Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.3 Bogotá July/Sept. 2016
Case Studies and Review of Jackhammer Esophagus
Robin Germán Prieto Ortiz MD (1), Álvaro Andrés Gómez Venegas MD (2), Albis Cecilia Hani de Ardila MD (3)
(1) General Surgeon and Resident in Gastroenterology at the Fundación Universitaria Sanitas. Bogotá, Colombia.
(2) Internist and Gastroenterologist at Gastroclínico Institute in Medellín, Colombia.
(3) Internist and Gastroenterologist, Director of the Unit of Gastroenterology and Digestive Physiology of the Hospital Universitario San Ignacio in Bogotá, Colombia.
This work was presented as a poster at the 2015 ACADI Convention.
Received: 24-09-15 Accepted: 25-07-16
Abstract
Jackhammer esophagus is a peristaltic hypercontractile disorder. According to the second version of the Chicago Classification of esophageal motility, jackhammer esophagus is defined manometrically by distal contractile integrals greater than 8000 mm Hg/cm/s which indicates very high amplitude and velocity. We present a series of five patients with jackhammer esophagus who underwent high-resolution esophageal manometry (HREM) from which clinical and manometric data were collected. There were three men and two women whose ages ranged from 41 to 73. Three of them had been diagnosed with gastroesophageal reflux disease, and showed symptoms of dysphagia, heartburn and regurgitation. The main endoscopic finding was the presence of hiatal hernia and presbyesophagus in two patients. HREM showed waves of up to 4 mm Hg greater than 8000 mm Hg/cm/s. In three of the five patients there were multiple waves. Although, the new third version of the Chicago classification of requires two waves with DCIs over 8000 mm Hg/cm/s to confirm a diagnosis of jackhammer esophagus, it should be noted that we do not yet have available equipment to interpret MAR and allow classifying esophageal disorders by Chicago v.3, and that is why in our physiology unit we still report the MAR with presorting. We conclude that the jackhammer esophagus is a disease with a varied clinical presentation that ranges from dysphagia and chest pain to GERD symptoms. Diagnosis must be confirmed by HREM.
Keywords
Jackhammer esophagus, high resolution esophageal manometry.
INTRODUCTION
Jackhammer esophagus is a hypercontractile esophageal motor disorder. Jackhammer esophagus is defined by high-resolution manometry (HRM) when high amplitude, high speed waves of contractions occur that have a distal contractile integral (DCI) greater than 8000 mm Hg/cm/s. (1, 2) We present a series of five cases with their clinical and manometric features plus a review of the subject.
METHODOLOGY
We reviewed reports from high-resolution esophageal manometry performed in the physiology unit of Hospital San Ignacio in Bogota last year for diagnoses of esophageal jackhammer. Five cases were found. Patients' digestive symptoms were recorded and any additional studies such as upper gastrointestinal tract endoscopy (UDE), barium enemas and HRM were reviewed. Relevant variables for analysis of cases were then compiled. Finally, a search was conducted in PubMed with search terms of Jackhammer esophagus and hypercontractile esophagus. We generated a text with which to review which is appended at the end of the list of references.
CASES
First Case
The patient was a 63-year-old man who had suffered acute myocardial infarction in 2014 that compromised three vessels. It was initially treated with coronary stenting which was followed with surgical myocardial revascularization and two coronary bridges. The patient consulted a physician because of persistent chest pain with atypical features that was accompanied by dysphagia for solids, but no impacted food was found. Cardiological studies ruled out a cardiogenic origin. Upper digestive endoscopy was normal. HRM found 1 of 10 waves with a DCI of 8,351 mm Hg/cm/s. Other waves measured over 5,000 mm Hg/cm/s (Tables 1 and 2 and Figure 1).
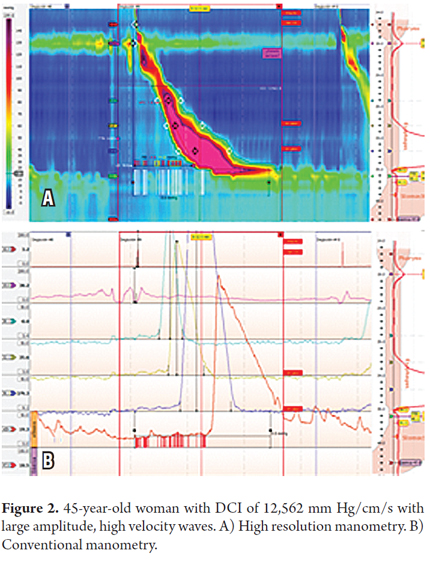
Second Case
The patient was a 45-year-old woman with typical symptoms of gastroesophageal reflux disease (GERD) caused by heartburn and regurgitation without dysphagia or chest pain that was refractory to treatment with proton-pump inhibitors (PPIs). Upper endsocpy showed hiatal hernia and esophagitis. Given that she had been refractory to treatment, HRM was performed. It found that three of every 11 waves had DCIs above 5,000 mm Hg/cm/s, and one of every 11 measured more than 8000 mm Hg/cm/s (12,562). Intrabolus pressure during the HRM was normal (Tables 1 and 2 and Figure 2).
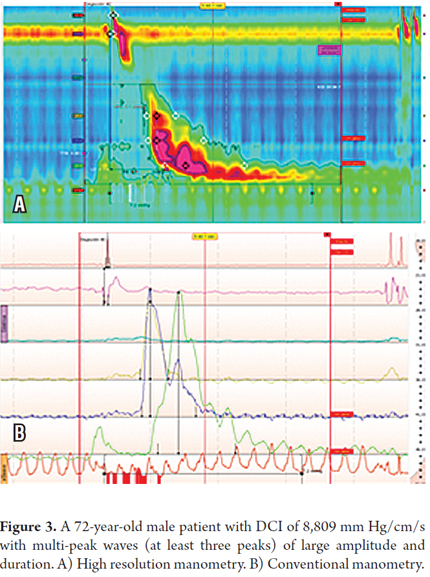
Third Case
The patient was a 72-year-old man with typical symptoms of gastroesophageal reflux disease (GERD) who also had occasional dysphagia for solids. Upper endoscopy showed no abnormalities, but a barium enema showed presbyesophagus and apparent esophageal diverticulum. HRM found three waves with DCIs over 5,000 mm Hg/cm/s, one with a DCI of 8,809 mm Hg/cm/s. There were also six multi-peak waves which reinforced the diagnosis of esophageal jackhammer (Tables 1 and 2 and Figure 3).
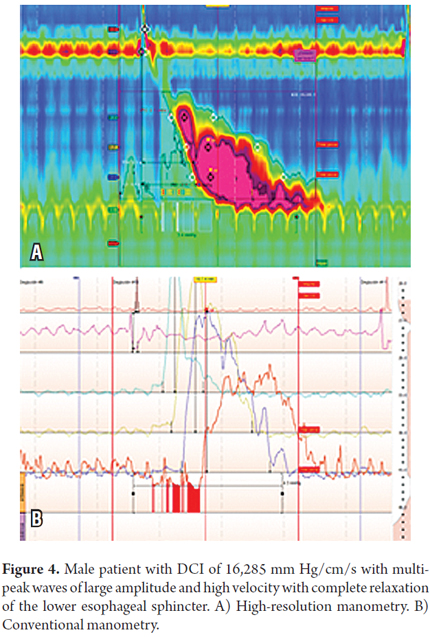
Fourth Case
A 73-year-old male patient with a long-standing history of GERD without dysphagia or chest pain and with typical symptoms that had become refractory to PPIs. Endoscopic revealed a hiatal hernia and presbyesophagus without esophagitis. HRM found that eight out of twelve waves had multiple peaks of more than 5000 mm Hg/cm/s and that four had DCIs above 8,000 mm Hg/cm/s. the highest DCI was 16,285 mm Hg/cm/s. This patient also had a high intrabolus pressure of 26 mm Hg. (Tables 1 and 2 and Figure 4).
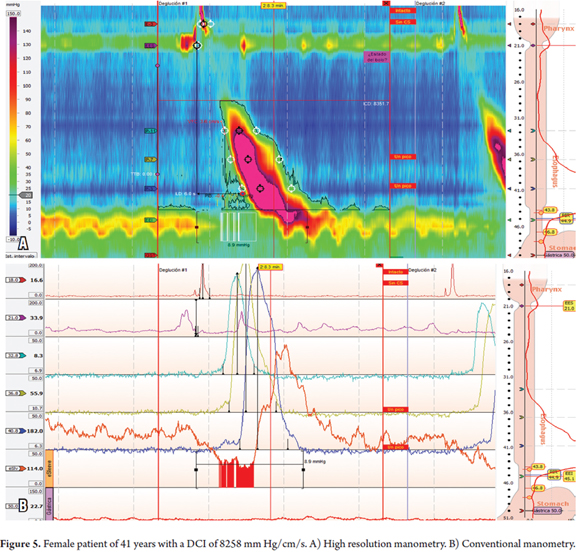
Fifth Case
A 41-year-old female patient who had suffered symptoms of occasional globus pharyngis without dysphagia or chest pain for two years. Upper endoscopy found nothing of significance. HRM showed the 8 of 10 waves had DCIs above 5,000 mm Hg/cm/s and that three of ten waves were multi-peak including one with a DCI above 8,000 (8,258 mm Hg/cm/s) (Tables 1 and 2 and Figure 5).
TOPIC REVIEW
Updating the Classification of Esophageal Contractility Disorders
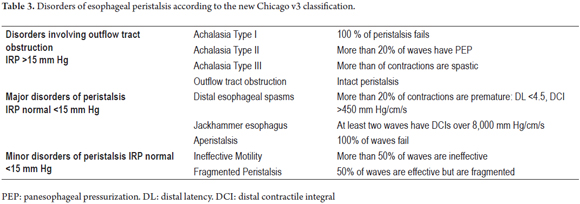
The International Working Group for Gastrointestinal Motility and Function, led by Dr. Peter Kahrilas of Northwestern University in Chicago, Illinois, has taken the responsibility of collecting the available evidence and building consensus criteria for defining esophageal contractility disorders. The latest version of its classification (v.3 Chicago 2015) establishes five groups of results which are based on analysis of functional status of lower esophageal sphincter (LES) and peristalsis. Whether the functional status of the LES is altered is determined by measurement of the integrated relaxation pressure (IRP). (1, 2) It should be our physiology unit still uses the older method for reporting HRM results because it does not yet have the equipment needed for interpreting and classifying esophageal disorders according to Chicago v.3. (1) Based on the new criteria (Table 3) the following three groups of esophageal manometric anomalies have been established:
1. Outflow tract disorders include achalasia Types I, II and III, and outflow tract obstruction (no change from the previous version).
2. Major peristalsis disorders do not have altered IRP (<15 mm Hg). They include diagnoses of distal esophageal spasms with more than 20% of contractions occurring prematurely, aperistalsis (absence of peristaltic waves), and jackhammer esophagus when at least two waves with DCIs over 8,000 mm Hg/cm/s occur. The previous Chicago classifications' criteria for this disorder of a single wave of high contractility is still used in Colombia. The new classification eliminates the diagnosis of nutcracker esophagus since this manometric alteration occurs frequently in healthy patients and is not a real disorder of esophageal contractility.
3. Minor disorders of peristalsis are characterized by normal IRP associated with ineffective waves (more than 50%) in what is now called ineffective motility disorder. If more than 50% of the waves are effective, but are fragmented in equal percentage of cases, fragmented peristalsis is diagnosed. (2)
DEFINITION OF JACKHAMMER ESOPHAGUS
Jackhammer Esophagus is a hypercontractile motor disorder of the esophagus which is diagnosed with HRM when esophageal waves have high amplitude and high speed so that the DCI measures higher than 8,000 mm Hg/cm/s. (1,2) It may be associated with outflow obstructions or abnormalities of the lower esophageal sphincter. (3, 4)
PHYSIOPATHOLOGY
The hypercontractile characteristic of jackhammer esophagus results from temporal asynchrony between contractions of the circular and longitudinal muscle layers of the muscularis and is probably due to excessive cholinergic activity. (5) The detection of these abnormalities in diabetic patients with autonomic neuropathy by Loo et al. supports this hypothesis of excess cholinergic stimulation. (6) In this study, multi-peak contractions were also more frequent in diabetic patients with neuropathy than in control subjects or in diabetics without neuropathy. This may also occur in patients with jackhammer esophagus in whom thickness of the esophageal smooth muscles has also been observed increased. (7)
A clinical and pathophysiological relationship exists between hypercontractile esophageal disorders and GERD. (8) A study by Crespin et al. has found that a large proportion of patients (69.2%) with hypercontractile esophageal disorders also have GERD symptoms of regurgitation and/or heartburn and that 53% had abnormal exposure to acidic pH as measured by esophageal pH monitoring. (9) Some of these patients underwent Nissen fundoplication with resolution of symptoms, decreased exposure to acid pH and, especially, normalization of esophageal peristalsis. The authors conclude that the symptoms of patients with hypercontractile disorders, typical reflux symptoms, and acidity related to GERD, improve with treatment that reduces exposure to acid pH and that this treatment also solves the esophageal contractility disorders.
CLINICAL SIGNS AND SYMPTOMS
Dysphagia, chest pain, regurgitation and epigastric pain are all associated with hypercontractile esophageal disorders but not specific to these disorders. When they are present, other disorders such as cardiac pathologies which may have lethal potential should be ruled out before hypercontractile esophageal disorders are considered. (10). Richter and Castell conducted a study that found that less than 5% of patients with these symptoms had peristalsis disorders demonstrable by esophageal manometry. (11) The combined prevalence of distal esophageal spasms, spastic esophageal achalasia and jackhammer esophagus is only about 2%. (12, 13) The deterioration of transit of esophageal boluses may be the cause of spastic contractions and may explain dysphagia. Chest pain is probably due to altered contractions, and hypersensitivity can be explained by the perception of acidity in patients without demonstrable evidence of reflux. (14) These patients frequently present epiphrenic diverticula which may occur as a result of hypercontractile disorders. The presence of a diverticulum could also explain the symptoms of dysphagia or regurgitation. (15)
DIAGNOSIS
Upper Digestive Tract Endoscopy
The first examination to be conducted as part of the initial study of the symptoms reported by the patient is an upper digestive tract endoscopy even though the results are generally normal. Sometimes endoscopy shows abnormal contractions or changes in the esophageal anatomy. If there is high suspicion, biopsy samples must also be taken to rule out eosinophilic esophagitis, especially when dysphagia is a prominent symptom. (16)
Esophageal Manometry
Esophageal manometry is the diagnostic gold standard for study of abnormal esophageal motility, even more so with the advent of high-resolution manometry. High-resolution manometry is superior to conventional manometry for assessment of the gastroesophageal junction and for quantifying contractile amplitude and wave speed through use of the DCI. (17) Conventional manometry cannot simultaneously monitor the motor function of the upper esophageal sphincter (UES), the esophageal body, and the lower esophageal sphincter (LES) with each swallow while the high-resolution manometry provides this possibility with a full spatiotemporal representation of motor functions of the esophagus. (18) To avoid false hypercontractility waves, there should be intervals of 20 seconds to 30 seconds between each swallow. As has been documented, these small ranges waves with higher DCIs. The criteria for diagnosis of esophageal jackhammer have been discussed earlier in this article.
Esophageal pH Monitoring
Given the relationship of GERD and hypercontractile disorders of the esophagus in patients with typical reflux symptoms (heartburn and regurgitation), measurement of pH in the distal third of the esophagus should be considered before defining treatment. While esophageal pH monitoring is not a perfect method, it allows accurate assessment of the degree of esophageal acid exposure and also correlate patient symptoms with reflux episodes.
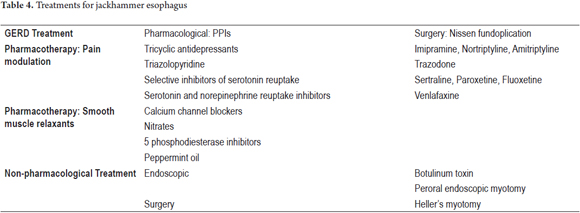
TREATMENT
Given jackhammer esophagus's low prevalence, there is no consensus on management of this condition. Nevertheless, since the study by Crespin et al. and other recent evidence have reinforced the idea that typical GERD symptoms can be related to jackhammer esophagus, initial management of patients who have both should be directed toward decreasing exposure to acid with either medications or surgery. (9) In contrast, for patients with dysphagia and chest pain who do not have GERD symptoms or elevated exposure to acid, management should try to decrease the amplitude of esophageal contractility through relaxation of smooth muscle tissue while also optimizing relaxation of the lower esophageal sphincter. Ideally, management should be by stages: first, seek control of symptoms with medication, either monotherapy or combination therapies; and second, consider the benefit of surgical or endoscopic treatment for refractory cases (Table 4).
MEDICAL MANAGEMENT
Proton-Pump Inhibitors (PPIs)
Proton-pump inhibitors (PPIs) should always be considered the drug of first choice. We recommend using empirical therapeutic at a double dose for 8 weeks. This recommendation is addressed especially to patients with symptoms of GERD, esophagitis and exposure to acid reflux confirmed by esophageal pH monitoring. This monotherapy can be effective for controlling symptoms and may even solve the esophageal motor disorder. (9, 19,20)
Smooth Muscle Relaxants
Nitrates and calcium antagonists appear to reduce the pressure of the lower esophageal sphincter and amplitude of esophageal contraction. These drugs have been studied for use in achalasia and distal esophageal spasms with slight improvements of symptoms and improvements in manometric findings, but have not yet been scientifically tested for treatment of jackhammer esophagus. Another group of drugs with effects similar to those of nitrates are 5-phosphodiesterase inhibitors such as Sildenafil, but evidence for their use in treating hypercontractile disorders is also weak, and they have side effects that include dizziness and headaches which have limited their use. Some experts recommend the use of peppermint oil which has been tested in a small group of patients with distal esophageal spasms and which could be useful since it has with few adverse effects in patients with jackhammer esophagus. (8, 21)
Pain and Sensitivity Modulators
Tricyclic antidepressants should start at very low doses that can be increased each week to achieve the desired goal. They should be administered at night. The most commonly used tricyclic antidepressant is imipramine. In Colombia, nortriptyline and amitriptyline are available. The main side effects are drowsiness, dizziness, weakness, dry mouth, nervousness, tremors, flushing, and prolonged QT intervals. (21, 22) It should be noted that trazodone is the only drug that has shown superiority over placebos in clinical trials in the treatment of patients with jackhammer and nutcracker esophagus. The dose is 100 to 150 mg once a day. There can be drug interactions with alcohol, barbiturates, and other CNS depressants, and it can cause dizziness, drowsiness and fatigue. (23)
Among the selective serotonin reuptake inhibitors (SSRIs), sertraline at usual doses of 50 mg to 200 mg daily and paroxetine at usual doses of 5 mg to 50 mg daily they have been shown to improve symptoms, especially pain. They are contraindicated in patients taking monoamine oxidase inhibitors (MAOIs), and can also cause nausea, decreased libido, insomnia, dry mouth and constipation. (24, 25) The risk of gastrointestinal bleeding may be increased with concomitant use of aspirin or NSAIDs because of the anti-inflammatory effect on platelet aggregation.
ENDOSCOPIC MANAGEMENT
Botulinum Toxin
Endoscopic injection of botulinum toxin has proven useful for relief of chest pain in various studies. The dose varies from 80 U to 260 U, and it may be injected at different sites within the esophagus or at the gastroesophageal junction. Some patients may suffer recurrences in which cases repeated injections of botulinum toxin are required. (26,27)
POEM (Peroral Endoscopic Myotomy)
POEM (peroral endoscopic myotomy) has been proposed for treating patients with hypercontractile esophageal disorders that are refractory to medical management and who have chest pain and dysphagia. Success has been recently reported for patients with nutcracker esophagus, diffuse esophageal spasms and jackhammer esophagus although no data are available regarding long-term outcomes. (28, 29)
SURGICAL MANAGEMENT
For patients with both GERD and jackhammer esophagus, Nissen fundoplication is an alternative therapeutic option to PPIs. Retrospective studies have shown improvement in symptoms and diminished impairment of esophageal contractility. (9) At present, despite case reports, Heller's myotomy is not considered to be standard management for patients with hypercontractile disorders , so risks and benefits of this intervention must be carefully assessed.
CONCLUSION
Jackhammer esophagus is a rare disorder of esophageal contractility. The clinical picture of patients who suffer from this disorder varies from GERD symptoms to chest pain and dysphagia. The gold standard for diagnosis is high resolution esophageal manometry. According to the criteria of the previous version of the Chicago classification, a single altered wave indicates a diagnosis of jackhammer esophagus, but according to the new 2015 Chicago v.3 version, there must be at least two waves with DCIs over 8,000 mm Hg/cm/s. For patients who have this disorder, the manometric path also includes intrabolus pressures and high amplitude multi-peak high waves that reinforce the diagnosis of jackhammer esophagus. Similarly, and as has been mentioned in larger series, a large proportion of these patients had symptoms typical of GERD refractory to treatment with PPIs, which is consistent with the evidence suggesting a cause and effect relationship between the two entities. There is no consensus about treatment, but it appears that reduction of exposure to acid improves symptoms and motor disorders. If the predominant symptoms are chest pain and dysphagia, management with neuromodulators and smooth muscle relaxants should also be provided. Surgical and endoscopic management should be reserved for patients with severe and refractory symptoms.
Financing
This article did not have any financial support.
REFERENCES
1. Kahrilas PJ, Ghosh SK, Pandolfino JE. Esophageal motility disorders in terms of pressure topography: the Chicago Classification. J Clin Gastroenterol. 2008;42(5):627–35. [ Links ]
2. Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE & international high resolution manometry working group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil (2015) 27(2), 160–174. [ Links ]
3. Ghosh SK, Pandolfino JE, Rice J, et al. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007; 293(4):G878–85. [ Links ]
4. Ghosh SK, Pandolfino JE, Zhang Q, et al. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006; 290(5):G988–97. [ Links ]
5. Jung HY, Puckett JL, Bhalla V, et al. Asynchrony between the circular and the longitudinal muscle contraction in patients with nutcracker esophagus. Gastroenterology. 2005; 128(5):1179–86. [ Links ]
6. Loo FD, Dodds WJ, Soergel KH, et al. Multipeaked esophageal peristaltic pressure waves in patients with diabetic neuropathy. Gastroenterology. 1985; 88(2):485–91 [ Links ]
7. Dogan I, Puckett JL, Padda BS, et al. Prevalence of increased esophageal muscle thickness in patients with esophageal symptoms. Am J Gastroenterol. 2007; 102(1):137–45. [ Links ]
8. Roman S, Kahrilas P. Management of Spastic Disorders of the Esophagus. Gastroenterol Clin North Am. 2013;42(1): 27–43. [ Links ]
9. Crespin OM, Tatum RP, Yates RB, Sahin M, Coskun K, Martin V, Wright A, Oelschlager BK, Pellegrini CA. Esophageal hypermotility: cause or effect? International Society for Diseases of the Esophagus. 2016;29(5):497-502. [ Links ]
10. Roman S, Lin Z, Kwiatek MA, et al. Weak peristalsis in esophageal pressure topography: classification and association with dysphagia. Am J Gastroenterol. 2011;106(2):349–56. [ Links ]
11. Richter JE, Castell DO. Diffuse esophageal spasm: a reappraisal. Ann Intern Med. 1984; 100(2):242–5. PubMed: 6691670. [ Links ]
12. Pandolfino JE, Roman S, Carlson D, et al. Distal esophageal spasm in high-resolution esophageal pressure topography: defining clinical phenotypes. Gastroenterology. 2011; 141(2):469–75. [ Links ]
13. Roman S, Pandolfino JE, Chen J, et al. Phenotypes and clinical context of hypercontractility in high resolution pressure topography (EPT). Am J Gastroenterol. 2012;107(1):37–45 [ Links ]
14. Goyal RK, Chaudhury A. Physiology of normal esophageal motility. J Clin Gastroenterol. 2008;42(5):610–9. [ Links ]
15. Tutuian R, Castell DO. Combined multichannel intraluminal impedance and manometry clarifies esophageal function abnormalities: study in 350 patients. Am J Gastroenterol. 2004;99(6):1011–9. [ Links ]
16. Savarino E, Gemignani L, Pohl D et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;34(4):476–86. [ Links ]
17. García J, Sánchez AC, Merino B, Nogales O, González C, Menchén P. Esófago hipercontráctil Jackhammer. Rev Esp Enferm Dig (Madrid). 2015;107(4): 234. [ Links ]
18. Hani A, Leguízamo AM, Carvajal JJ, Mosquera-Klinger J, Costa VA. Cómo realizar e interpretar una manometría esofágica de alta resolución. Rev Col Gastroenterol. 2015;30(1). [ Links ]
19. Fass R, Fennerty MB, Ofman JJ, et al. The clinical and economic value of a short course of omeprazole in patients with noncardiac chest pain. Gastroenterology. 1998;115(1):42–9. [ Links ]
20. Achem SR, Kolts BE, MacMath T, et al. Effects of omeprazole versus placebo in treatment of noncardiac chest pain and gastroesophageal reflux. Dig Dis Sci. 1997;42(10):2138–45. [ Links ]
21. Gillman PK. Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Br J Pharmacol. 2007;151(6):737–48. [ Links ]
22. Cannon 3rd RO, Quyyumi AA, Mincemoyer R, et al. Imipramine in patients with chest pain despite normal coronary angiograms. N Engl J Med. 1994;330(20):1411–7. [ Links ]
23. Clouse RE, Lustman PJ, Eckert TC, Ferney DM, Griffith LS. Low-dose trazodone for symptomatic patients with esophageal contraction abnormalities. A double-blind, placebo-controlled trial. Gastroenterology. 1987;92(4):1027–36. [ Links ]
24. Gillman PK. Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Br J Pharmacol. 2007;151(6):737–48. [ Links ]
25. Varia I, Logue E,OConnor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J. 2000;140(3):367–72. [ Links ]
26. Nebendahl JCBB, von Schrenck T, et al. Treatment of diffuse esophageal spasm with botulinum toxin: a prospective study with 6 month follow up (abstract). Gastroenterology. 1999;116:A802. [ Links ]
27. Miller LS, Pullela SV, Parkman HP, et al. Treatment of chest pain in patients with noncardiac, nonreflux, nonachalasia spastic esophageal motor disorders using botulinum toxin injection into the gastroesophageal junction. Am J Gastroenterol. 2002;97(7):1640–6. [ Links ]
28. Khashab MA, Saxena P, Kumbhari V, et al. Peroral endoscopic myotomy as a platform for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc. 2014;79(1):136–9. [ Links ]
29. Kandulski A, Fuchs KH, Weigt J, Malfertheiner P. Jackhammer esophagus: high-resolution manometry and therapeutic approach using peroral endoscopic myotomy (POEM). Dis Esophagus. 2016;29(6):695-6. [ Links ]











 text in
text in