Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.3 Bogotá jul./set. 2016
An Unusual Finding of a Dieulafoy's Lesion in the Duodenum
Angélica Rojas D. MD (1), Germán David Carvajal P. MD (2), Robin Germán Prieto O. MD (3), Diego Mauricio Aponte M. MD (4)
(1) Internal medicine specialist. El Bosque University. Bogotá, Colombia.
(2) General surgery, gastroenterology and endoscopy specialist. Clínica Universitaria Colombia in Bogotá, Colombia.
(3) General surgery specialist. Second year gastroenterology and endoscopy resident at the Fundación Universitaria Sanitas in Bogotá, Colombia.
(4) Gastroenterology Program Coordinator at the Fundación Universitaria Sanitas. Gastroenterology, Clínica Universitaria Colombia in Bogotá, Colombia.
Received: 27-11-15 Accepted: 25-07-16
Abstract
Dieulafoy's lesions do not usually cause upper gastrointestinal bleeding, but they are one of the most common causes of hidden and recurrent bleeding. An extra-gastric Dieulafoy lesion is rare, and, because of their location, Dieulafoy's lesions in the duodenum are difficult to diagnosis and treat. Endoscopic injection therapy combined with adrenaline injections and mechanical therapy reduce the risk of rebleeding. This article describes the case of a patient treated at the Clínica Universitaria Colombia and reviews the topic of Dieulafoy's lesions.
Keywords
Gastrointestinal bleeding, Dieulafoy's lesion, duodenal, endoscopic hemostasis.
QR Code
View the procedure at https://youtu.be/tcoAIT5Alww
INTRODUCTION
The annual incidence of acute gastrointestinal bleeding ranges from 50 to150 cases per 100,000 population. Almost 80% of patients are caused by peptic ulcers, esophageal erosion and gastroduodenal erosion. (1) Occult digestive bleeding accounts for 5% of all gastrointestinal bleeding and one of its causes is Dieulafoy's lesion (DL). It is potentially fatal and accounts for 0.1% of acute hemorrhages. (1)
The majority of DL cases are found in the stomach within 6 cm of the gastroesophageal junction. The extragastric location of the case reported here is rare. (2) Lack of knowledge about the Dieulafoy's lesion increases the morbidity and mortality of the patients who suffer from it, and it should be noted that this patient had recurrent upper gastrointestinal bleeding secondary to Dieulafoy's lesion in the duodenum.
CASE PRESENTATION
A 26-year-old man was admitted to the emergency department after four days of melena associated with hematemesis, asthenia, adynamia and one episode of lipothymia. The patient said he had not taken any non-steroidal anti-inflammatory drugs (NSAIDs) recently. He had had recurrent gastrointestinal tract bleeding at the ages of 7, 8, 9 and 15 years. In those episodes, upper digestive tract endoscopy failed to find the source of bleeding.
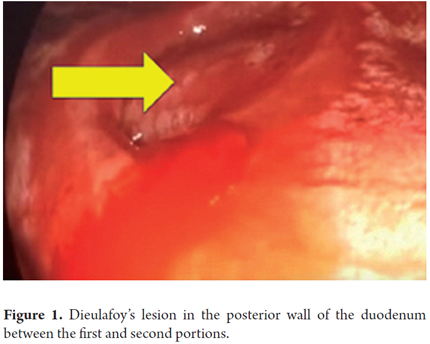
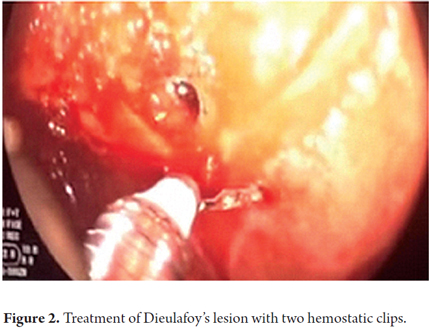
The initial physical examination found the patient's general condition to be abnormal with a generalized mucocutaneous pallor and the following vital signs: Arterial blood pressure: 90/60, HR: 110 bpm, respiration rate: 16 rpm, and SaO2: 90%. The abdomen was soft, without pain on palpation pain, and without signs of peritoneal irritation. A rectal examination showed melena. Hemoglobin at admission was 15 g/dL and hematocrit was 42%. A blood test six hours after admission showed anemia with hemoglobin of 13 g/dL and hematocrit of 36%. Renal function was in the prerenal range with BUN of 26 and creatinine of 0.84. Upper endoscopy showed that the mucosa of the esophagus and cardia were normal. Dark sticky blood was present in the mucous of the fundus, corpus and antrum. The pylorus appeared to be normal. A an active jet of blood that was compatible with Dieulafoy's lesion was found between the first and second portion of the posterior wall of the duodenum (Figure 1), A 1:10,000 adrenaline solution was injected and two hemostatic clips were placed to completely control bleeding (Figures 2 and 3).
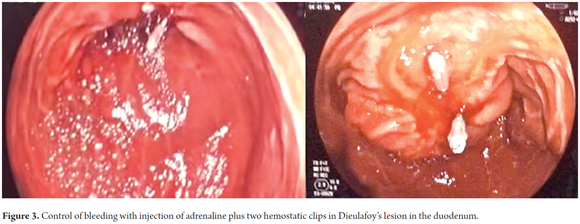
Upper digestive endoscopy 12 hours later found no bleeding where the hemostatic clips had been place on Dieulafoy's lesion. The patient progressed satisfactorily without hemodynamic instability and without rebleeding. He was discharged and followed up as an outpatient.
DISCUSSION
Dieulafoy's lesion was originally described by Gallard in 1884 as a miliary aneurysm of the stomach. (3) In 1898, the French surgeon Georges Dieulafoy described it more accurately after autopsy studies of fatal digestive hemorrhages in three asymptomatic young men. (2) It is characterized by a histologically normal artery that has an abnormally large diameter (1-3 mm), a tortuous path, and which protrudes through a small defect of the mucosa that varies in diameter from 2 mm to 5 mm. (1) Histologically Dieulafoy's lesion is a small defect of the submucosa with fibrinoid necrosis at its base. This covers a tortuous artery whose walls have been thicker because of thickening of the muscularis of the mucosa and subintimal fibrosis. This condition is characterized by absence of inflammation or ulcers in the surrounding mucosa. It usually occurs in adults and is twice as common in men as in women. It is rarely detected in children younger than 15 years of age. (3)
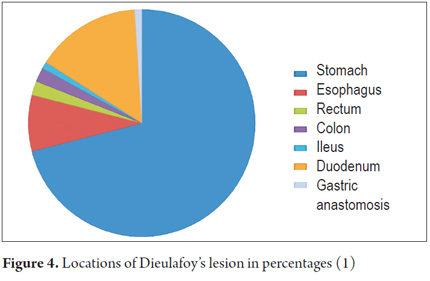
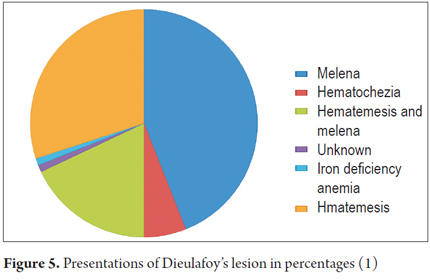
Approximately 75% to 95% of these lesions are located within the proximal 6 cm below the gastroesophageal junction, especially predominantly in the lesser curvature. The remaining 5% are extragastric lesions located in the esophagus, duodenum, jejunum, colon and rectum (Figure 4). (4, 5) It should be noted that the pathogenesis of Dieulafoy's lesion is unknown. In the past it was thought to be an abnormality secondary to aging that led to elongation and twisting of a submucosal artery, aneurysms, atherosclerosis, arteritis and/or inflammation. However, it is currently believed that the Dieulafoy's lesion may be a congenital vascular malformation. (1, 6) These patients present acute, massive and sometimes recurrent hemorrhaging. The most frequent symptoms are massive hematemesis, melena, and hematochezia without abdominal pain. (Figure 5).
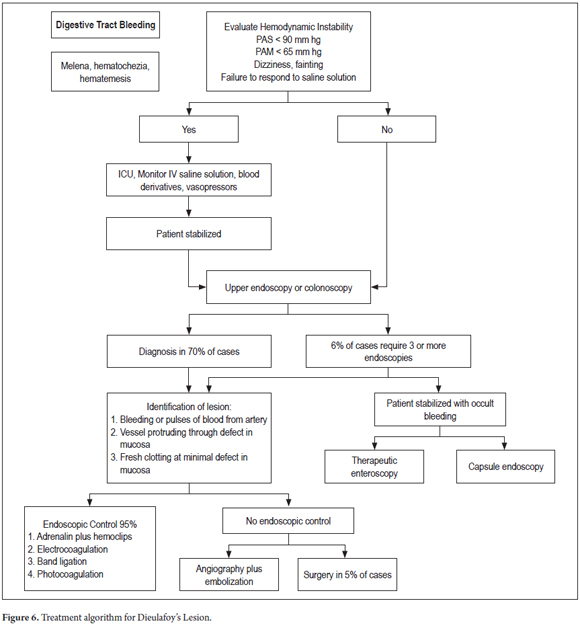
Even though the initial endoscopy is effective for diagnosis of up to 70% of the patients, several endoscopies may be required. About 6% of these patients require three or more endoscopies to establish a diagnosis. (1) Failure to make the diagnosis during the initial endoscopy may be due to excessive blood, clots, and/or subtle lesions. The endoscopic criteria proposed for diagnosis of DL are:
- Active or pulsing arterial bleeding from a minimal defect of the mucosa with normal surrounding mucosa.
- Endoscopic sighting of a vessel that protrudes, with or without active bleeding, through a minimal defect of the mucosa or through surrounding normal mucosa.
- Fresh clotting, adhering at a narrow point of attachment to a minimal defect of the mucosa or to mucosa of normal appearance. (7)
When the lesion has not been located, enteroscopy will allow evaluation of the small intestine up to a distance of 150 cm from the pylorus. This achieves diagnosis in 70% to 100% of patients with occult gastrointestinal bleeding. (8) Successful location of Dieulafoy's lesion has also been achieved with capsule endoscopy which has the advantage of being minimally invasive, but has the disadvantage of not allowing intervention. (1) In patients with DL, endoscopic management, which has success rates of up to 95%, has become the standard for treatment. (9) Although various endoscopic techniques are frequently used, the most frequently used is an injection of adrenaline solution. This can be done on its own as a single therapy or in combination with another modality. (2) Other endoscopic hemostatic techniques used are electrocoagulation, laser photocoagulation, sclerotherapy, hemoclips and band ligation.
With the use of electrocoagulation and thermo-coagulation methods, increased risk of transmural injury in thin-walled organs such as the duodenum has been reported. For this reason the use of hemoclips is suggested as a more effective and safer method of hemostasis.
Band ligation has also been reported to be an effective, safe and low cost solution for the treatment of DL. (2)
A study of 24 patients by Chung et al. compared the results of injection of hypertonic saline solution with those of mechanical therapy using either hemoclips or band ligation in order to determine the efficacy of these treatment methods. (10) The initial rate of bleeding control was higher in the group of patients treated with mechanical therapy, while the rate of rebleeding was significantly higher in the group treated with hypertonic saline.
Parkinson et al. have demonstrated that the use of hemoclips is a significantly more effective therapy for prevention of recurrent bleeding. (11) On the other hand, Karaahmet et al. suggest that the endoscopic combination of adrenaline injection and mechanical therapies is superior to monotherapy for treatment of DL. (12) Angiography and embolization are indicated for patients with active bleeding who are not amenable to endoscopic and/or surgical treatment and for those whose DL is inaccessible or cannot be located. (13)
Finally, surgical resection is reserved for 5% of cases that are refractory to endoscopic management and angiographic methods. Figure 6 shows the algorithm for the study and treatment of the Dieulafoy's lesion.
CONCLUSION
Dieulafoy's lesions in the duodenum are uncommon pathologies that cause severe and recurrent hemorrhaging of the upper digestive tract. Appropriate early endoscopic diagnosis is essential. Although several effective endoscopic techniques are available for controlling bleeding, the combination of adrenaline injection therapy and mechanical therapy reduces the risk of rebleeding.
REFERENCES
1. Baxter M. Dieulafoys lesion: current trends in diagnosis and management. Ann R Coll Surg Engl. 2010;92(7):548–554 [ Links ]
2. Mohammed Ibrarullah and Gajanan D Wagholikar. Dieulafoys lesion of duodenum: a case report. BMC Gastroenterology. 2003,31(3):2. [ Links ]
3. Chaer R, Helton WS. Dieulafoys disease. Am Coll Surg. 2003;196:290–6. [ Links ]
4. McClave SA, Goldschmid S, Cunningham JT and Boyd WP Jr. Dieulafoys cirsoid aneurysm of the duodenum. Dig Dis Sci. 1988,33(7):801-805. [ Links ]
5. Norton ID, Petersen BT, Sorbi D, Balm RK, Alexander GL and Gostout CJ. Management and long-term prognosis of Dieulafoy lesion. Gastrointest Endosc. 1999, 50(6):762-767 [ Links ]
6. Dincer Avlan, Ali Nayci, Engin Altintas. An unusual cause for massive upper gastrointestinal bleeding in children: Dieulafoys lesion. Pediatr Surg Int. 2005;21(5):417–418. [ Links ]
7. Dy NM, Gostout CJ and Balm RK. Bleeding from the endoscopically-identified Dieulafoy lesion of the proximal small intestine and colon. Am J Gastroenterol. 1995;90(1):108-111. [ Links ]
8. Al-Mishlab T, Amin AM and Ellul JM. Dieulafoys lesion: an obscure cause of GI bleeding. J R Coll Surg Edinb. 1999;44(4):222-225. [ Links ]
9. Sone Y, Kumada T, Toyoda H, et al. Endoscopic management and follow up of Dieulafoy lesion in the upper gastrointestinal tract. Endoscopy. 2005;37(5):449-53. [ Links ]
10. Chung IK, Kim EJ, Lee MS, et al. Bleeding Dieulafoys lesions and the choice of endoscopic method: comparing he hemostatic efficacy of mechanical and injection methods. Gastrointest Endosc. 2000;52(6):721–4. [ Links ]
11. Park CH, Joo YE, Kim HS, Choi SK, Rew JS, Kim SJ. A prospective, randomized trial of endoscopic band ligation versus endoscopic hemoclip placement for bleeding gastric Dieulafoys lesions. Endoscopy. 2004;36(8):677-81. [ Links ]
12. Karaahmet Fatih, Kılıncalp S, Coskun. The efficiency of endoclips in maintaining the gastrointestinal bleeding-related Dieulafoys lesion. 2015;9. [ Links ]
13. Alomari A, Fox V, Kamin D. Embolization of a bleeding Dieulafoy lesion of the duodenum in a child. Case report and review of the Literature. Journal of Pediatric Surgery. 2013; 48(1):e39-41. [ Links ]











 texto em
texto em 


