetaminophen, ferrous sulfate, and isoniazid in liquid form are hypertonic because they contain syrup or sorbitol. Some tablets contain lactose and are high osmolarity substances which have osmotic laxative effects.
Bacterial, parasitic and fungal infections are other major causes, although there are few studies that have determined the percentages of their involvements. (16) One of the most frequently mentioned causative organisms is Clostridium difficile which only accounted for 5% of cases in a study conducted in several ICUs in Spain. (10) Infections by other germs such as Salmonella, Shigella, Campylobacter and Escherichia coli have also been found to cause AD.
Viral infections represent a major cause of diarrhea in patients in ICUs including in immunocompetent patients. When they occur concomitantly with a bacterial infection, the risk of mortality increases. The most frequently involved viruses are influenza, respiratory syncytial, herpes simplex, and cytomegalovirus. (17)
To a lesser extent, other clinical abnormalities contribute to onset of diarrhea. They include intestinal ischemia associated with cardiovascular or mesenteric disease, common arteriosclerosis in the elderly population; intestinal hypoperfusion related to low cardiac output syndrome, all intestinal malabsorption syndromes, multiple organ failure, absence of the ileocecal valve due to surgery, and short bowel syndrome. (18)
Many patients treated in ICUs have some degree of malnutrition. In these patients it is common to find abnormalities in the gastrointestinal mucosa that impair digestion and absorption of nutrients. Immunological disorders also occur as a result of decreased IgA levels which favors microbial growth and passage of enterotoxins into the bloodstream through the mucosal barrier. All of these factors can lead to the onset of diarrhea (6).
Enteral Nutrition
For various reasons enteral nutrition has been implicated as a cause of diarrhea in critically ill patients cared for in the ICU. As has been mentioned, factors depend on the composition of nutrition. Those that are associated with increased risks of diarrhea include the distribution of macronutrients, composition of caloric intake of more than 20% carbohydrates and fats, hyperosmolarity given by the presence of small solutes, low content of vitamin A (<10,000 IU/L), and low content of sodium (<90 mE/L). (19) FODMAPs (fermentable oligosaccharides and polyols) have also been implicated as laxative agents. (20)
Other factors involved are related to administration techniques: gravity administration of boluses, and at high doses, increases the risk of diarrhea. The use of infusion pumps that regulate the administration of nutrition can reduce this risk. (5) Although some authors relate jejunal administration of nutrition to increased risk of diarrhea, (20) a study by Montejo found no percentage difference between administration of nutrition to the stomach or to the jejunum. (12)
Formulas can become excellent breeding grounds because of their compositions, especially when this is combined with improper handling, failure to adherence to ICU protocols about maximum hang time of the mixture. Colonization by multiple germs that cause diarrhea may occur in critically ill patients. Besides causing diarrhea, contaminated formulas can lead to urinary tract infections, respiratory infections such as pneumonia, and even sepsis. (14) Abnormal water absorption in the colon has also been studied in relation to gastric enteral nutrition. Enteral nutrition to the stomach increases the secretion of water in the ascending colon which may be related to decreased secretion of peptide YY, an intestinal polypeptide that promotes colonic water absorption. During gastric tube feeding, secretion of this peptide decreases. The administration of short-chain fatty acids typically produced by colonic bacteria can reverse this situation and increase water absorption in the colon. (21)
DIAGNOSIS
Most diarrhea that occurs in the ICU is self-limiting to a period of no longer than 72 hours. Physical examination remains of great importance, and the patient should be evaluated for dehydration, abdominal distension and signs of peritoneal irritation. (22)
Once an ICU patient receiving EN has been diagnosed with diarrhea, the etiology should be assessed according to the possibilities presented in Table 1. Check what kind of drugs the patient is receiving, paying special attention to the use of antibiotics and time management as these may be related to the presence of pseudomembranous colitis due to Clostridium difficile or other microorganisms. Administration of prokinetics, laxatives, and hyperosmolar drugs should also be evaluated. (22)
Infectious processes in the intestine must be evaluated by analysis of stool and stool cultures studies, especially for Clostridium difficile. Blood samples must be assessed for leukocytosis and electrolyte disturbances. Sometimes plain abdominal radiographs are useful for assessing obstructive processes, and colonoscopy may be needed for the study of colitis. (23)
EN management should be considered as a cause of diarrhea once the causes mentioned above have been discarded. The composition, volume, hanging nutrition, and method of administration (continuous infusion or boluses) of the formula must be evaluated to identify possible etiologies of AD. (24)
TREATMENT
Given that diarrhea may be transient, the first steps are to guarantee proper replacement of water and electrolytes from the onset of the condition, evaluate drugs, their active compounds and administration, and then monitor the condition without any other definite therapeutic intervention. (25)
Perhaps the most specific treatment that can be administered is for Clostridium difficile. Its severity can be classified as mild (not requiring more than the suspension of antibiotics), moderate (requiring treatment with metronidazole) and severe (requiring treatment with vancomycin). (16, 26)
CONCLUSIONS
Although diarrhea is one of the most common complications in patients treated in ICUs around the world, there have been relatively few studies conducted to evaluate the characteristics of diarrhea in ICU patients receiving enteral nutrition. The current recommendation for EN management in patients with diarrhea is to continue it. The composition or management technique can be changed, but suspension of EN is not recommended since bowel rest produces alterations in mucosal integrity and promotes bacterial overgrowth both of which perpetuate AD. (27) Although some studies suggest the use of probiotics and prebiotics to treat diarrhea, the evidence is unclear, and additional studies are needed. Soluble fiber may be useful for some patients receiving enteral nutrition. (28, 29)
As our presentation is a review of cases, we understand that it does not allow us to draw statistically significant conclusions regarding the use of EN and the onset of diarrhea. Nevertheless, we would lay stress on the fact that a direct relationship between episodes AD and administration of enteral nutrition could not be established in any of our patients. We also consider that studies to design a protocol for the evaluation and management of diarrhea in ICU would be very important. This would prevent unnecessary suspensions of enteral nutrition and establish early diagnosis and treatment of correctable conditions. We think that it would be useful to conduct prospective studies to objectively evaluate the characteristics of patients treated in ICUs who develop diarrhea and the correlation of this condition with the administration of enteral nutrition in Colombian hospitals.
REFERENCES
1. Lebak KJ, Bliss DZ & Savik K. Whats new on defining diarrhea in tube-feeding studies? Clin Nurs Res. 2003;12(2),174-204. [ Links ]
2. Whelan K, Judd PA, Taylor MA. Defining and reporting diarrhoea during enteral tube feeding: do health care professionals agree? Journal of Human Nutrition and Dietetics. 2003;16(1):21-6. [ Links ]
3. Luft VC, Beghetto MG, de Mello EZ, Polanczyk CA. Role of enteral nutrition in the incidence of diarrhoea among hospitalized adult patients. Nutrition. 2008;24(6):528-35. [ Links ]
4. Martin B. Prevention of gastrointestinal complications in critically ill patients. AACN Advanced Critical Care. 2007;18(2):158-66. [ Links ]
5. Martinuzzi ALN, Ferraresi Zarranz EM, Santana Porbén S, Alcántara S, Alonso M. Diarrea en el paciente crítico. Su actualidad. RCAN Rev Cubana Aliment Nutr. 2012;22(1):120-134. [ Links ]
6. Whelan K, Judd PA, Tuohy KM, Gibson GR, Preedy VR, Taylor MA. Fecal microbiota in patients receiving enteral feeding are highly variable and may be altered in those who develop diarrhea. American Journal of Clinical Nutrition. 2009;89(1):240-7. [ Links ]
7. Heaton K. Bristol stool form scale. Family Doctor Books in association with the British Medical Association. Preview Books Online; 2003. Bowels Online. Available: http://www.familydoctor.co.uk Accessed 1st July 2003. [ Links ]
8. Whelan K, Judd PA, Taylor MA: Assessment of fecal output in patients receiving enteral tube feeding: validation of a novel chart. European Journal of Clinical Nutrition. 2004; 58(7):1030-1037. [ Links ]
9. Borges SL, Pinheiro BV, Pace FHL, Chebli JMF. Diarréia nosocomial em unidade de terapia intensiva: incidencia e fatores de risco. Arq Gastroenterol. 2008;45(2):117-24. [ Links ]
10. Izaguirre Guerricagoitia L, Truchuelo Aragón A. Prevalencia de diarrea en las unidades de pacientes en estado crítico de España: estudio multicéntrico. Enferm Intensiva. 2011; 22(2):65-73. [ Links ]
11. Ukleja A. Altered GI motility in critically ill patients: current understanding of pathophysiology, clinical impact, and diagnostic approach. Nutrition in Clinical Practice 2010;25(1):16-25. [ Links ]
12. Montejo JC. Enteral nutrition-related gastrointestinal complications in critically ill patients: a multicenter study. The Nutritional and Metabolic Working Group of the Spanish Society of Intensive Care Medicine and Coronary Units. Crit Care Med. 1999;27(8):1447. [ Links ]
13. Luft VC, Beghetto MG, de Mello ED, Polanczyk CA. Role of enteral nutrition in the incidence of diarrhea among hospitalized adult patients. Nutrition. 2008; 24(6):528-35. [ Links ]
14. Jack L, Coyer F, Courtney M, Venkatesh B. Diarrhoea risk factors in enterally tube fed critically ill patients: A retrospective audit. Critical Intensive and Critical Care Nursing. 2010;26(6),327-334. [ Links ]
15. Nguyen N, Ching K, Fraser R, Chapman M, Holloway R. Risk of Clostridium difficile diarrhoea in critically ill patients treated with erythromycin-based prokinetic therapy for feed intolerance. Intensive Care Med. 2008; 34(1):169-173. [ Links ]
16. Cohen SH, Gerding DN, Johnson S,Kelly CP, Loo VG, Clifford McDonald MDL, Pépin J, Wilcox MH. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hospital Epidemiol. 2010;31(5):431-55. [ Links ]
17. Miggins M, Hasan A, Hohmann S. The potential influence of common viral infections diagnosed during hospitalization among critically ill patients in the United States. PLoS One 2011; 29;6(4):e18890. [ Links ]
18. Montejo JC, Jiménez J, Ordóñez j, Caparrós T, García A, Ortiz C, López J; para el Grupo de Trabajo de Metabolismo y Nutrición de la SEMICYUC Sociedad Española de Medicina Intensiva, crítica y Unidades Coronarias. Complicaciones gastrointestinales de la nutrición enteral en el paciente crítico. Medicina Intensiva [España]. 2001;25:152-60. [ Links ]
19. Barrett JS, Shepherd SJ, Gibson PR. Strategies to manage gastrointestinal symptoms complicating enteral feeding. JPEN J Parenter Enteral Nutr. 2009;33(1):21-6. [ Links ]
20. Halmos EP, Muir JG, Barrett JS, et al. Diarrhoea during enteral nutrition is predicted by the poorly absorbed short-chain carbohydrate (FODMAP) content of the formula. Aliment Pharmacol Ther 2010;32(7):925-933. [ Links ]
21. Whelan K. Enteral tube feeding diarrhoea: manipulating the colonic microbiota with probiotics and prebiotics. Proceedings of the Nutrition society. 2007;66(3):299-306. [ Links ]
22. Kenneally C, Rosini JM, Skrupky LP, et al. An analysis of thirty-day mortality for Clostridium difficile-associated disease in the ICU setting. Chest. 2007;132(2):418-424. [ Links ]
23. McClave SA, Martindale RG, Vanek VW, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2009;33:277. [ Links ]
24. Rushdi TA, Pichard C, Khater YH. Control of diarrhea by fiber-enriched diet in ICU patients on enteral nutrition: a prospective randomized controlled trial. Clin Nutr 2004; 23(6):1344-52. [ Links ]
25. OKeefe SJ. A guide to enteral access procedures and enteral nutrition. Nat Rev Gastroenterol Hepatol. 2009;6(4):207–215. [ Links ]
26. Maroo S, Lamont JT. Recurrent clostridium difficile. Gastroenterology. 2006;130:1311-1316. [ Links ]
27. Whelana K, Schneiderb S. Mechanisms, prevention, and management of diarrhea in enteral nutrition. Current Opinion in Gastroenterology. 2011,27(2):152–159. [ Links ]
28. Barraud D, Blard C, Hein F, et al. Probiotics in the critically ill patient: a double blind, randomized, placebo-controlled trial. Intensive Care Med 2010;36(9):1540–1547. [ Links ]
29. Rushdi TA, Pichard C, Khater YH. Control of diarrhea by fiber-enriched diet in ICU patients on enteral nutrition: a prospective randomized controlled trial. Clin Nutr 2004; 23(6):1344-52. [ Links ]











 texto em
texto em