Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.3 Bogotá July/Sept. 2016
Extrahepatic Manifestations of Hepatitis B.
Laura Penagos MD (1), Luisa Calle MD (2), Óscar Santos MD (3)
(1) General Practitioner at Universidad CES in Medellín, Colombia.
(2) Clinical Hepatologist and Liver Transplantation at the Universidad de Antioquia in Medellín, Colombia.
(3) Clinical Hepatologist and Liver Transplantation in the Hepatology and Liver Transplant Group at the Hospital Pablo Tobón Uribe and the Universidad de Antioquia in Medellín, Colombia. Mail: osmausa@yahoo.com
Received: 07-10-15 Accepted: 25-07-16
Abstract
Chronic hepatitis, liver cirrhosis and hepatocellular carcinoma are the classic manifestations of chronic hepatitis B infections, but up to 20% of patients present extrahepatic manifestations of the infection. The most common extrahepatic presentations are polyarteritis nodosa and glomerular disease, but patients can also develop cutaneous, rheumatological, hematological and neurological manifestations. In this article we present the case of a woman with chronic hepatitis B whose initial manifestation was a flare-up accompanied by leukocytoclastic vasculitis and arthritis. Clinicians should be aware of extrahepatic presentations of hepatitis B because they can be associated with severe complications and may also require separate antiviral treatment independent of that indicated for liver disease.
Keywords
Chronic hepatitis B, extrahepatic manifestations, leukocytoclastic vasculitis.
INTRODUCTION
Hepatitis B virus (HBV) infections are considered to be public health problems globally. (1, 2) About 30% of the world's population has serological evidence of current or previous HBV infections, (1) and approximately 400 million people are chronically infected. (3). Prevalence varies but is higher in developing countries. (1) Colombia is country with low to intermediate HBV prevalence, but in some regions of the country prevalence is over 8%. (4)
Chronic HBV infection is a dynamic process influenced by age at onset and the relationship between viral replication and the host immune system. (2, 5) Less than 10% of adult patients with acute infections progress to chronic infections, (6) but 15% to 40% of individuals with chronic HBV infections develop complications which are associated with increased mortality such as liver cirrhosis, decompensation and hepatocellular carcinoma. (3,5,7-9). There are also various extrahepatic manifestations of HBV which affecting approximately 20% of patients with acute and chronic infections. (10, 11) Clinical presentation varies greatly from subtle signs with no clear relation with viral infection or liver disease to rheumatological, neurological, kidney, skin, blood and even systemic manifestations. (10, 12) We report the case of a patient with extrahepatic manifestations secondary to an HBV infection, and we review the literature.
CASE DESCRIPTION
The patient was a 60-year-old woman who resided in Medellin. For 20 days prior to admission, she had suffered generalized jaundice associated with nausea, abdominal pain, diarrhea but no dysentery, pain in several upper limb joints, and subjective weight loss. Two weeks earlier she had consulted a local second-level hospital where they had diagnosed an acute HBV infection, had treated her symptoms, and had discharged her. She had a medical history of chronic rashes for the previous 10 years and mentioned purpura. The rash was sometimes itchy, had periods of remission and recrudescence, had no clear trigger, and left residual pigmentation. This condition had not been previously studied, but she had been receiving empirical treatment of 5 mg of prednisolone daily for 2 years without showing improvement. The patient reported no previous history of use of alcohol, hepatotoxic drugs, psychoactive substances, exposure to environmental toxins, blood transfusions or tattoos. The patient also said she had not had sex in the last prior months. She had no family history of importance. Upon physical examination it became clear that the patient had mild mucocutaneous jaundice, mild hepatomegaly without tenderness, but no splenomegaly, ascites or collateral circulation. Nevertheless, on both sides of her legs, thighs and buttocks she had bilateral, symmetrical and well-defined purpura plates of up to 5 cm in diameter (Figure 1).
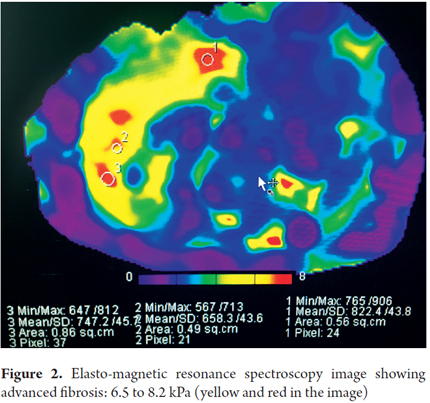
The patient suffered from pain in her metacarpal joints, phalangeal joints and elbows but did not have joint synovitis. Laboratory tests showed ALT of 1,237 U/L, AST of 873 U/L, total bilirubin of 5.2 mg/dL, gamma glutamyl transferase of 535 U/L, serum albumin of 2.6 g/dL, prothrombin time of 13.2 seconds, and INR of 1.21. Her complete blood count showed mild anemia without thrombocytopenia. Serology for hepatotropic virus was positive for Hepatitis B surface antigen (HBsAg), positive for total hepatitis B core antibody (anti-HBc), negative for IgM antibody to hepatitis B core antigen (IgM anti-HBc), negative for hepatitis B envelope (HBe) antigen), and positive for antibodies against HBe antigen. Hepatitis B viral load was 3,559,374 IU/mL. Tests for antibodies against hepatitis C virus and hepatitis D virus as well as ELISA for HIV were negative. A diagnosis of a flare-up of chronic HBV infection with clinical suspicion of cryoglobulinemia was confirmed based on the negative result for HBe antigen, the absence of cirrhosis, the presence of extrahepatic manifestations in the skin and joints. Systemic vasculitis and polyarteritis nodosa also had to be ruled out. On this basis, further testing revealed normal renal function, normal urinary sediment, and low levels of serum complements C3 and C4. Protein electrophoresis showed hypergammaglobulinemia but was negative for antinuclear antibodies and cryoglobulin. Limb electromyography was normal. Laboratory pathology of purpura biopsies was consistent with leukocytoclastic vasculitis of small vessels. Ultrasound showed no changes indicating cirrhosis or portal hypertension but did show mild ascites which prevented performance of percutaneous liver biopsy. Elasto-magnetic resonance spectroscopy showed increased hepatic stiffness (6.5 to 8.2 kPa) consistent with advanced-F4 fibrosis (Figure 2).
Essential mixed cryoglobulinemia, polyarteritis nodosa and hypocomplementemic urticarial vasculitis were discarded. The diagnosis of chronic hepatitis B infection with Child-Pugh B liver cirrhosis was confirmed along with a reactivation flare-up and non-cryoglobulinemic type, non-polyarthritis extrahepatic vasculitis. Treatment with 0.5 mm of entecavir per day was begun as well as administration of Clobetazol, a high potency topical steroid type, for purpura. The patient slowly improved despite mild biochemical deterioration of the liver during the first days of treatment. She was discharged 10 days later. At her three-month follow up examination her clinical evolution was good, her hepatic biochemical profile was normal, her joint symptoms had resolved, and her skin lesions had improved considerably.
DISCUSSION
Chronic HBV infections are a well-documented cause of liver cirrhosis and hepatocellular carcinoma. (3, 5, 8, 9) Nevertheless, extrahepatic manifestations are often forgotten even though they may be associated with significant morbidity and mortality. The prevalence of these manifestations is low (10% to 20% of patients) and has even declined in recent years. (11) Extrahepatic manifestations are sometimes difficult to diagnose because they can be atypical and have no clear temporal relationship with the symptoms of hepatitis. They also may occur in patients who have no evidence of chronic liver disease. (10) The pathophysiology of these manifestations has still not been fully elucidated, but the best accepted theories are that they are caused by circulating autoantibodies, deposition of immune complexes, local formation of immune-induced viral antigens, autoantibodies generated by the virus (which react against tissue), and/or development of a direct viral reaction at extrahepatic sites. (12) The most common extrahepatic manifestations include polyarteritis nodosa, serum sickness-like reaction, essential mixed cryoglobulinemia, nephropathy, dermatologic manifestations, arthritis and neurological involvement. (13)
Polyarteritis nodosa is a necrotizing vasculitis that occurs in up to 5% of chronic HBV infections. It manifests early in the first 6 months after infection and is a sudden, severe illness. (14) It results in hypertension, eosinophilia, abdominal pain, weight loss, polyarthralgia, and subsequent kidney, gastrointestinal and neurological involvement. (14) Patients may present with palpable purpura on lower extremities which can progress into large ulcers. These are sometimes associated with painful subcutaneous nodules and livedo reticularis. (15)
Serum sickness-like reaction is a condition that can occur in 10% to 30% of patients in the prodromal phase of HBV infection. It can result in arthritis and arthralgia with generally symmetrical distribution but which especially affects the small joints of the hands and feet. Occasionally, it is asymmetrical, affects only one joint, or affects large joints. (12) Macular petechial, outbreaks of rashes, and purpura may develop. (12) In addition to palpable purpura, other possibilities include Henoch-Schonlein purpura, multiform erythema, toxic erythema, angioneurotic edema and lichenoid dermatitis. (12, 15)
Essential mixed cryoglobulinemia is a systemic disease that begins with the reversible precipitation of immunoglobulin in a cold environment. (15) Although it most common in chronic hepatitis C infections, its prevalence ranges from 1% to 15% in patients with HBV. (15) Its classic manifestations are purpura, arthralgia and weakness. Less can often glomerulonephritis, pulmonary complications, neurological involvement, and systemic vasculitis develop. (12) Unlike polyarteritis nodosa, this condition only affects small vessels and does not result in peripheral eosinophilia or cause aneurysms. (10)
Nephropathy associated with chronic HBV infection is mediated by immune complexes. (16) Usually it manifests as nephrotic syndrome in both children and adults. It occurs primarily among boys and men. (12) The most common form is membranous nephropathy, but membranoproliferative glomerulonephritis and mesangial proliferative glomerulonephritis may also develop. (16) The prognosis varies with age: it is self-resolving in 95% of children, but 25% of adults progress to advanced kidney failure. (12, 16)
Another manifestation is joint polyarthritis which can occur in either the acute episode, the pre-icteric phase, or the chronic phase of the disease. (11) It compromises the joints of the hands and may be asymmetrical. (12) Deposition of immune complex and cryoprecipitate containing immunoglobulin and complement elements in the synovium of patients with chronic infections has been demonstrated to be a cause of this phenomenon. (11, 12) Some patients may have positive rheumatoid factor, but the absence of joint destruction visible in imaging differentiates joint polyarthritis from rheumatoid arthritis. (11) Cases of peripheral neuropathy associated with acute and chronic HBV infections have also been reported. (12) Immune complexes with HBV surface antigen virus have been found in cerebrospinal fluid of infected patients which indicates the pathogenesis of these extrahepatic manifestations. (11)
Dermatological manifestations in chronic HBV infections vary and may be part of systemic syndromes, or just limited to skin involvement. (12) Urticaria, maculopapular rash, and lichen planus are the most common. These manifestations most often occur in women, are episodic, and are usually pruritic. Gianotti-Crosti syndrome (also known as infantile papular acrodermatitis) sometimes develops in children. (11) The syndrome is characterized by 2-3 mm papular or vesicular lesions on the face and distal extremities which are erythematous without pruritus. It can last up to 15 days. (17) Axillary and inguinal lymphadenopathy, splenomegaly and hepatomegaly, anorexia, weight loss and diarrhea may also develop. (11) Caroli's triad of acute urticaria, headaches and arthralgia is another manifestation that has been associated with HBV, especially in the acute phase of the disease. (11) It is estimated that 8% of cases of leukocytoclastic vasculitis are caused by hepatitis C virus. (18) This type of vasculitis has also been described in hepatitis B virus infections but is uncommon, although in the literature there are no exact data on its appearance in chronically infected patients. (11)
Although some indications have been established for treatment of patients with chronic hepatitis B infections, all patients with extrahepatic manifestations of the disease require medical treatment. Of the currently available options, patients should receive treatment with a nucleoside or nucleotide analogue but should not be treated with Interferon which can worsen some of the manifestations that are immunologically mediated. (3)
Key points in the case presented here include the fact that the patient was initially diagnosed at another institution with acute hepatitis B infection due to jaundice and very elevated transaminases. However, the patient had no recent exposure to any risk factors and her antibody profile (anti-HB core total positive, anti HB IgM core negative, HBeAg negative, AntiHBe positive) was consistent with chronic HBV infection. Her transaminase levels were 10 times higher than normal, but this is not uncommon in the natural history of hepatitis B infections. The possibility of liver cirrhosis was suspected because of the presence of hypoalbuminemia, and mild ascites on ultrasound. A liver biopsy was in order, but in our hospital percutaneous liver biopsies are not performed on patients with ascites due to high risk of bleeding. A transjugular biopsy was considered but rejected due to the low yield and high cost. We also do not have fibro-scan for noninvasive assessment of liver fibrosis. The only method we have is elasto-magnetic resonance spectroscopy which does not require contrast medium for post-processing and which ensures proper evaluation of the whole liver. This can be performed in patients with obesity and ascites and moreover allows visualization of early morphological changes due to chronic liver disease or portal hypertension.
In conclusion, chronic HBV infections are associated with various extrahepatic manifestations that we must learn to recognize and treated promptly to avoid complications that may endanger the lives of our patients.
Source of financial support
None
REFERENCES
1. Trépo C, Chan HLY, Lok A. Hepatitis B virus infection. Lancet. 2014;384(9959):2053-63. [ Links ]
2. Carneiro de Moura M, Marinho R. Natural history and clinical manifestations of chronic hepatitis B virus. Enfermedades Infecc Microbiol Clínica. 2008;26(7):11-8. [ Links ]
3. European Association For The Study Of The Liver. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2012;57(1):167-85. [ Links ]
4. Roman S, Jose-Abrego A, Fierro NA, Escobedo-Meléndez G, Ojeda-Granados C, Martínez-López E, et al. Hepatitis B virus infection in Latin America: a genomic medicine approach. World J Gastroenterol WJG. 2014;20(23):7181–96. [ Links ]
5. Fattovich G. Natural history and prognosis of hepatitis B. Semin Liver Dis. 2003;23(1):47–58. [ Links ]
6. Locarnini S, Hatzakis A, Chen D-S, Lok A. Strategies to control hepatitis B: Public policy, epidemiology, vaccine and drugs. J Hepatol. 2015;62(1):S76–86. [ Links ]
7. Ganem D, Prince AM. Hepatitis B virus infection-natural history and clinical consequences. N Engl J Med. 2004;350(11):1118–29. [ Links ]
8. Lok ASF, McMahon BJ. Chronic hepatitis B. Hepatol Baltim Md. 2007;45(2):507–39. [ Links ]
9. Lin C-L, Kao J-H. Hepatitis B viral factors and clinical outcomes of chronic hepatitis B. J Biomed Sci. 2008;15(2):137–45. [ Links ]
10. Pyrsopoulos NT, Reddy KR. Extrahepatic manifestations of chronic viral hepatitis. Curr Gastroenterol Rep. 2001;3(1):71–8. [ Links ]
11. Cacoub P, Terrier B. Hepatitis B-related autoimmune manifestations. Rheum Dis Clin North Am. 2009;35(1):125–37. [ Links ]
12. Han S-HB. Extrahepatic manifestations of chronic hepatitis B. Clin Liver Dis. 2004;8(2):403–18. [ Links ]
13. Cacoub P, Saadoun D, Bourlière M, Khiri H, Martineau A, Benhamou Y, et al. Hepatitis B virus genotypes and extrahepatic manifestations. J Hepatol. 2005;43(5):764–70. [ Links ]
14. Jones AM, Warken K, Tyring SK. The cutaneous manifestations of viral hepatitis. Dermatol Clin. 2002;20(2):233–47. [ Links ]
15. Nishida N, Kudo M. Clinical Features of Vascular Disorders Associated with Chronic Hepatitis Virus Infection. Dig Dis. 2014;32(6):786–90. [ Links ]
16. Bhimma R, Coovadia HM. Hepatitis B Virus-Associated Nephropathy. Am J Nephrol. 2004;24(2):198–211. [ Links ]
17. Akhter A, Said A. Cutaneous manifestations of viral hepatitis. Curr Infect Dis Rep. 2015;17(2):452. [ Links ]
18. Sharlala H, Adebajo A. Virus-induced vasculitis. Curr Rheumatol Rep. 2008;10(6):449–52. [ Links ]











 text in
text in